
Improvement in peripheral bronchoscopy requires the use of advanced imaging
We have read the recently published article “Combined Portable Cone Beam Computed Tomography and Robotic-assisted Bronchoscopy Impacting Diagnosis of a Solitary Pulmonary Nodule: a Case Report” by Duke and colleagues with great interest (1). We congratulate the authors on this successful submission and would like to offer a few comments regarding the use of advanced imaging for peripheral pulmonary lesion (PPL) evaluation.
The arena of PPL evaluation has exploded over the last two decades with the implementation of lung cancer screening and an aging population combined with improved diagnostic and therapeutic techniques (2). The importance of this cannot be understated, as early detection and prompt treatment for lung cancer significantly improves outcomes (3). Historically, there was minimal need for bronchoscopy in the evaluation of PPLs due to an unacceptably low yield of approximately 37%, compared to a 92% yield of computed tomography (CT)-guided transthoracic needle biopsy (4,5). However, several technological advancements including electromagnetic navigation bronchoscopy (ENB), radial endobronchial ultrasound (r-EBUS), robotic-assisted bronchoscopy (RAB), augmented fluoroscopy (AF), and cone-beam CT (CBCT) have catapulted navigational bronchoscopy to the forefront of PPL evaluation. The early studies on ENB with r-EBUS demonstrated sensitivities from 67% to 84% with a systematic review and meta-analysis demonstrating an approximately 77% yield (using the superDimension® system) (6). A more recently published multicenter pilot and feasibility study by Chen and colleagues using robotic-assisted bronchoscopy (Monarch® robotic platform) combined with r-EBUS and fluoroscopy demonstrated a 96% lesion localization (7).
Although electromagnetic navigational bronchoscopy continues to progress and multiple studies have demonstrated the ability to navigate safely into the periphery, the intra-procedural nodule location compared to pre-operative CT chest, the so called “CT-to-body divergence”, remains a crucial bottleneck. In the simplest of forms, a routine CT chest is ideally performed at total lung capacity (TLC), which cannot be consistently reproduced intraoperatively. Diaphragmatic movement, airway distortion, segmental occlusion with the bronchoscope, airway bleeding, and most importantly, atelectasis result in a highly variable nodule location. A study by Pritchett and colleagues found that nodule divergence distance during bronchoscopy could vary quite significantly, with an average of 13mm in the upper lobes and 22mm in non-upper lobes (8). Certain maneuvers such as high positive end-expiratory pressures (PEEP), lower fraction of inspired oxygen, and air insufflation help minimize atelectasis, but these interventions fall short of routine CT chest physiologic parameters and may also contribute to hemodynamic complications. One way to overcome this hurdle is by utilizing intra-procedural advanced imaging modalities that seamlessly integrate into the navigation system to provide guidance to the bronchoscopist. There are currently no widely available RAB platforms that integrate the advanced imaging modality into the RAB system. Illumisite® by Medtronic does offer an integrated fluoroscopic navigation with electromagnetic navigation, albeit without a robotic arm. The majority of platforms currently rely on multiple different, non-communicating platforms during the procedure. Although these technologies clearly improve lesion localization, an integrated platform, which provides direction to the bronchoscopist would likely allow these technologies to be more widely accepted and utilized.
Although there remains a need for an integrated imaging systems to improve lesion localization, a single-procedure, bronchoscopic approach maintains several advantages over CT-guided biopsies. In addition to a reduced risk of pneumothorax, another critical advantage is the ability to perform EBUS with transbronchial needle aspiration to sample hilar and mediastinal lymph nodes for tumor staging (9). Confirmation of tool-in-lesion using advanced imaging along with immediate nodal staging could combine the sensitivity of CT-guided biopsies and the standard of care lymph node staging into a single procedure. The role of bronchoscopy and EBUS staging remains vital in the multidisciplinary approach to lung cancer diagnosis and treatment. Additional case reports, rigorous studies, and technological advancements are required to advance the field.
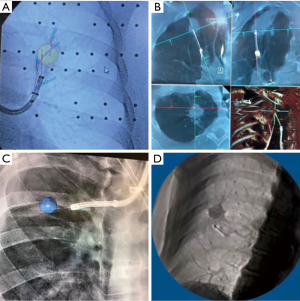
The authors’ successful use of mobile 3D imaging to assist robotic bronchoscopy is yet another example where adding advanced imaging to peripheral bronchoscopy improves diagnostic sensitivity and more importantly, reduces delays in care and additional procedures. In this case, the catheter was initially 1.8 cm inferior to the target lesion; however, after implementation of mobile three-dimensional (3D) imaging, the catheter was renavigated and the team was able to confirm tool-in-lesion which led to a diagnosis of adenocarcinoma. Our own experience during peripheral bronchoscopy is similar, where using advanced imaging technology helps with making fine adjustments to the bronchoscope to reach the target PPL, as demonstrated in Figure 1A-1D. While robotic bronchoscopy clearly offers improved reach, vision, stability, and control, it still needs integrated advanced imaging into the platform to truly improve accuracy. It is imperative that the future direction of peripheral bronchoscopy includes advanced imaging, which will lead to improved lesion localization, diagnostic yield, and hopefully, additional therapeutic options in the future.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Case Reports. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-27/coif). AW reports that he has worked as a consultant for Noah Medical and is also a speaker for Biodesix. KP has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Duke JD, Fernandez-Bussy S, Reisenauer J. Combined portable cone beam computed tomography and robotic-assisted bronchoscopy impacting diagnosis of a solitary pulmonary nodule: a case report. AME Case Rep 2022;6:23. [Crossref] [PubMed]
- Meza R, Jeon J, Toumazis I, et al. Evaluation of the Benefits and Harms of Lung Cancer Screening With Low-Dose Computed Tomography: Modeling Study for the US Preventive Services Task Force. JAMA 2021;325:988-97. [Crossref] [PubMed]
- Blandin Knight S, Crosbie PA, Balata H, et al. Progress and prospects of early detection in lung cancer. Open Biol 2017;7:170070. [Crossref] [PubMed]
- DiBardino DM, Yarmus LB, Semaan RW. Transthoracic needle biopsy of the lung. J Thorac Dis 2015;7:S304-16. [PubMed]
- Tanner NT, Yarmus L, Chen A, et al. Standard Bronchoscopy With Fluoroscopy vs Thin Bronchoscopy and Radial Endobronchial Ultrasound for Biopsy of Pulmonary Lesions: A Multicenter, Prospective, Randomized Trial. Chest 2018;154:1035-43. [Crossref] [PubMed]
- Folch EE, Pritchett MA, Nead MA, et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J Thorac Oncol 2019;14:445-58. [Crossref] [PubMed]
- Chen AC, Pastis NJ Jr, Mahajan AK, et al. Robotic Bronchoscopy for Peripheral Pulmonary Lesions: A Multicenter Pilot and Feasibility Study (BENEFIT). Chest 2021;159:845-852. [Crossref] [PubMed]
- Pritchett MA, Schampaert S, de Groot JAH, et al. Cone-Beam CT With Augmented Fluoroscopy Combined With Electromagnetic Navigation Bronchoscopy for Biopsy of Pulmonary Nodules. J Bronchology Interv Pulmonol 2018;25:274-82. [Crossref] [PubMed]
- Dale CR, Madtes DK, Fan VS, et al. Navigational bronchoscopy with biopsy versus computed tomography-guided biopsy for the diagnosis of a solitary pulmonary nodule: a cost-consequences analysis. J Bronchology Interv Pulmonol 2012;19:294-303. [Crossref] [PubMed]
Cite this article as: Potts K, Wagh A. Improvement in peripheral bronchoscopy requires the use of advanced imaging. AME Case Rep 2022;6:30.


