Successful one-lung ventilation in a patient after laryngectomy by inserting a long spiral single-lumen tube into the left main bronchus: a case report
Highlight box
Key findings
• Using a long spiral single-lumen tube (SLT) provided stable one-lung ventilation in a patient after laryngectomy with voice prosthesis (VP).
• A long spiral endotracheal tube affords the flexibility to allow atraumatic placement through a contracted tracheostoma.
What is known and what is new?
• Patients who have had laryngectomy require thorough preoperative assessment, the potential for stomal stenosis and an action plan for possible VP displacement must be considered.
• A long spiral SLT might be an option for one-lung ventilation in patients after laryngectomy with a tracheoesophageal VP.
What is the implication, and what should change now?
• Patients with a tracheostoma and implantation of a tracheoesophageal VP require careful selection and placement of the appropriate airway device for one-lung ventilation.
Introduction
In the airway management of patients who have previously undergone total laryngectomy, the size of the permanent tracheal stoma and implantation of a tracheoesophageal voice prosthesis (VP) make the airway management and choice of an appropriate endotracheal tube difficult (1-3). Herein, we report the airway management for lung cancer surgery in a patient with a VP following total laryngectomy, using lung isolation techniques that were achieved with a long spiral single-lumen tube (SLT). We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-108/rc).
Case presentation
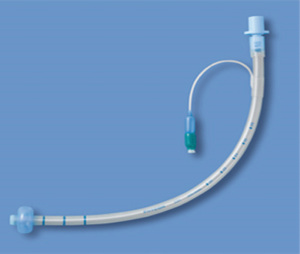
A 66-year-old man (169 cm, 57 kg) with Parkinson’s disease had a medical history of right supraglottic laryngeal cancer, for which he underwent total laryngectomy. At that time, the patient had difficulty inserting a cuffed tracheostomy tube [7 mm inner diameter (ID), 10 mm outer diameter (OD)]. A VP (Provox Vega, Atos Medical, Sweden, 20 Fr, 12.5 mm) was inserted into the tracheoesophageal fistula (Figure 1). At his current presentation, segmentectomy combined with lymph node dissection was scheduled for a 11 mm malignant nodule in the apical segment of the right lung.
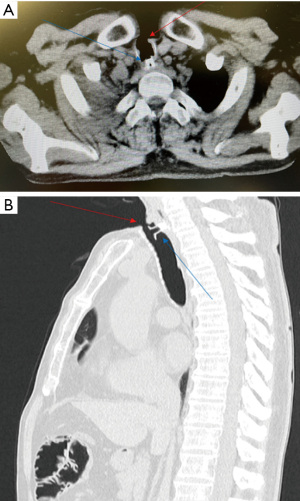
After intravenous cannula placement, epidural anesthesia was performed at the thoracic T5/6 level. General anesthesia was induced with propofol at a target concentration of 3.0 µg/mL with remifentanil 0.3 µg/kg/min and rocuronium 40 mg. Although we had originally planned to insert a silicone double-lumen endotracheal tube (DLT) (Phycon 33 Fr, 11 mm OD, Fuji Systems, Japan) through the permanent tracheostoma, this plan was abandoned because the diameter of the stoma was narrower than 9 mm, which could have led to the VP being dislodged, along with airway injury. Therefore, we elected to use a long, cuffed, spiral SLT (Phycon wire-reinforced endotracheal tube long type defender with cuff, 6 mm ID, 8.7 mm OD, 400 mm in length, Fuji Systems, Japan) under the guidance of a 4 mm bronchoscope (Figure 2). Bronchoscopic observation of the trachea from the stoma revealed the VP below it. The tube was advanced carefully under bronchoscopic guidance, and was placed into the left main bronchus and secured in place (Figure 3). Adhesive tape was used to secure the tube. After placement of an arterial cannula in the left radial artery, the patient was turned to the left lateral position for the surgery. During the surgery, remifentanil 0.1–0.2 µg/kg/min and propofol 1.8 µg/mL were administered to maintain anesthesia with phenylephrine administration as needed, for management of hypotension. One-lung ventilation (OLV) was maintained for 146 minutes, with pressure-controlled ventilation with a driving pressure of 25 cmH2O and an inspired oxygen fraction of 1.0. Although peripheral capillary oxygen saturation decreased to 82% during the surgery because the tube accidentally slipped deeper into the left lower lobe due to the surgeon’s manipulations, the tube position was immediately adjusted using bronchoscopy, with recovery of oxygen saturation. Thoracotomy with a 150 mm long posterolateral incision in the fifth intercostal space allowed adequate gradual collapse of the lung. When bilateral ventilation was required, such as during the air leakage test, the tube was withdrawn above the carinal bifurcation and the tube cuff was deflated. Although slight air leakage via the narrow stoma remained, the right lung was gradually inflated to complete the leak test. After the surgery, we observed integrity of the mucosa and correct positioning of the VP by bronchoscopy. The VP was correctly functioning. Postoperatively, the patient was transferred to an intensive care unit and was discharged in an ambulatory condition on postoperative day 7.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Over the past 5 years, 10 of 3,480 patients requiring OLV in our hospital had a laryngectomy. Among them, one had a long spiral SLT, a Phycon left-sided DLT was used in 7 (35 Fr n=3, 37 Fr n=4), a Blue-line left-sided DLT (37 Fr, Smiths Medical, San Clemente, CA, USA) and Broncocath left-sided DLT (37 Fr, Medtronic, Minneapolis, MN, USA) used in the remaining two patients. The combination of a SLT and bronchial blocker or a tracheostomy DLT was not used in any of the patients. In terms of endotracheal tube selection, a left-sided tracheostomy DLT (Rüsch, 39 Fr, Teleflex, Wayne, PA, USA) can be used when the diameter of the tracheostoma is equal to or greater than 13 mm, although a right-sided tracheostomy DLT is not available in Japan (2,3). Of note, since a left-sided tracheostomy DLT cannot be used for left pneumonectomy or left main bronchotomy, other tubes should be selected (4). Furthermore, in Japan, since the average OD of the tracheal cannula used after tracheostomy is mostly 12–13 mm for men and 10–11 mm for women, use of a tracheostomy DLT appears to be very infrequent (5). When the tracheostoma size is equal to or less than 13 mm, insertion of an oral DLT or a combination of a tracheal cannula/SLT and bronchial blocker or SLT alone allows the performance of OLV (Figure 4) (6,7). However, with the combination of a tracheal cannula/SLT and bronchial blocker, the establishment of OLV is likely to take time because a blocker sometimes interferes with bronchoscopy (8). In addition, since the lung collapses relatively slowly, the combination might not be suitable for patients who undergo thoracic surgery in which alternate lung collapse and ventilation are required frequently. If the tracheostomy stoma size is large enough for insertion of an oral DLT, the use of the oral DLT might make the establishment of lung isolation easy (7). However, since it has been reported that DLTs increase the risk of airway injury, it is important to select a silicone DLT that has little effect on the airway mucosa (8-10). According to a report by Campos et al., among methods for OLV, DLTs were used least frequently as compared to other methods in patients with a tracheostoma (11). Since the tracheal diameter of Americans is reportedly bigger than that of Japanese, even use of a SLT/Shiley tracheal cannula in combination with a bronchial blocker allows easy establishment of OLV in American patients, but this would not be true in Japanese patients (5,12).
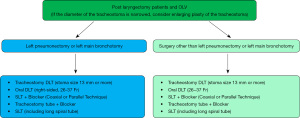
In our case, following total laryngectomy, a cuffed tracheostomy cannula was initially inserted through the tracheostoma, although the stoma subsequently contracted to diameter of 9 mm over time. Therefore, it was difficult to use the oral or tracheostomy DLT. While using the Univent tube (Teleflex, Wayne, PA, USA) might provide stable OLV, it could not be used in this case since the minimum OD of that tube is 9.7 mm for adult patients. Instead, we successfully established lung isolation by inserting a long spiral SLT into the left main bronchus under the guidance of a 4 mm bronchoscope. Further, the risk of tracheal mucosal injury was reduced because of the flexibility afforded by the wire reinforced and round shape of the tip of the long spiral SLT, compared with a standard DLT and an ordinary spiral SLT (4). In addition, the cuff of the tube is much shorter than the conventional one, and this shorter length may be useful when placed in the right main bronchus, where the margin of placement is less than in the left main bronchus (4,13). In order to address the stenosis condition, an enlarging plasty of the tracheostoma might be an option. However, the risk of infection of the tracheostoma need to be considered.
It is estimated that 5% to 8% of patients with primary lung cancer suffer from pharyngeal cancer, particularly in the vicinity of the epiglottis (1). Prior to lung cancer surgery, many of these patients are likely to undergo surgery or radiotherapy in the airway and neck region. These patients might subsequently need airway management through the permanent tracheostoma, which makes it difficult to achieve OLV. VPs are often offered to patients after laryngectomy. Between 70–90% of patients who have a VP can achieve speech (14). Of the 10 patients who underwent OLV after laryngectomy at our hospital, five (50%) had a VP. VPs have an internal unidirectional valve, which prevents aspiration from the esophagus to the airway, while simultaneously allowing exhalation through the mouth (14). The occurrence of prosthesis aspiration is 3.9–6.7% of patients (15). If the VP is accidentally dislodged, in order to maintain patency of the fistula until another prosthesis is fitted, a Fogarty catheter might be necessary to prevent the loss of the tracheoesophageal fistulous tract and entry of esophagogastric contents into the airway (16). In our case, since bronchoscopic observation revealed the VP under the permanent tracheostoma, we inserted the tube carefully so as not to interfere with it. If the VP had fallen into the trachea, its location would have had to be precisely determined. Since several reports have discussed the difficulty of accurately locating the VP using chest X-rays alone, a computed tomography scan is often performed to identify its location (15,17). Combined use of a flexible bronchoscope, forceps, and a retrieval basket is effective for removing the dislodged VP (18). In addition, if the VP falls into the esophagus, leading to complications such as intestinal obstruction, surgical treatment is sometimes required (19). Some types of VPs can be taped or stitched to the skin prior to airway manipulation in laryngectomy patients (20).
Our case report is limited to the presentation of a single patient because it is rare for post-laryngectomy patients with contracture of the stoma and VP to undergo surgery requiring OLV.
Conclusions
In the present case, lung cancer surgery was successfully completed with the use of a long spiral SLT for establishment of OLV in our patient with a VP, since a DLT was unusable because the permanent tracheostoma had contracted after total laryngectomy. When lung isolation techniques need to be performed in total laryngectomy patients, it is important to assess the size of the tracheostoma, check for the presence of a VP, select the appropriate tube size for the tracheostoma, insert the tube carefully, and be prepared to deal with the eventuality of dislodgement of the VP.
Acknowledgments
The authors thank and respect the patient and the staff of the Juntendo Hospital operating room.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-108/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-108/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-108/coif). I.K. serves as an unpaid editorial board member of AME Case Reports from May 2023 to April 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol 2010;23:12-7. [Crossref] [PubMed]
- Masamune T, Matsukawa T, Ookawa I, et al. Double-lumen tracheostomy tube (Tracheopart) used in two patients for one-lung ventilation under general anesthesia. Masui 2004;53:1418-20. [PubMed]
- Dincq AS, Lessire S, Mayné A, et al. Double-lumen tubes for tracheostomized patients. J Cardiothorac Vasc Anesth 2015;29:e35-6. [Crossref] [PubMed]
- Pedoto A. How to choose the double-lumen tube size and side: the eternal debate. Anesthesiol Clin 2012;30:671-81. [Crossref] [PubMed]
- Miyamoto M, Saito K, Nakagawa H. Morphometric Analysis of Tracheal Rings using Ultra—high Resolution Computed Tomography in Japanese Adults. Nippon Jibiinkoka Tokeibugeka Gakkai Kaiho (Tokyo) 2023;126:200-7. [Crossref]
- Collins SR, Titus BJ, Campos JH, et al. Lung Isolation in the Patient With a Difficult Airway. Anesth Analg 2018;126:1968-78. [Crossref] [PubMed]
- Letal M, Theam M. Paediatric lung isolation. BJA Education 2017;17:57-62. [Crossref]
- Clayton-Smith A, Bennett K, Alston RP, et al. A Comparison of the Efficacy and Adverse Effects of Double-Lumen Endobronchial Tubes and Bronchial Blockers in Thoracic Surgery: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J Cardiothorac Vasc Anesth 2015;29:955-66. [Crossref] [PubMed]
- Knoll H, Ziegeler S, Schreiber JU, et al. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology 2006;105:471-7. [Crossref] [PubMed]
- Kang S, Chae YJ, Kim DH, et al. Comparison of fiberoptic bronchoscopic intubation using silicone and polyvinyl chloride double-lumen tubes. Korean J Anesthesiol 2023;76:300-6. [Crossref] [PubMed]
- Campos JH, Musselman ED, Hanada S, et al. Lung Isolation Techniques in Patients With Early-Stage or Long-Term Tracheostomy: A Case Series Report of 70 Cases and Recommendations. J Cardiothorac Vasc Anesth 2019;33:433-9. [Crossref] [PubMed]
- D'Anza B, Knight J, Greene JS. Does body mass index predict tracheal airway size? Laryngoscope 2015;125:1093-7. [Crossref] [PubMed]
- Slinger P. Sleeve pneumonectomy. J Cardiothorac Vasc Anesth 2009;23:269-70. [Crossref] [PubMed]
- Terada T, Saeki N, Toh K, et al. Voice rehabilitation with Provox2 voice prosthesis following total laryngectomy for laryngeal and hypopharyngeal carcinoma. Auris Nasus Larynx 2007;34:65-71. [Crossref] [PubMed]
- Conte SC, De Nardi E, Conte F, et al. Aspiration of tracheoesophageal prosthesis in a laryngectomized patient. Multidiscip Respir Med 2012;7:25. [Crossref] [PubMed]
- Rao Kadam V, Lambert P, Pant H, et al. 'Speaking valve' aspiration in a laryngectomy patient. Anaesth Intensive Care 2010;38:197-200. [Crossref] [PubMed]
- Dewan K, Erman A, Long JL, et al. Assessment and Retrieval of Aspirated Tracheoesophageal Prosthesis in the Ambulatory Setting. Case Rep Otolaryngol 2018;2018:9369602. [Crossref] [PubMed]
- Abia-Trujillo D, Tatari MM, Venegas-Borsellino CP, et al. Misplaced tracheoesophageal voice prosthesis: A case of foreign body aspiration. Am J Emerg Med 2021;41:266.e1-2. [Crossref] [PubMed]
- Hiltmann O, Buntrock M, Hagen R. Mechanical ileus caused by a Provox voice prosthesis -- an "iatrogenic" enteral complication in voice prosthesis rehabilitation of laryngectomees. Laryngorhinootologie 2002;81:890-3. [Crossref] [PubMed]
- Kress P, Schäfer P, Schwerdtfeger FP, et al. Are modern voice prostheses better? A lifetime comparison of 749 voice prostheses. Eur Arch Otorhinolaryngol 2014;271:133-40. [Crossref] [PubMed]
Cite this article as: Imai E, Fukuda M, Kochiyama T, Yamaguchi A, Sugasawa Y, Hayashida M, Kawagoe I. Successful one-lung ventilation in a patient after laryngectomy by inserting a long spiral single-lumen tube into the left main bronchus: a case report. AME Case Rep 2024;8:16.