
Takotsubo cardiomyopathy following a virtual work meeting during COVID-19 pandemic: a case report
Highlight box
Key findings
• Psychosocial stress induces physical distress with clinical manifestation.
What is known and what is new?
• Coronavirus disease 2019 (COVID-19) pandemic promotes increasing digitalization of the work environment and social isolation.
• Psychosocial stress evoked by virtual work meetings can be a trigger of Takotsubo cardiomyopathy.
What is the implication, and what should change now?
• Increase doctors’ awareness of the increased load of psychosocial stress due to COVID-19 leading to more or aggravated physical problems.
• Decrease social isolation and re-establish social (work) environment hand in hand with the growing COVID-19 immunization rate.
Introduction
Takotsubo cardiomyopathy (TTC) is a cardiac disorder featuring acute myocardial infarction and transient left ventricular systolic dysfunction often triggered by recent emotional or physical stress. Both, the symptoms (chest pain and/or dyspnea) and the electrocardiogram (ECG) changes (ST elevation, T-wave inversion, ST depression, left bundle branch block) resemble those of acute coronary syndrome (ACS). Even more, since serum troponin levels are elevated in those patients (1,2).
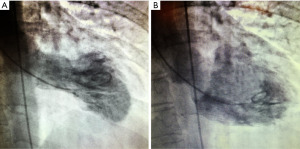
TTC is usually diagnosed by coronary angiography displaying a systolic apical ballooning appearance (3) despite coronary arteries not being obstructed.
Studies suggest catecholamine cardiotoxicity, coronary microvascular impairment, and coronary artery spasm as possible underlying causes (4,5). We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-18/rc).
Case presentation
A 56-year-old female without previous cardiac history presented to the emergency department at the Evangelisches Krankenhaus Düsseldorf (Germany) with a complaint of chest pain and dyspnea. Following an online work meeting in the morning she had developed left substernal chest pain without any radiation. The patient reported that already during the online session she felt very excited and mentally tense and did not improve even after calming down.
Prior to this, the patient was in good health, both physically and mentally, and denied any previous history of angina or similar symptoms in the past. She is of normal weight and performed well in a stress ECG which was performed during a checkup at the family doctor in 2020. Thus, she did not display an increased cardiovascular risk profile. She further reported no history of anxiety or other psychological disorders. Apart from cortisone cream to treat psoriasis on her hands and feet she took no further medication.
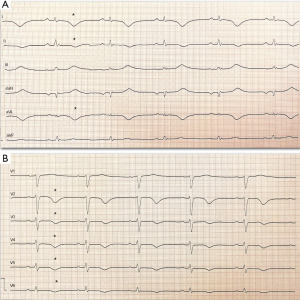
Upon arrival to the emergency department the initial vital signs were within normal limits and stable. Physical examination was essentially normal. ECG (Figure 1) showed a normal frequency sinus rhythm with T-wave inversions [leads I, II, augmented vector left (aVL) and anterolateral chest leads from V2 to V6]. Initial troponin-Ths levels were elevated at 352 ng/L (reference range <14 ng/L) and creatinine kinase levels at 119 U/L (reference range <170 U/L). After one hour the levels peaked at 359 ng/L and 121 U/L, respectively. A mildly reduced ejection fraction with hypokinesia of the anterior septum and apical segment was noted during transthoracic echocardiography.
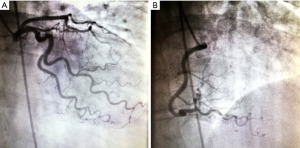
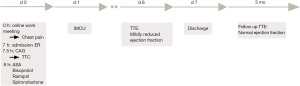
Since blood results and ECG findings were suggestive of ACS, coronary angiography was performed. This examination revealed no obstructive coronary artery disease (Figure 2) but demonstrated akinesia of the inferior, apical, and anterior wall with hyper-dynamic basal segments with apical ballooning indicating TTC (Figure 3). Guideline-directed medical therapy was initiated with bisoprolol [2.5 mg 1-0-1 per os (p.o.)], ramipril (2.5 mg 1-0-1 p.o.), spironolactone (25 mg 1-0-0 p.o.) and acetylsalicylic acid (100 mg 1-0-0 p.o.) (Figure 4). The next day, the patient reported no thoracic discomfort anymore. The medication was well-tolerated assessed by daily physical examination such as measurement of blood pressure and heart rate. Biochemistry analysis revealed decreasing troponin levels. The patient was discharged after seven days and instructed to follow up with ECG and transthoracic echocardiography in 4 weeks. The follow-up transthoracic echocardiography confirmed that the ejection fraction had normalized. The patient reported no discomfort anymore.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
To our knowledge we report the first case of TTC following a virtual work meeting (on a well-known online platform) during the coronavirus disease 2019 (COVID-19) pandemic. A previously healthy 56-year-old female acquired psychosocial stress-induced left ventricular dysfunction, diagnosed as TTC.
Proposed risk factors for TTC are stress-induced increase of catecholamines, microvascular dysfunction, inflammation, and estrogen deficiency (1,2,6). Often catecholamine levels are elevated in the plasma of these patients. Estrogen on the other hand executes protective effects on the vascular system promoting vasodilation and on the endothelium function (3). Therefore, postmenopausal women are more likely to miss out on these protective effects. Indeed, studies have illuminated that women older than 55 years have an almost five-fold risk of developing TTC compared to those younger than 55 years (7).
Recent studies unveiled an overall negative impact of COVID-19 on daily life, work and social activity associated with greater psychological difficulties (8,9).
In accordance with the COVID-19 restrictions at the work place many employees, and so our patient, are urged to work from home (WFH). WFH bears higher risks to suffer from social distancing and social isolation. Virtual meetings cannot replace face-to-face meetings in reality since they are often limited and regulated in terms of body language, interaction between colleagues and informal exchange of ideas. This promotes work conflicts more easily (10) associated with emotional distress.
Our patient matches this profile. She is post her menopause and older than 55 years. Furthermore, during the COVID-19 pandemic she worked from home for almost 12 months in a human resources department and had to face the psychosocial challenges evoked through the pandemic and the altered work situation. In this context, the emotional stress triggered at the work meeting may have been amplified out of scale.
Conclusions
This case undermines the impact of the COVID-19 pandemic on the psychosocial issues in this altered work environment.
In times of the ongoing pandemic, this topic is of current interest, since TTC has a comparable death rate to ACS (11). Thus, an early consultation and timely treatment at a hospital affiliated with a chest pain unit is mandatory; even more, since people avoid hospitals in fear of a COVID-19 infection and being out of capacity. During this challenging time, doctors should be aware of the increased load of psychosocial stress due to COVID-19 leading to more or aggravated physical problems such as demonstrated by our case of TTC.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-18/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-18/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-18/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 2004;141:858-65. [Crossref] [PubMed]
- Akashi YJ, Nef HM, Lyon AR. Epidemiology and pathophysiology of Takotsubo syndrome. Nat Rev Cardiol 2015;12:387-97. [Crossref] [PubMed]
- Ghadri JR, Wittstein IS, Prasad A, et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur Heart J 2018;39:2032-46. [Crossref] [PubMed]
- Ono R, Falcão LM. Takotsubo cardiomyopathy systematic review: Pathophysiologic process, clinical presentation and diagnostic approach to Takotsubo cardiomyopathy. Int J Cardiol 2016;209:196-205. [Crossref] [PubMed]
- Khalid N, Ahmad SA, Shlofmitz E, et al. Pathophysiology of Takotsubo Syndrome. 2023.
- Kurisu S, Kihara Y. Clinical management of takotsubo cardiomyopathy. Circ J 2014;78:1559-66. [Crossref] [PubMed]
- Deshmukh A, Kumar G, Pant S, et al. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J 2012;164:66-71.e1. [Crossref] [PubMed]
- Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. [Crossref] [PubMed]
- Zhang SX, Wang Y, Rauch A, et al. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res 2020;288:112958. [Crossref] [PubMed]
- Kniffin KM, Narayanan J, Anseel F, et al. COVID-19 and the workplace: Implications, issues, and insights for future research and action. Am Psychol 2021;76:63-77. [Crossref] [PubMed]
- Templin C, Ghadri JR, Diekmann J, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 2015;373:929-38. [Crossref] [PubMed]
Cite this article as: Zhu E, Scherschel K, Schedlowski M, Meyer C. Takotsubo cardiomyopathy following a virtual work meeting during COVID-19 pandemic: a case report. AME Case Rep 2023;7:40.


