
Surgical therapy for major lung parenchymal damage from late coronavirus disease complication: case report and literature review
Highlight box
Key findings
• Patients diagnosed with pulmonary caverns after coronavirus disease infection should be treated with broad-spectrum antibiotics. Those with signs of superinfection or lobar destruction should be reevaluated as soon as possible for surgical therapy.
What is known and what is new?
• Prolonged use of antibiotics or antivirals.
• Prolonged use of antibiotics would not have improved the general condition of the patients.
What is the implication, and what should change now?
• Patients with obvious symptoms of pulmonary damage or deterioration of the general condition should undergo radiological monitoring. Once another possible infectious focus has been ruled out, they should be re-evaluated for prompt surgical therapy.
Introduction
Coronavirus disease [severe acute respiratory syndrome coronavirus disease 19 (SARS COVID-19)] has emerged as one of the most challenging diseases of recent decades. Its sudden onset, accelerated spread, and impact on all economic, social, and health sectors has been devastating (1). Two years after the pandemic outbreak, our knowledge of the virus has expanded and developed, but we face a new wave of atypical complications that require special attention (1,2).
In addition to the acute complications of COVID-19 infection, late complications of the disease are taking an increasingly important part in the management of affected patients. Clinical symptoms that persist for longer than four weeks after infection, or that reappear after this period, are grouped under the collective term “Long COVID”. The symptomatology of Long COVID is broad and includes general symptoms such as fatigue, as well as organ-related complaints. Among the cardiac symptoms, the cardiac arrhythmias are frequently reported, and the pulmonary symptoms include prolonged cough, dyspnea. The neurological late effects may be pain or concentration, memory and mental disorders (2).
Pulmonary cavity formation is another serious long COVID complication that has been described in some cases in the literature (3-5). However, the exact pathophysiology, incidence, and an appropriate therapy of pulmonary cavities after COVID-19 are still unclear.
At this time, there are only limited published case reports regarding pulmonary cavity as long COVID. In this article, we present three cases of pulmonary cavity as a late complication after COVID-19, who were successfully treated by surgical treatment. Furthermore, to better understand this late complication, we performed a literature review of published articles. We present this case report in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-36/rc).
Case presentation
Case 1
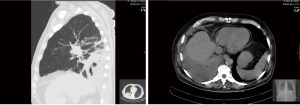
A 56-year-old female patient, multimorbid and unvaccinated, who was diagnosed with SARS COVID-19 pneumonia at the end of November 2021. She initially presented to our emergency department in early December because of progressive dyspnea and chest pain. Chest computed tomography (CT) revealed a left central and a right peripheral pulmonary embolism also typical CT findings of COVID-19 pneumonia with peripheral ground-glass opacities (GGOs) (Figure 1A). After hospital admission to the intensive care unit, therapeutic anticoagulation and ventilatory support using Optiflow (nasal high flow) were performed. After successful treatment with dexamethasone and tocilizumab [interleukin 6 (IL-6) receptor antagonist], her general condition improved and she was only supported with oxygen via nasal cannulas at 4 liters per minute. With a negative polymerase chain reaction test and stable condition, the patient was transferred to the normal ward after 14 days. Afterwards, with increasing infectious parameters another CT thorax examination was performed. CT morphology showed typical compact infiltration after COVID-19 pneumonia with beginning destruction of the left lower lobe and accompanying pleural effusion (Figure 1B,1C).

Neurologic deterioration accompanied by phase and opisthotonos developed in the following days. Meningitis was ruled out by lumbar puncture. Despite the administration of broad-spectrum antibiotics, the infection parameters increased dramatically [white blood cell (WBC) 19.7 mg/dL and C-reactive protein (CRP) level of 269 mg/L].
Therefore, a new CT examination (22 days later) was performed, which revealed a destroyed left lower lobe. As a result of the lobe destruction and an added bacterial superinfection the patient developed sepsis. Alveolar lavage and blood samples were positive for S. aureus. We performed a limited thoracotomy for lobectomy on an emergency status. Histopathological findings revealed infarct pneumonia with pulmonary artery embolism. Bacteriological result of the specimen revealed also S. aureus. There were no signs of a thoracic complication after surgery and the patient was discharged finally to a rehabilitation center.
Case 2
A 73-year-old male patient, multimorbid, with complete vaccination regimen (boosted), developed COVID-19 in early December 2021. Inpatient admission to the department of internal medicine was performed for further treatment and isolation. For further diagnosis, a CT thorax was performed, showing typical radiological COVID-19 infiltrations. Four weeks after the diagnosis of COVID-19, despite the antibiotic adjustment, infection parameters increased significantly (WBC 22 mg/dL and CRP level of 180 mg/L). Therefore, a new CT examination was performed (Figure 2). Here, a new spondylodiscitis and a right lower lobe consolidation with accompanying pleural empyema were revealed. The patient was referred to our thoracic center, and the indication for thoracoscopy was indicated. Intraoperatively, a stage III pleural empyema with a lung abscess of the right lower lobe was found. Due to advanced adhesions, thoracotomy followed by lobectomy and decortication of the empyema was performed. Histopathological findings revealed extensive pleuropneumonia in the setting of COVID-19 infection. The bacteriological result was positive for S. aureus. No complications occurred in the postoperative period, and the drain was removed on the sixth day due to prolonged air-leakage. The infection parameters were also regressive. The patient discharged nine days after the surgery.
Case 3
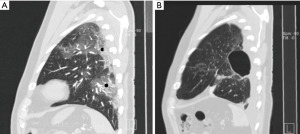
A 53-year-old male patient, who was non-vaccinated and diagnosed with COVID-19 pneumonia in early December 2021. The acute infection resolved after approximately 2 weeks. There was no requirement for ventilation during his hospitalization. The patient could be discharged on the fourth day. He was readmitted eight weeks later with progressive dyspnea and hemoptysis. Furthermore, he reported persistent left thoracic pain. On sonography of the pleura, a relevant pleural effusion was detected and punctured. Cytologically and microbiologically, the punctate showed no evidence of malignancy or inflammatory genesis. A chest CT scan showed extensive consolidation of the left apical lower lobe segment (Figure 3A) and a lunge cavity (Figure 3B). Due to the persistence of hemoptysis, we performed a video thoracoscopic resection of the left segment 6 using a uniportal technique. Already on the first postoperative day, after removal of the chest drain, thoracic pain was no longer present. We were able to discharge the patient on the second postoperative day without preexisting pain or hemoptysis. Histopathological findings revealed significant dystelectatic and hemoptysed lung tissue, as well as focal intraalveolar fibrosis. One week later, in the postoperative consultation, there were no postoperative complications with completed wound healing.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
To identify relevant articles published until March 2022, we carried out a literature search of the PubMed and Web of Science databases. The reference lists of relevant articles were screened for additional eligible studies.
A total of 12 publications with only 50 patients were found, of which nine were case reports and three were case series. Most of articles were published in a period before the development of the COVID vaccines. Except two articles without detailed information, all patients received no vaccination. Therefore, there are still no specific data correlating the benefits of vaccination with the prevention of these complications. As shown in Table 1, an interval time between acute infection and the appearance of pulmonary cavities was about 4 weeks (2–9 weeks). The results showed that most patients (n=25) were treated with conservative therapies (e.g., antibiotics, antivirals, bronchoscopy with bronchoalveolar lavage, etc.).
Table 1
| Reference | Study type | Sample size | Vaccination | Interval* | Therapy | Mortality |
|---|---|---|---|---|---|---|
| Bakhle et al., 2022 (6) | Case report | 1 | No | 2 weeks | Conservative | 0% |
| Amalnath et al., 2022 (7) | Case series | 22 | Unknown | 2–4 weeks | Unclear | 82% |
| Zamani et al., 2021 (8) | Case report | 1 | No | 3 weeks | Conservative | 0% |
| Zoumot et al., 2021 (5) | Case series | 12 | No | 3–7 weeks | Conservative and bronchoalveolar lavage | 50% |
| Kurys-Denis et al., 2021 (3) | Case series | 6 | Unknown | 2–6 weeks | Conservative | 0% |
| Egoryan et al., 2021 (9) | Case report | 1 | No | 2 weeks | VATS decortication | 0% |
| Afrazi et al., 2021 (10) | Case report | 1 | No | 2 weeks | Conservative | 0% |
| Abdelhadi et al., 2021 (11) | Case report | 1 | No | 2 weeks | Conservative | 0% |
| Renaud-Picard et al., 2020 (12) | Case report | 1 | No | 3 weeks | Conservative | 0% |
| Selvaraj et al. 2020 (4) | Case report | 1 | No | 3 weeks | Conservative and bronchoalveolar lavage | 0% |
| Muheim et al., 2020 (13) | Case report | 2 | No | 5 and 9 weeks | Conservative/bronchoalveolar lavage and CT-guided drainage | – |
| Chen et al., 2020 (14) | Case report | 1 | No | 2 weeks | Conservative | 0% |
*, interval from first symptoms of COVID-19 infection to pulmonary cavities. COVID-19, coronavirus disease 19; VATS, video-assisted thoracic surgery; CT, computed tomography.
Only two patients were treated using invasive therapies. One patient underwent CT-guided drainage (13), and another underwent video-assisted thoracic surgery for decortication (9). Both patients were successfully treated and recovered from the procedures.
The long-term consequences of COVID-19 infection are currently unknown, but recent data suggest that some patients continue to develop symptoms and complications associated with COVID-19 after acute infection, termed long COVID (2-15). Cavitation of the lungs is a rare complication that has been reported mostly in the acute and subacute phases of infection (15,16). These do not seem to occur necessarily in the preexisting pulmonary lesions 9). Our cases were also lung healthy and never smokers until the time of infection. Therefore, it lets not to think primarily about the pulmonary susceptibility, since it is also reported in the pediatric literature about the pulmonary cavity in the newborn as a presumptive COVID manifestation (6).
The patients who undergo the elective surgical procedures within eight weeks after COVID-19 infection are exposed to higher perioperative risks, especially postoperative pneumonia (17). The fact remains that survived COVID-19 infection can cause structural parenchymal destruction of the lung. In our report we mention three cases in which the indication for surgery was due to sepsis in two of them and in one hemoptysis. The prolonged use of antibiotics would not have improved the general condition of the patients.
In this regard, this alteration can occur at any age and can also involve the pulmonary healthy patients. The clinical course of affected individuals can range from complete asymptomatic to severe symptoms such as hemoptysis or abscess formation (12).
This group of patients with late COVID complications requires individualized treatment strategy, despite the increased perioperative risks.
Conclusions
According to the literature review and our experiences, in patients with a diagnosis of pulmonary cavity after COVID infection (without any sign of sepsis), a board-spectrum antibiotical therapy with penicillins and beta-lactamase inhibitors like piperacilin/tazobactam should be administrated as a first-line therapy. In patients without sign of destroyed lung and well-limited cavities, a CT-guided drainage could be also performed as a co-therapy. A routine bronchoscopy is very useful to rule out any defect with the intrabronchial tract.
The patients with persistent symptoms (fever, hemoptysis, etc.), impaired general condition, or any sign of sepsis should undergo a CT control to rule out other infection focuses/impaired lung. These patients should be thereafter discussed in an interdisciplinary team and evaluated for a possible surgical therapy.
Acknowledgments
The abstract was successfully submitted and presented at the 31st Annual Meeting of the German Society for Thoracic Surgery in September 2022.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-36/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-36/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-36/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Coronavirus disease (COVID-19): situation report, 156. Geneva: World Health Organization; 2020.
- Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond) 2021;53:737-54. [Crossref] [PubMed]
- Kurys-Denis E, Grzywa-Celińska A, Celiński R. Lung cavitation as a consequence of coronavirus-19 pneumonia. Eur Rev Med Pharmacol Sci 2021;25:5936-41. [PubMed]
- Selvaraj V, Dapaah-Afriyie K. Lung cavitation due to COVID-19 pneumonia. BMJ Case Rep 2020;13:e237245. [Crossref] [PubMed]
- Zoumot Z, Bonilla MF, Wahla AS, et al. Pulmonary cavitation: an under-recognized late complication of severe COVID-19 lung disease. BMC Pulm Med 2021;21:24. [Crossref] [PubMed]
- Bakhle A, Sreekumar K, Baracho B, et al. Cavitary lung lesions in a neonate: Potential manifestation of COVID-19 related multisystem inflammatory syndrome. Pediatr Pulmonol 2022;57:311-4. [Crossref] [PubMed]
- Amalnath D, Barathi D, Pari H. Uncommon Manifestation of COVID -19 - Delayed Onset Cavitating Lung Lesions, a Retrospective Study of 22 Patients from a Tertiary Care Centre in Southern India. J Assoc Physicians India 2022;70:11-2. [PubMed]
- Zamani N, Aloosh O, Ahsant S, et al. Lung abscess as a complication of COVID-19 infection, a case report. Clin Case Rep 2021;9:1130-4. [Crossref] [PubMed]
- Egoryan G, Hyser E, Mushtaq AH, et al. Development of cavitary lung disease as a long-term complication of coronavirus disease 2019 in a young previously healthy patient: a case report. J Med Case Rep 2021;15:377. [Crossref] [PubMed]
- Afrazi A, Garcia-Rodriguez S, Maloney JD, et al. Cavitary lung lesions and pneumothorax in a healthy patient with active coronavirus-19 (COVID-19) viral pneumonia. Interact Cardiovasc Thorac Surg 2021;32:150-2. [Crossref] [PubMed]
- Abdelhadi A, Kassem A. Candida Pneumonia with Lung Abscess as a Complication of Severe COVID-19 Pneumonia. Int Med Case Rep J 2021;14:853-61. [Crossref] [PubMed]
- Renaud-Picard B, Gallais F, Riou M, et al. Delayed pulmonary abscess following COVID-19 pneumonia: A case report. Respir Med Res 2020;78:100776. [Crossref] [PubMed]
- Muheim M, Weber FJ, Muggensturm P, et al. An unusual course of disease in two patients with COVID-19: pulmonary cavitation. BMJ Case Rep 2020;13:e237967. [Crossref] [PubMed]
- Chen J, Peng S, Zhang B, et al. An uncommon manifestation of COVID-19 pneumonia on CT scan with small cavities in the lungs: A case report. Medicine (Baltimore) 2020;99:e21240. [Crossref] [PubMed]
- Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020;324:782-93. [Crossref] [PubMed]
- Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med 2021;27:601-15. [Crossref] [PubMed]
- Deng JZ, Chan JS, Potter AL, et al. The Risk of Postoperative Complications After Major Elective Surgery in Active or Resolved COVID-19 in the United States. Ann Surg 2022;275:242-6. [Crossref] [PubMed]
Cite this article as: Gamrekeli A, Ramirez-Fragoso F, Ghamarnejad O, Kardassis D, Stöckle F, Custodis F, Stavrou GA. Surgical therapy for major lung parenchymal damage from late coronavirus disease complication: case report and literature review. AME Case Rep 2023;7:33.


