
Non-operative treatment of atlanto-occipital incongruity following high energy trauma: a case report
Highlight box
Key findings
• O-C1 incongruity discovered following C1-C2 fusion.
• Diagnosis, management and outcome of a case of O-C1 incongruity treated non-operatively in a C-collar with success.
What is known and what is new?
• Occipitocervical dislocation can be a devastating injury leading to significant neurologic deficit, morbidity and mortality, and has historically been treated with operative fusion.
• Here we present a case of O-C1 incongruity that was treated non-operatively with success.
What is the implication, and what should change now?
• Not all cases of O-C1 incongruity equate to instability requiring surgery.
• Surgeons should avoid unnecessary high-cervical fusions which can decrease flexion and extension by 50%.
Introduction
Traumatic occipitocervical dislocations (OCDs) are rare and potentially devastating injuries (1). Their prevalence is roughly 6–8%, and can represent up to 15-20% of fatal cervical spine injuries (2). They often result from sudden deceleration in high-energy trauma. The craniocervical articulation is restrained primarily by the tectorial membrane, the alar ligaments and the atlanto-occipital (O-C1) joint capsules. The apical ligament is often considered a rudimentary structure, and is absent in 20% of cases. The Barkow ligament connects the tip of the odontoid to the occipital condyle, acting to prevent neck hyperextension. The cruciform ligament is made up of longitudinal and transverse bands that center posterior to the odontoid. The transverse bands limit lateral motion of C1 relative to the dens and prevent posterior displacement, while the longitudinal band connects the body of C2 to the basion. OCD results from disruption of some or all of these structures (3).
In most trauma centers, the diagnosis is typically made by computer tomography (CT), as well as magnetic resonance imaging (MRI) if ligamentous disruption is suspected and/or neurological deficits are present. The condyle to C1 interval (CCI) is considered a highly sensitive parameter for diagnosing OCD and is abnormal when >1.5 mm with a condylar sum of >3.0 mm (4). Traction testing is useful in determining stability of the soft tissues supporting this complex joint, with >2 mm distraction considered abnormal or unstable (5,6). During this test, a Mayfield skull clamp is applied to the patient’s skull, and manual traction is applied. Lateral X-ray (XR) of the cervical spine is taken prior to traction, and during traction to assess for any cranial displacement of the occipital condyles relative to the atlas.
Delayed diagnosis and management of this condition is a well-known risk factor for poor outcomes in the high-energy polytraumatized patient. Higher Injury Severity Score (ISS) and better neurologic presentation have been associated with missed diagnosis, and delay in treatment has been associated with increased likelihood of neurological deterioration (5,7). This is largely due to the fact that patients with higher ISS scores are more likely to present to trauma bays with more life-threatening injuries requiring urgent or emergent intervention, which may draw attention away from an OCD. Numerous case reports and larger case series have demonstrated that early surgical stabilization can predictably improve outcomes and neurological recovery in patients who sustain these injuries (5,8,9). Cranio-cervical fixation is still largely considered the treatment of choice for the majority of cases of traumatic OCD, and was recommended in the 2013 guidelines from the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee (10).
Distraction at the O-C1 joints or incongruent O-C1 joints are considered an indication for OCD fusion. Most patients with distraction at O-C1 joints or incongruent O-C1 joints are diagnosed with OCD and are taken to surgery for occipitocervical fusion.
We present a case of distraction injury at the C1-C2 joints with incongruent O-C1 joints found on post-operative CT imaging following C1-C2 posterior fusion. This patient underwent traction testing and there was no obvious instability detected. Thus, this patient was treated conservatively for his O-C1 injury without surgical fusion. Normally, occipitocervical fusion will fuse two joints, O-C1 and C1-C2. Fusing O-C1 will eliminate 50% of flexion/extension, while fusing C1-C2 will eliminate 50% of rotation. We truly believe surgical fusion is only indicated for unstable OCD patients. This patient showed that an incongruent O-C1 joint may not always equate to an unstable injury pattern and may not always require occipitocervical fusion. This manuscript is written following CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-23/rc).
Case presentation
A 19-year-old man with a history of obesity [body mass index (BMI): 38.74 kg/m2] was involved in a high-speed head-on motor vehicle collision. He had a prolonged extrication, and on arrival paramedics were concerned with his ability to maintain his airway due to multiple mandibular and facial fractures. He was therefore intubated in the field, and transferred to a level 1 trauma center for further management.
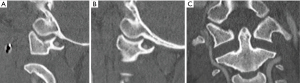
On arrival, he had elevated troponins but otherwise normal laboratory workup and electrocardiogram (EKG). He remained hypotensive throughout his initial presentation. He had multiple facial lacerations. A reliable neurologic exam could not be obtained due to the patient’s intubated and sedated status, however bulbocavernosus reflex was intact, reflexes were normal and the patient did not demonstrate evidence of spinal or neurogenic shock. Radiographs revealed a right Arbeitsgemeinschaft für Osteosynthesefragen (AO) Type C Pilon fracture, a right cuboid fracture, and a left anterior hip dislocation. CT of the head revealed bilateral mandibular fractures, and a right lateral pterygoid fracture, without evidence of intracranial hemorrhage or embolus. CT of the full spine revealed distraction of the C1-C2 articulation without associated fracture, and without clear disruption or distraction of the O-C1 joint (Figure 1A-1C). The patient was placed in a Miami J cervical collar (C-collar). Due to persistent hemodynamic instability with no obvious source, he was taken to the operating room (OR) for emergent exploratory laparotomy with general surgery, which ultimately did not reveal any intraabdominal hemorrhage or injury. His left hip was closed reduced while on the operating table after the abdomen was closed.
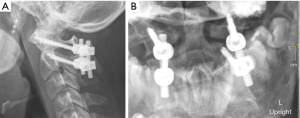
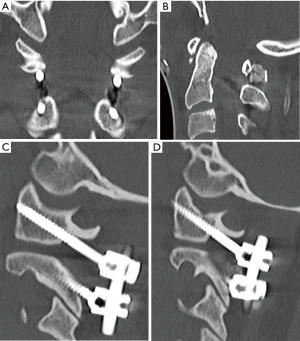
Less than 24 hours after presentation, the patient was taken to the OR for urgent management of his multiple injuries. He first underwent external fixation of his right pilon fracture, followed by C1-C2 posterior instrumentation and fusion (Figure 2). He was placed in a C-collar and transferred to the intensive care unit (ICU) post-operatively. Per our institution protocol, post-operative cervical spine CT was obtained which revealed further distraction and subluxation of the occipitocervical junction bilaterally, with a CCI of 4 mm bilaterally, a basion-dens interval (BDI) of 10 mm, and a Power’s Ratio of 1.1 (Figure 3). Due to concern for significant injury, the patient was brought back urgently to the OR for traction testing to rule out OCD.
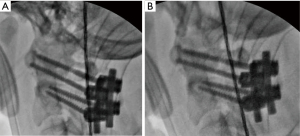
The patient was positioned supine on the operating table. Mayfield pins were applied to the patient’s head, and C-arm was positioned for lateral imaging. Manual traction was applied, without evidence of widening of the O-C1 joint (Figure 4), and therefore the traction test was confirmed to be negative. The patient was externally stabilized in a Miami-J C-collar for 12 weeks post-operatively. Once awakened from sedation, the patient was found to have no neurologic deficits. At 4 weeks post-operatively, he was found to have drainage and a small dehiscence from the middle portion of his posterior cervical wound, requiring operative irrigation and debridement for presumed surgical site infection (SSI). At 12 weeks post-operatively from C1-C2 posterior instrumentation and fusion, he was evaluated in clinic and found to have no motor or sensory deficits, no neck pain and maintained C1-C2 and O-C1 articulations, without subluxation on flexion and extension views (Figure 5).

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Traumatic OCDs are typically the result of high energy mechanisms and present with quite variable neurologic symptoms. They may be associated with polytraumatic injuries, as well as variable stability patterns (1). These injuries can result from low energy mechanisms as well, particularly in older patients or patients with previous cervical fusions, as Tavolaro et al. showed (11). Reis et al. showed that missed diagnosis and delayed treatment of OCD is associated with poorer neurological outcome (8). Reasons for delayed diagnosis are multifactorial. They are often missed or overlooked particularly in patients with multiple other injuries which contributes to their high rates of morbidity. Other reasons include low clinical suspicion, and inexperience with evaluating the craniocervical junction (CCJ) (7).
In the initial evaluation of traumatized patients, traditional cervical radiographs should be evaluated scrupulously, but are oftentimes insufficient as they can have variable results based on patient body habitus, positioning and external immobilization devices, and also do not adequately capture the complex osseoligamentous structures that support the CCJ and atlantoaxial spine (12,13). Spine CT is a more reliable imaging modality in evaluating acute fractures, dislocations and disruptions of the CCJ complex (4,14). MRI is also particularly helpful in evaluating the integrity of the soft tissues, spinal cord, and brainstem (6,15). This is the ideal modality for assessing the tectorial membrane, transverse ligament, alar ligaments and occipitocervical joint capsules when there is suspicion for traumatic disruption of these supportive soft tissue structures (16,17). In the diagnosis of OCD, dynamic traction fluoroscopy has been shown to be a reliable and accurate diagnostic modality to determine the stability of the CCJ (3,5). It can be utilized in conjunction with or in place of MRI.
Our patient presented directly to a level 1 trauma center with multiple injuries, and with no neurological deficits based on initial examination. Cervical radiographs and CT full spine demonstrated distraction at the atlantoaxial articulation, which was emergently stabilized with C1-C2 posterior instrumentation and fusion. CT of the cervical spine following instrumentation showed both longitudinal distraction of the O-C1 joints with anterior subluxation of the occiput, which had increased compared to pre-operative CT of the cervical spine. This amounted to an increased Power’s Ratio, a high-normal BDI, and an elevated CCI. This prompted an emergent return to the operating OR for traction testing to evaluate the stability of the occipitocervical junction, which did not displace. MRI was not obtained given the recently placed posterior cervical hardware, and concern for increased signal and potentially limited diagnostic power compared to intraoperative traction testing. Once the injury had been assessed and found to be overall stable on dynamic testing, the patient was treated conservatively with external immobilization in a C-collar for 12 weeks.
The patient showed good adherence to post-operative protocols and had adequate follow-up through 3 months post-operatively. That said, one limitation is that he did not return to clinic after removal of his C-collar and return to activity, which limits our longer-term follow-up data. Another limitation is our lack of a clear neurological examination on initial presentation, which unfortunately did not allow us to establish a baseline from which to compare his post-operative outcome.
Our non-operative treatment strategy was selected based on the incongruity of the O-C1 with no evidence of instability and a normal neurologic exam. This breaks from the traditional dogma of early surgical stabilization for patients with an incongruent O-C1 joint (10,18,19). Surgical stabilization is considered the treatment of choice to prevent further neurologic injury in the setting of an incongruent O-C1 joint. In our case, the initial displacement and likely energy transfer was directed through the C1-C2 articulation, with presumed disruption of the C1-C2 joint complex based on distraction of the posterior column at those levels. As this patient was already fused from C1-C2 (leading to 50% decrease in rotational motion), we felt that further fusion leading to decreased flexion-extension would provide little additional stability and cause significantly increased stiffness of the cervical spine for this young patient. At 12 weeks post-operatively, the patient experienced no neck pain, good adherence to wearing C-collar at all times with limited range of motion (ROM), and flexion/extension radiographs showed no evidence of subluxation or distraction at the O-C1 joints indicating a good clinical outcome. We therefore feel that even if the O-C1 joint is incongruent on radiographs and CT scans, this may not always equate to an unstable OCD and therefore may not require posterior fusion.
Conclusions
Traumatic OCD is a potentially devastating injury pattern that should be thoroughly evaluated, and treatment should be tailored to each specific and unique patient presentation. These injuries can be the result of both high and low energy mechanisms, and can present in a variety of ways. In patients with a stable neurological exam, CT of the cervical spine should be used primarily in the diagnostic compendium of OCDs to evaluate important anatomic relationships that may be disrupted in the traumatic setting. In addition, dynamic traction testing should be utilized to give a more comprehensive assessment of the ligamentous stability of these injuries. Incongruity of the O-C1 joint may not be synonymous with instability as previously thought, and in cases of O-C1 incongruity with stable traction testing, non-operative treatment with external immobilization can be considered as a viable treatment option even in the polytraumatized patient.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-23/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-23/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-23/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mueller FJ, Kinner B, Rosskopf M, et al. Incidence and outcome of atlanto-occipital dissociation at a level 1 trauma centre: a prospective study of five cases within 5 years. Eur Spine J 2013;22:65-71. [Crossref] [PubMed]
- Anania P, Fiaschi P, Sbaffi PF, et al. A Case of Asymptomatic Occipital Condyle Fracture with Incomplete Occipitocervical Dislocation: How Did It Happen? World Neurosurg 2018;109:403-8. [Crossref] [PubMed]
- Child Z, Rau D, Lee MJ, et al. The provocative radiographic traction test for diagnosing craniocervical dissociation: a cadaveric biomechanical study and reappraisal of the pathogenesis of instability. Spine J 2016;16:1116-23. [Crossref] [PubMed]
- Martinez-Del-Campo E, Kalb S, Soriano-Baron H, et al. Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine 2016;24:535-45. [Crossref] [PubMed]
- Bellabarba C, Mirza SK, West GA, et al. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine 2006;4:429-40. [Crossref] [PubMed]
- Kasliwal MK, Fontes RB, Traynelis VC. Occipitocervical dissociation-incidence, evaluation, and treatment. Curr Rev Musculoskelet Med 2016;9:247-54. [Crossref] [PubMed]
- Mendenhall SK, Sivaganesan A, Mistry A, et al. Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J 2015;15:2385-95. [Crossref] [PubMed]
- Reis A, Bransford R, Penoyar T, et al. Diagnosis and treatment of craniocervical dissociation in 48 consecutive survivors. Evid Based Spine Care J 2010;1:69-70. [Crossref] [PubMed]
- Labler L, Eid K, Platz A, et al. Atlanto-occipital dislocation: four case reports of survival in adults and review of the literature. Eur Spine J 2004;13:172-80. [Crossref] [PubMed]
- Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 2013;72:114-26. [Crossref] [PubMed]
- Tavolaro C, Bransford R, Yerrapragada A, et al. Occipitocervical Dislocation in Low-Energy Trauma. Case Rep Orthop 2018;2018:3931525. [Crossref] [PubMed]
- Dziurzynski K, Anderson PA, Bean DB, et al. A blinded assessment of radiographic criteria for atlanto-occipital dislocation. Spine (Phila Pa 1976) 2005;30:1427-32. [Crossref] [PubMed]
- Harris JH Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol 1994;162:881-6. [Crossref] [PubMed]
- Gire JD, Roberto RF, Bobinski M, et al. The utility and accuracy of computed tomography in the diagnosis of occipitocervical dissociation. Spine J 2013;13:510-9. [Crossref] [PubMed]
- Roy AK, Miller BA, Holland CM, et al. Magnetic resonance imaging of traumatic injury to the craniovertebral junction: a case-based review. Neurosurg Focus 2015;38:E3. [Crossref] [PubMed]
- Radcliff KE, Hussain MM, Moldavsky M, et al. In vitro biomechanics of the craniocervical junction-a sequential sectioning of its stabilizing structures. Spine J 2015;15:1618-28. [Crossref] [PubMed]
- Kim YJ, Yoo CJ, Park CW, et al. Traumatic Atlanto-occipital Dislocation (AOD). Korean J Spine 2012;9:85-91. [Crossref] [PubMed]
- Joaquim AF, Ghizoni E, Tedeschi H, et al. Upper cervical injuries - a rational approach to guide surgical management. J Spinal Cord Med 2014;37:139-51. [Crossref] [PubMed]
- Ji XT, Li A, Wang Q, et al. Posterior reduction and instrumentation with rod-screw construct for atlanto-axial dislocation: a single institutional study with 21 consecutive cases. Clin Neurol Neurosurg 2013;115:1433-9. [Crossref] [PubMed]
Cite this article as: Bunzel EW, Khoo K, Zhou H. Non-operative treatment of atlanto-occipital incongruity following high energy trauma: a case report. AME Case Rep 2023;7:24.


