
Anaplastic lymphoma kinase-positive anaplastic large-cell lymphoma with primary bone involvement: a case report
Highlight box
Key findings
• We describe a case of anaplastic lymphoma kinase positive (ALK+) anaplastic large-cell lymphoma (ALCL) patient with primary multiple bone lesions. After receiving multiple cycles of chemotherapy, local bone radiotherapy and denosumab treatment, the patient’s bone pain and osteolytic lesions were improved.
What is known and what is new?
• Few case reports of ALCL originating in bone have been reported. Unlike conventional involvement of lymph nodes, the clinical significance of ALK expression in ALCL with primary bone injury is not clear.
• The treatment of denosumab has helped improve patients’ bone pain and osteolytic lesions.
What is the implication, and what should change now?
• ALK+ ALCL originating primarily in the bone may be easily misdiagnosed and hence require appropriate evaluation in the upfront setting. In consideration of the lack of relevant experience due to the rarity of the disease, choosing a suitable treatment regimen requires comprehensive consideration.
Introduction
Lymphomas originating in extranodal sites are uncommon, and lymphomas originating in bone are even rarer. Lymphomas originating in bone but not involving visceral or regional lymph nodes are diagnosed as primary bone lymphoma (PBL), accounting for 4–5% of extranodal lymphomas (1). Most PBLs are primary diffuse large B-cell lymphoma of bone (PBDLBCL) (1,2). Few case reports of anaplastic large-cell lymphoma (ALCL) originating in bone have been reported (3).
ALCL is a unique clinicopathological type of non-Hodgkin’s lymphoma (NHL), accounting for about 3% of all adult NHLs. Anaplastic lymphoma kinase (ALK) is associated with NPM-ALK t(2;5) translocation, which was first found in ALCL cells in 1994. The influence of ALK expression on the prognosis of ALCL patients with primary bone lesions remains controversial (4-8). As this disease is rare and the lack of standard treatment, more relevant studies and case reports are needed.
Herein, we describe a case of ALK-positive (ALK+) ALCL patient with primary multiple bone lesions. The patient received multiple cycles of chemotherapy, sequential local bone radiotherapy and anti-bone absorption treatment. At present, regular follow-up shows that the patient’s bone pain has been controlled and there is no sign of recurrence. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-80/rc).
Case presentation
A 47-year-old Chinese man visited a local hospital with a 1-month history of lumbosacral part and left chest pain. A monoclonal M-protein is detected in peripheral blood by immunofixation. Bone marrow biopsy was completed and about 1.5% immature plasma cells were found by cytologic analyses. Flow cytometry analysis revealed a tiny amount of abnormal monoclonal plasma cells, and the result of fluorescence in situ hybridization was notable for t(11;14). The result of the positron emission tomography-computed tomography (PET-CT) examination revealed multiple osteolytic lesions. The scattered osteolytic lesions were identified as hypermetabolic lesions, including the second rib on the left, the ninth thoracic vertebra, bilateral iliac bones, the left mass of the sacral vertebra, and the bone of the upper femur on the right. The results showed increased uptake of the 18F-fludeoxyglucose (FDG) with bone cortex not bone marrow and highly suggested a malignant disease, indicating multiple myeloma involvement. At the same time, no abnormal metabolism was found in lymph nodes or extranodal sites (such as lung, liver, spleen and so on). Before starting treatment, hepatitis B surface antigen (HBsAg) was detected positive in the patient’s peripheral blood, antiviral treatment was started immediately. To relieve the pain, the patient immediately received two cycles of bortezomib, lenalidomide, and dexamethasone (VRD) chemotherapy. Contrary to what was supposed, the patient’s pain was aggravated after treatment, and associated numbness and weakness occurred in the left leg. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
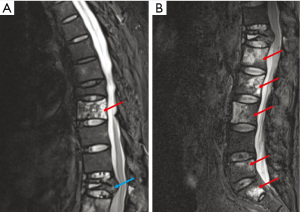
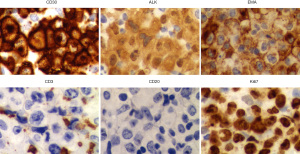
In July 2021, when admitted to our hospital, the patient was generally in stable condition without symptoms of anaemia, dyspnoea or fever. Physical examination revealed multiple pain in the whole body and restricted movement of the left leg. Upon review of the family history of the patient, no special medical history was found. After completing the hematology examination, complete blood count, serum calcium, and creatinine were revealed within normal range, Epstein-Barr virus (EBV) was undetectable. At the same time, the levels of some tumor markers, such as carcinoembryonic antigen, glycan antigen 125, neuron-specific enolase, and prostate-specific antigen, were also detected within normal ranges. Magnetic resonance imaging (MRI) showed tumor infiltration in thoracic vertebrae, lumbar vertebrae, sacrum, right iliac bone and left piriformis muscle, compression fracture of T8 centrum, swelling of lumbar dorsal and paravertebral soft tissues (Figure 1). Based on the poor effect of early treatment and after discussion with the patient and his family, the patient finally agreed to accept the biopsy of the T10 and L2 vertebral bodies. The results of immunohistochemical analysis of pathology showed that a strong positive for CD30, epithelial membrane antigen (EMA), CD38 and MUM1, a positive cytoplasmic and nuclear pattern for ALK, whereas CD3, CD4, CD8 and CD20 were negative. And the Ki67 index was almost 80% (Figure 2). The patient was diagnosed as ALK+ ALCL stage IV with primary bone involvement.
The chemotherapy including cyclophosphamide, doxorubicin and prednisone (CHP) and anti-CD30 monoclonal antibody brentuximab vedotin (BV), were given at the first time. Unfortunately, after receiving three cycles of chemotherapy, the patient’s toes and feet developed a sock like abnormal feeling with obvious pain, which was considered as peripheral nerve damage. After symptomatic treatment, such as pain relief and neurotrophic therapy, the symptoms of patients improved slowly. Therefore, CHP regimen was adopted in the fourth cycle of chemotherapy. After these four courses of chemotherapy, the patient’s chest and waist pain symptoms were relatively relieved. Reexamination of MRI showed that the bone and muscle injuries were not aggravated, while more vertebral bodies had compression fractures. In order to improve the quality of life, the patient underwent posterolateral thoracic interbody fusion for compression fractures of thoracic.
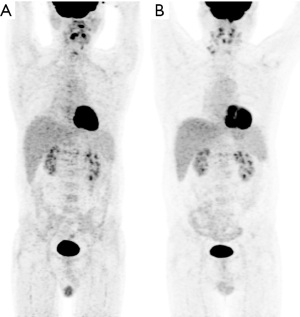
After the surgery, one more course of CHP regimen was given. Fortunately, the patient’s symptoms were more improved. Considering the high risk of overall prognostic index evaluation, the patient agreed to collect autologous stem cells as a reserve for possible consolidation autologous stem cell transplantation. Then two cycles of chemotherapy, including cyclophosphamide, mitoxantrone and prednisone, were given. The result of the second PET-CT examination indicated the multiple abnormal bone density shadows and postoperative changes of vertebral body, and no obvious metabolic abnormalities were observed (Figure 3A). Subsequently, the patient received local radiotherapy on thoracic T9 vertebral body and left sacral focus. In recent 1 year, the patient had a routine follow-up, including routine blood test, serum calcium, creatinine, HBsAg and hepatitis B virus (HBV)-DNA and MRI, and received denosumab treatment every month to prevent fractures. In February 2023, the recent PET-CT examination showed that the metabolism of thoracic T9 vertebral body and left sacrum was slightly lower than before (Figure 3B). The patient’s pain was controlled well and no fracture occurred again.
Discussion
Our manuscript introduced a patient diagnosed with ALK+ ALCL originating primarily in the bone, who received multiple cycles of chemotherapy with local bone radiotherapy, and his bone pain has been controlled. The patient is still in good condition under routine follow-up for about 1 year.
Lymphoma of bone origin is designated as PBL. Oberling first described PBL in 1928 (3). Each bone is a potential site for lymphoma development, most commonly in the diaphysis (1). In addition to pain and swelling in the involved site, pathological fracture is the more common clinical manifestation of PBL (4). However, it is difficult to diagnose PBL based on clinical manifestations and routine laboratory examination. X-ray plain film is difficult to estimate the extent of the disease. Computed tomography (CT) scanning and MRI can help to assess the disease stage and evaluate the involvement of bone and surrounding tissues. Moreover, PET-CT plays an important role in functional evaluation of bone lesions (4,9,10). The ALCL is an extremely uncommon histological subtype of PBL, and it is unclear whether the ALCL of primary bone has a worse prognosis than other types of PBL (3).
ALCL is a group of NHL with uncontrollable proliferation of abnormal T cells. In 2016, the World Health Organization (WHO) divided ALCL into four types: ALK+ ALCL, ALK-negative ALCL (ALK− ALCL), primary cutaneous ALCL (pcALCL) and breast implant-associated ALCL (BIA-ALCL) (11). PcALCL and BIA-ALCL are less aggressive and localized lymphomas, while ALK+ and ALK− ALCLs are aggressive systemic lymphomas. ALK, i.e., anaplastic lymphoma kinase, is a protein product of the ALK gene located on chromosome 2 and highly correlated with immunohistochemical identification of ALK protein (12).
ALK+ ALCL occurs mostly in children and young adults and is slightly more common in males. At the time of the initial visit, most patients present with advanced stage III–IV disease, usually accompanied by B symptoms (12). Extranodal sites often occur, including skin, soft tissue, bone, lung, liver, and bone marrow. ALK+ ALCL can be diagnosed according to histological and immunological examination. Cells with kidney or horseshoe shaped nuclei in the involved tissues are ALCL typical cells (13). Immunohistochemical results showed that cells in ALCL are usually CD30 positive, and the abnormal loss of universal T cell markers (CD3 and CD5) is also characteristic. At the same time, immunohistochemistry (IHC) shows variable positive for CD45, EMA, TIA-1, perforin, and granzyme B (3). ALK fusion protein is detected by fluorescence in situ hybridization. It should be noted that for ALCL originating from bone, due to decalcification of the specimen, it may not be possible to obtain sufficient signal (14).
Because of the rarity of this disease, most of the evidence for various treatment options in patients with systemic ALCL comes from a retrospective study of peripheral T-cell lymphoma (PTCL) (12). CHOP, including cyclophosphamide, doxorubicin, vincristine and prednisone, is the most commonly used initial treatment (12). Although the prognosis of systemic ALCL is more favourable than that of PTCL, the prognosis has hardly improved in the past 30 years, especially in patients with recurrence or relapse (R/R) ALCL. With the deepening of our understanding of the biology of systemic ALCL, more and more potential therapeutic targets and chemotherapy schemes are being found and tested to improve the prognosis. BV is an antibody-drug conjugate medication and selectively targets tumor cells expressing the CD30 antigen, a defining marker of ALCL. The recent clinical results showed that the combination of BV plus CHP (A+CHP) had a better response rate and progression free survival rate in CD30 positive peripheral T lymphoma compared with CHOP (14). Therefore, A+CHP has been used for the first-line treatment of ALK+ ALCL in recent years. However, BV-induced peripheral neurotoxicity (BVIN) is a major reason for the limited clinical application of BV (15). Similar to the symptom of peripheral nerve involvement caused by the use of vincristine, the most common form of BVIN is the symmetrical socking-glove pattern (15,16). Although reversible to a large extent, BVIN may last for months or years after treatment, which may have a negative impact on the quality of life and work life of patients. At present, only strategy of BVIN includes dose adjustments and treatment discontinuation. Meanwhile, the latest clinical research data support the consideration of consolidative stem cell transplantation in CD30 positive PTCL patients after obtaining complete response (CR) (12,17). In addition to chemotherapy and targeted therapy, radiotherapy is also used for ALCL with primary bone involvement. Considering the limitations of the treatment strategy, our patient was mobilized with stem cells before radiotherapy, and enough stem cells were collected as an alternative treatment. Unlike in conventional nodular ALCL, the significance of ALK+ in patients with primary bone ALCL has not been clearly determined (5,6).
As used in many other bone malignancies, PBL patients should also pay more attention to bone health preventive measures. In the case of risk factors of osteoporosis, pathological fracture and other related complications, anti-bone absorption drugs should be given as early as possible (18). Denosumab is a receptor activator of nuclear factor kappa-Β ligand inhibitor, retaining bone mass by inhibiting the bone absorption process (19). It is generally recommended for postmenopausal women with a high risk of fractures and men for long-term prevention of fractures. Moreover, denosumab has also proved effective in patients receiving anti-tumor therapy. Similar to bisphosphonate, denosumab has a promising additional role in reducing bone injury pain. After the combined treatment of chemotherapy and denosumab, our patient’s bone pain and osteolytic lesions have been improved to a certain extent.
In our case, the patient was initially misdiagnosed as multiple myeloma. Vertebral body biopsy helped us to make the correct diagnosis. In contrast to other cases, the patient was treated not only with chemotherapy and local radiotherapy but also denosumab treatment. Meanwhile, sufficient stem cells were collected as a possible consolidation of autologous stem cell transplantation. Fortunately, the patient’s bone pain has been controlled and he is generally in good condition.
Conclusions
In summary, we describe a case of primary multiple bone injury in an ALK+ ALCL patient. It should be noted that, unlike conventional involvement of lymph nodes, the clinical significance of ALK expression in ALCL with primary bone injury needs further study. After receiving multiple cycles of chemotherapy, continuous local bone radiotherapy and denosumab treatment, the patient’s bone pain and osteolytic lesions were improved. Regular follow-up shows that the patient is generally in good condition. We will continue to follow up the report of ALCL originating in bone. Relevant cases will be further studied to better summarize treatment experience.
Acknowledgments
We owe thanks to the patient.
Funding: This work was supported in part by the Natural Science Foundation of Hubei Province (No. 2019CFB656 to L.J.) and the Youth Science Fund Project of National Natural Science Foundation (NNSF) of China (No. 82100138 to L.C.).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-80/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-80/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-80/coif). L.C. received funding from Youth Science Fund Project of National Natural Science Foundation of China (No. 82100138). L.J. received funding from receives funding from Natural Science Foundation of Hubei Province (No. 2019CFB656). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mikhaeel NG. Primary bone lymphoma. Clin Oncol (R Coll Radiol) 2012;24:366-70. [Crossref] [PubMed]
- Noh BJ, Han CS, Park JS, et al. ALK-positive anaplastic large-cell lymphoma with primary bone involvement: A rare case and review of the literature. Malays J Pathol 2018;40:161-7. [PubMed]
- Bhagavathi S, Fu K. Primary lymphoma of bone: a review. Semin Diagn Pathol 2014;31:48-52. [Crossref] [PubMed]
- Zheng W, Yin QQ, Hui TC, et al. Primary bone anaplastic lymphoma kinase positive anaplastic large-cell lymphoma: A case report and review of the literature. World J Clin Cases 2021;9:3403-10. [Crossref] [PubMed]
- Al-Asaadi Z, Fatin S, Patel K, et al. Anaplastic large cell lymphoma with axial skeletal lesions portends a poor prognosis. Br J Hosp Med (Lond) 2015;76:606-7. [Crossref] [PubMed]
- Nagasaka T, Nakamura S, Medeiros LJ, et al. Anaplastic large cell lymphomas presented as bone lesions: a clinicopathologic study of six cases and review of the literature. Mod Pathol 2000;13:1143-9. [Crossref] [PubMed]
- Nayak HK, Nishant R, Sinha NK, et al. Anaplastic large T-cell lymphoma presenting as an isolated osseous involvement: a case report and review of the literature. BMJ Case Rep 2013;2013:bcr2013009308. [Crossref] [PubMed]
- Kim KH, Jung YH, Han CW, et al. A case of Primary Bone Anaplastic Large Cell Lymphoma. Am J Case Rep 2016;17:734-8. [Crossref] [PubMed]
- Moog F, Kotzerke J, Reske SN. FDG PET can replace bone scintigraphy in primary staging of malignant lymphoma. J Nucl Med 1999;40:1407-13. [PubMed]
- Tutaeva VV, Ovsiannikova MR, Bobin AN, et al. Anaplastic large cell lymphoma ALK-positive variant of primary bone lymphoma associated with melanoma. Oxf Med Case Reports 2023;2023:omad025. [Crossref] [PubMed]
- Swerdlow SH, Campo E, Harris NL, et al. editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. Lyon, France: International Agency for Research on Cancer; 2017:2
- Hapgood G, Savage KJ. The biology and management of systemic anaplastic large cell lymphoma. Blood 2015;126:17-25. [Crossref] [PubMed]
- Santini-Araujo E, Kalil RK, Bertoni F, et al. Tumors and Tumor-Like Lesions of Bone. Verlag, London, UK: Spinger; 2015:385-411.
- Horwitz S, O'Connor OA, Pro B, et al. The ECHELON-2 Trial: 5-year results of a randomized, phase III study of brentuximab vedotin with chemotherapy for CD30-positive peripheral T-cell lymphoma. Ann Oncol 2022;33:288-98. [Crossref] [PubMed]
- Velasco R, Domingo-Domenech E, Sureda A. Brentuximab-Induced Peripheral Neurotoxicity: A Multidisciplinary Approach to Manage an Emerging Challenge in Hodgkin Lymphoma Therapy. Cancers (Basel) 2021;13:6125. [Crossref] [PubMed]
- Li T, Timmins HC, Lazarus HM, et al. Peripheral neuropathy in hematologic malignancies - Past, present and future. Blood Rev 2020;43:100653. [Crossref] [PubMed]
- Savage KJ, Horwitz SM, Advani R, et al. Role of stem cell transplant in CD30+ PTCL following frontline brentuximab vedotin plus CHP or CHOP in ECHELON-2. Blood Adv 2022;6:5550-5. [Crossref] [PubMed]
- Messina C, Christie D, Zucca E, et al. Primary and secondary bone lymphomas. Cancer Treat Rev 2015;41:235-46. [Crossref] [PubMed]
- Pang KL, Low NY, Chin KY. A Review on the Role of Denosumab in Fracture Prevention. Drug Des Devel Ther 2020;14:4029-51. [Crossref] [PubMed]
Cite this article as: Cheng L, Huang M, Chen X, Jiang L. Anaplastic lymphoma kinase-positive anaplastic large-cell lymphoma with primary bone involvement: a case report. AME Case Rep 2024;8:19.


