
A case report of inadequately treated acute deep venous thrombus and venous stasis
Highlight box
Key findings
• The patient experienced an improvement in lower leg edema and in chronic venous stasis ulcers after treatment of the vessels with a series of thrombectomies.
What is known and what is new?
• Chronic venous stasis is not an uncommon condition seen in dermatology and outpatient clinics. The current standard of care treatments aims at preventing secondary infections and often chase complications rather than prevent them from the source.
• This manuscript details a case of a patient who regained function and increased quality of life after a thrombectomy of the occluded.
What is the implication, and what should change now?
• Patients that present with chronic venous insufficiency should be referred to interventional radiologists in addition to the current standard of care for treatment and investigation of the cause of the venous insufficiency. Infection rate decline and ulcer improvement could be seen.
Introduction
Venous stasis dermatitis, also known as stasis dermatitis, or stasis eczema, is a common skin condition that typically affects the lower extremities. Venous stasis dermatitis may occur when the veins start to function ineffectively—venous insufficiency—which can lead to a pooling of fluid within the legs.
Venous stasis syndrome manifests clinically and classically present as chronic leg edema, skin hyperpigmentation, and induration; and can lead to the development of a venous ulcer if untreated or underdiagnosed. In extreme cases, venous stasis complications can lead to the necessity of limb amputation.
The etiology of venous stasis is largely related to medical conditions that affect blood flow in the legs, including, but not limited to, deep vein thrombosis, post-surgical lack of ambulation, congestive heart failure, and neoplastic conditions.
The incidence of venous stasis is not uncommon and is a major health problem seen at an annual incidence of 76 per 100,000 (1). Stasis dermatitis has a prevalence of 6–7% in patients over 50 years of age, affecting a significant portion of the elderly population (2). Fifteen to 20 million people over 50 in the United States live with the disease, making it twice as prevalent as psoriasis and only slightly less prevalent than seborrheic dermatitis (3). It is a common pathology that presents to dermatology clinics where the standard of care conservative treatment will include compression stockings, wet dressings, and elevation of extremities in order to prevent secondary infections. Stasis dermatitis is, however, judged less desirable for dermatologic therapy as compared to skin conditions such as actinic keratoses, tinea pedis, contact dermatitis, and seborrheic dermatitis, demonstrating a poor correlation between patient complaints and physical exam findings. Thus, despite the prevalence of skin pathologies in this age group, their dermatologic needs are largely unfulfilled (4).
Here, we present a case of a venous stasis that is presenting secondary to chronic occlusion of the left common iliac vein and femoral vein due to a tilted and irretrievable IVC filter that was placed more than 5 years prior to presentation. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-39/rc).
Case presentation
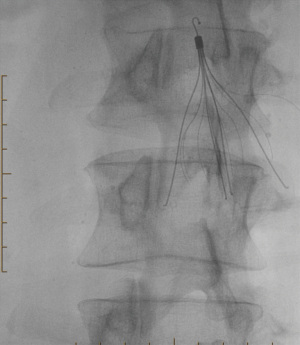
A 55-year-old Caucasian male presented to the outpatient Interventional Radiology clinic, IYA Medical in Scottsdale, Arizona, after a 10-year history of chronic venous stasis secondary to chronic occlusion of the left-common iliac vein and femoral vein. This presentation is believed to be secondary to a tilted and irretrievable IVC filter that tilted to an improper place and did not have proper follow-up due to the patient being incarcerated and becoming irretrievable leading to the case discussed in this case report. The original IVC filter was placed after the patient developed a popliteal clot secondary to an ankle trauma (Figure 1).
Upon presentation, the patient was unable to ambulate and had a greatly decreased quality of life. Physical examination was limited due to the patient being in severe pain. The lower extremity had thickened erythematous changes with an increased temperature and revealed ulceration (Figure 2) secondary to venous insufficiency.

After ruling out arterial involvement with a lower extremity magnetic resonance angiogram (MRA) and confirming venous involvement with magnetic resonance venogram (MRV), the patient was treated with a series of several thrombectomies and thrombolysis in an outpatient setting until restoration of the venous blood flow to the main venous system was achieved (Figures 3,4). The clots removed were massive and hemorrhagic in nature (Figure 5).



After treatment, the extreme swelling of the lower extremities has markedly decreased and the change can be visualized in the post-treatment images (Figures 6,7). The improved venous blood flow has reduced painful leg ulcers both in number and severity—which greatly reduces the patient’s likelihood of a secondary infection.
All procedures performed in this study were performed in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of written consent is available for review by the editorial office of this journal.
Discussion
The clinical presentation and progression of the disease in this patient are classic for chronic venous insufficiency. This presentation is consistent with an advanced case of chronic venous insufficiency that is treated conservatively in early disease states in most dermatology clinics by the standard of care. A multidisciplinary approach for these patients including primary care, dermatology, and interventional radiology among others can prevent the progression of the disease to a state that could necessitate amputation or other complications.
With treatment in an outpatient interventional radiology center with thrombectomy to achieve collateral venous blood flow, patient outcomes could improve markedly. This more aggressive interventional treatment improved the venous insufficiency, which corrected the abnormal blood flow in the venous system and resolved the lower extremity ulcers. This treatment can be an excellent approach for those with chronic venous insufficiency who also show dermatological abnormalities as well as a history or suspicion of central venous obstruction.
Conclusions
Venous stasis dermatitis is a common pathology that presents to dermatology clinics where the standard of care conservative treatments will include compression stockings, wet dressings, and elevation of the lower extremities in hopes of preventing infection (5). In patients with chronic venous insufficiency who are experiencing dermatologic abnormalities and have a history or suspicion of central venous obstruction, further investigation is warranted. This can include treatment at a specialized center with more in-depth imaging done (computed tomography venogram/MRV) and evaluation by a multidisciplinary team of clinical, diagnostic, and interventional specialists. Referral to interventional radiology in recurrent, severe cases of dermatologically presenting cases of chronic venous insufficiency can be an excellent adjunct to the current standards of care and could improve patient outcomes substantially (6). In summary, we present the clinical case, history, imaging studies, and postoperative photos of a 55-year-old male who presented with advanced chronic venous insufficiency. This case emphasizes the importance of collaborating with interventional radiologists to utilize an interdisciplinary approach that can improve the outcomes of patients who may present to an outpatient dermatology clinic with signs and symptoms of acute or chronic venous insufficiency and suspicion or history of central venous obstruction for more definitive treatment. This case describes the longitudinal treatment of one patient who found improvement with this treatment and more patients which is a limitation of this case report.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-39/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-39/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-39/coif). I.A. reports that she is the daughter of A.K.M.A. of IYA Medical, however not employed by IYA Medical. S.A.A. reports that he is the son of A.K.M.A. of IYA Medical. He is not employed at IYA Medical and did not receive any financial or other interest from this case. A.K.M.A. reports that IYA Medical is a profitable medical clinic and this patient was treated through his insurance and a monetary interest cannot be overlooked in this case. The payment for this patient’s treatment was in accordance with his insurance company and has not significantly changed or altered any specific details presented in this case. I.A. and S.A.A. are his children and did not receive any financial interest or otherwise. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were performed in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Agnihothri R, Shinkai K. Stasis Dermatitis. JAMA Dermatol 2021;157:1524. [Crossref] [PubMed]
- American Academy of Dermatology. Eczema types: Stasis dermatitis overview. Available online: https://www.aad.org/public/diseases/eczema/types/stasis-dermatitis
- Flugman SL. Stasis Dermatitis. Medscape 2020. Available online: https://emedicine.medscape.com/article/1084813-overview#a6
- Beauregard S, Gilchrest BA. A survey of skin problems and skin care regimens in the elderly. Arch Dermatol 1987;123:1638-43. [Crossref] [PubMed]
- Nayak L, Hildebolt CF, Vedantham S. Postthrombotic syndrome: feasibility of a strategy of imaging-guided endovascular intervention. J Vasc Interv Radiol 2012;23:1165-73. [Crossref] [PubMed]
- Raju A, Mallick R, Campbell C, et al. Real-World Assessment of Interventional Treatment Timing and Outcomes for Varicose Veins: A Retrospective Claims Analysis. J Vasc Interv Radiol 2016;27:58-67. [Crossref] [PubMed]
Cite this article as: Agha I, Asif N, Ghotra J, Cornell R, Khodra E, Agha SA, Agha AKM. A case report of inadequately treated acute deep venous thrombus and venous stasis. AME Case Rep 2024;8:9.




