
Severe subglottic stenosis after resection of anterior mediastinal tumor using a double‑lumen tube: a case report
Highlight box
Key findings
• This report demonstrated leading up to the onset and subsequent recovery of subglottic stenosis.
What is known and what is new?
• Airway obstruction owing to subglottic stenosis may occur several days post-surgery with a double‑lumen tube (DLT). However, reports of subglottic stenosis among patients who underwent surgery involving the DLT have been limited.
• We documented reports on the course from the immediate postoperative period to the onset of subglottic stenosis and recovery in detail.
What is the implication, and what should change now?
• We suggest that tracheostomy is effective and should be performed in patients with worsening subglottic stenosis and that prompt treatment before the development of complete obstruction will result in the alleviation of the stenosis.
Introduction
Double-lumen tubes (DLTs) are commonly used for differential pulmonary ventilation during thoracic surgery. Few reports exist on subglottic stenosis among patients who underwent surgery involving DLTs (1-3). Progressive subglottic stenosis is a fatal complication leading to asphyxia. However, we lack immediate postoperative period documentation leading up to the onset and subsequent recovery of subglottic stenosis.
Herein, we present a case of a 75-year-old woman successfully treated for subglottic stenosis after DLT. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-92/rc).
Case presentation
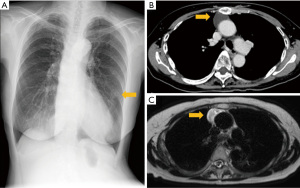
A 75-year-old woman presented to our hospital with an abnormal chest shadow, which was identified during a medical examination (Figure 1A). She had a history of dyslipidemia and nontuberculous mycobacteriosis. Chest computed tomography (CT) revealed an inflammatory nodule in the lingula and an anterior mediastinal mass with a poor contrast effect measuring 6.0 cm × 3.1 cm × 1.9 cm (Figure 1B), which grew from 2.2 to 6.0 cm over 21 months. Low and high signals were detected on T1- and T2-weighted thoracic magnetic resonance imaging, respectively (Figure 1C). Concordantly, a thymic cyst was suspected. Since the tumor doubled in size within a short period, resection was performed. At the time of surgery, the patient was 161 cm tall and weighed 51 kg. Physical examination was unremarkable and no airway abnormalities, such as hoarseness, were observed. Tracheal diameter was 13.8 mm measured by CT.
The patient underwent robotic-assisted thoracoscopic resection via the right lateral approach. General anesthesia was administered with the patient in the supine position. A 35-Fr left-sided DLT (Parker Double-Lumen Endo-Bronchial Tubes, Japan Medicalnext Co., Ltd., Osaka, Japan) was used for intubation and differential lung ventilation (deflated right lung). Intubation was complicated owing to the patient’s narrow glottis, however, DLT barely passed through the glottis in one attempt. The surgical operating time was 1 h 28 min; the anesthesia time was 2 h 46 min. The patient was extubated in the operating room after the end of surgical procedure. No intraoperative complications were observed. Hoarseness and stridor were observed on postoperative day (POD) 1, which was initially attributed to the intubation. Patient’s percutaneous oxygen saturation (SpO2) was 97% and respiratory status was stable, with a nasal cannula set at 1 L/min oxygen flow rate. Laryngoscopy showed submucosal hemorrhage around the vocal cords and mild subglottic stenosis just below the glottis; however, there was no arytenoid dislocation or findings necessitating emergency treatment (Figure 2A).
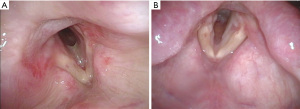
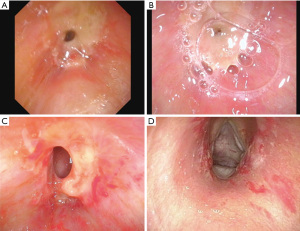
On POD 4, her SpO2 was 97% on room air and the hoarseness had improved. However, her stridor became more severe and laryngoscopy was re-performed and revealed subglottic stenosis progression prompting emergency tracheotomy (Figure 2B). The tracheotomy tube was used Mera Sofit D-7CFS (Senko Medical Instrument Mfg. Co., Ltd., Tokyo, Japan). Intravenous hydrocortisone sodium succinate (250 mg/day) and inhaled epinephrine (0.1 mg/day) were administered. On POD 5, subglottic stenosis progressed further (Figure 3A). By POD 7, observation of the glottis through the tracheostomy orifice revealed almost complete airway obstruction (Figure 3B). By POD 9, partially improving the subglottic stenosis (Figure 3C), thereafter the subglottic stenosis was almost completely alleviated by POD 12 (Figure 3D) (Figure S1A,S1B) and gradual improvement continued (Figure S1C). Hydrocortisone was discontinued on POD 14, and the tracheal cannula was removed on POD 22 (Figure S1D,S1E). Trachea-cutaneous fistula closure was performed on POD 35, and she was discharged on POD 42, remaining well (Figure S1F-S1H). The pathological examination of the anterior mediastinal tumor confirmed the diagnosis of thymic cyst. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Reports on subglottic stenosis after thoracic surgery using DLT are limited (1-3); however, similarities were observed between previous cases and the present one. These included significant resistance while passing through the glottis during intubation, worsening stridor noted on the first POD, emergency airway treatment required on POD 4 and improvement of the subglottic stenosis by PODs 10–14. This sequence of events was possibly caused by the large tube size damaging the tracheal mucosa, as in previous reports (1-3). DLTs have a larger outer diameter than the standard tracheal tubes; making appropriate size selection challenging. Despite previous attempts to identify the appropriate DLT size through various factors, such as patient height, weight, tracheal and left main bronchial diameters, and transverse diameters of the cricoid cartilages, established methods are lacking (4,5). In this case, we suspected that the DLT may have damaged the tracheal mucosa as a possible cause of subglottic stenosis. There were no systemic diseases that promote an inflammatory response, and the anesthesia time was not particularly long, lasting less than 3 hours. The instantaneous and powerful damage to the tracheal mucosa by the DLT rather than the intubation time may be the cause of sever subglottic stenosis. As a preventive measure of the stenosis, downsizing the DLT and using a bronchial blocker may have been considered. However, Takahashi et al. reported that subglottic stenosis occurred when the tube size was changed from 35 to 32 Fr, owing to resistance during intubation (3). It may be difficult to prevent subglottic stenosis completely by downsizing the DLT.
Since it is difficult to predict the onset of subglottic stenosis before surgery and more effective preventive measures have not been established, early intervention such as tracheostomy is crucial. Systemic administration of steroids and epinephrine inhalation have been used to treat subglottic stenosis. However, formal evidence is lacking and airway clearance via tracheotomy is likely necessary.
Conclusions
This case highlights the potential of subglottic stenosis following thoracic surgery using a DLT. Patients should be monitored for hoarseness and stridor, as airway obstruction secondary to subglottic stenosis may occur several days after surgery with a DLT. Tracheostomy is recommended for worsening subglottic stenosis and early intervention is crucial.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-92/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-92/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-92/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hayashi M, Kiyohashi M, Fuchibe M, et al. Late-onset Subglottic Stenosis after Extubation of a Double Lumen Tube. J Jpn Soc Clin Anesth 2018;38:19-24. [Crossref]
- Yonei A, Moriyama H, Ichinari H. A Case of Severe Subglottic Stenosis on the 3 Day After Operation for Primary Lung Cancer - a Case Report. J Jpn Soc Resp Endoscopy. 2020;42:529-33.
- Takahashi R, Suzuki M. A case of subglottic stenosis developed after intubation of double-lumen tube. J Jpn Soc Head Neck Surg 2019;29:197-201. [Crossref]
- Ideris SS, Che Hassan MR, Abdul Rahman MR, et al. Selection of an appropriate left-sided double-lumen tube size for one-lung ventilation among Asians. Ann Card Anaesth 2017;20:28-32. [Crossref] [PubMed]
- Sato M, Kayashima K. Difficulty in inserting left double-lumen endobronchial tubes at the cricoid level in small-statured women: A retrospective study. Indian J Anaesth 2017;61:393-7. [Crossref] [PubMed]
Cite this article as: Oiwa H, Sugawara K, Morita S, Uebayashi A, Sakai H, Funai K, Ema T. Severe subglottic stenosis after resection of anterior mediastinal tumor using a double‑lumen tube: a case report. AME Case Rep 2024;8:14.


