Surgical excision of a tufted angioma of the hand in an adult—a rare case report with a review of literature
Introduction
Tufted angioma is also known as Angioblastoma of Nakagawa (1) first described it in Japanese literature with the name “angioblastoma” in 1949 (2). The author suggested that this lesion is composed of undifferentiated atypical mesenchymal cells (3).
In 1971 Macmillan and Champion first described Tufted Angioma with the term “progressive capillary haemangioma” in English literature (2). To avoid misunderstanding with cerebellar haemangioblastoma (3), in 1976, Wilson Jones coined the term of Tufted Angioma, referring to dermis small delimited dusky red plaques with progressive enlargement (4) that are similar to strawberry nevi (5). Jones and Orkin separated it from Kaposi’s sarcoma or low-grade angiosarcoma in 1989 (4).
However, diagnosis of tufted angioma is infrequent and true incidence remains unknown.
As of 2015, only 158 cases are described in the English-language literature. No racial or gender predilection is recognized for tufted angioma. Patient with tufted angioma with a strong family history of similar lesions transmitted in an autosomal-dominant mode of inheritance have been reported (6). In those patients, lesion spontaneously regressed.
Most of these benign vascular tumors develop in childhood (2) with approximately 25% with congenital presentation and 50% of them that appear in the first year of life. Acquired TA has been reported in immuno-compromised adults (7), older individuals are occasionally affected (2).
Tufted angioma must be distinguished from other vascular tumors including infantile hemangiomas, congenital hemangiomas, vascular malformations and, especially in adult-onset cases, Kaposi form hemangio-endothelioma or Kaposi’s sarcoma (1). When present in old patient, this lesion should be distinguished from angiosarcoma (8).
No causes of TA have yet been established. Trauma does not appear to be a predisposing factor, although a report describes the development of a lesion of tufted angioma at the site of a previous arthropod bite (1).
Solitary cutaneous TA is an asymptomatic lesion with excellent prognosis as reported in our report.
Case presentation
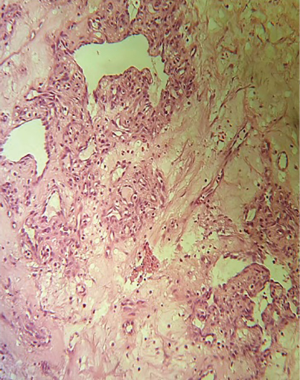
We present the case of a 29-year-old Chinese woman who was admitted to hospital for a bloody neoplasm of the second finger of the left hand. The patient reports the appearance of paint at the level of neoformation without loss of finger function. The case history was partially unclear. Patient reported having this neoformation with a slow growth over the years, but did not remember a specific trigger. The neoplasia sometimes caused intense pain and this was also due to the position it occupied in the hand. The first diagnostic hypotheses could be: foreign body granuloma, wart of the hand, tumor (e.g., ulcerated spinocellular carcinoma, basal cell tumor), hemangiopericytoma, angioma. The patient was not sure if she had received an unspecified insect bite some time ago and at a first observation of the lesion we thought of a granuloma. However, the patient reported having always had a reddish appearance on her finger and a long history could not be justified by a recent traumatic event. There was no history of other types of cutaneous lesion, infection or any drug intake. No physical or systemic abnormality was noted. Patient had normal haemogram, coagulation profile and immune status. This neoplasm was a greyish nodular neoformation of 3.1 cm of maximum diameter with focal brunest areas and tensile-elastic texture superficially ulcerated. Lesion was completely excised and submitted for histopathological examination. The final diagnosis was “Tufted angioma” (Figures 1 and 2) because of the histologic finding of small circumscribed angiomatous tufts and lobules scattered in the dermis. Cell marker studies suggest that the cell lobules of the tufted angiomas consist of closely packed blood capillary endothelial and perithelial cells.
The patient has been discharged the same day; no postoperative complications have occurred. After a follow-up of 6 months, the patient was in good condition without recurrences or symptoms, no pain or loss of function was referred.
Discussion
In 1987, Padilla et al. (9) described 20 patients with benign, progressive vascular lesions that had a distinctive histopathologic appearance. They termed these lesions tufted angioma. Previously, similar lesions had been described as “angioblastoma” or “angioblastoma of Nakagawa” in the Japanese literature (10,11); these are now considered by many to be identical to acquired tufted angioma because of similar histopathological features (4,9,12,13).
Most cases (60–70%) of tufted angiomas develop before the age of five years and fewer than 10% of cases with TA occur after the age of 50 years. There is no sex predilection (14).
Macroscopically, Tufted angioma presents with solitary slowly spreading erythematous macules and papules (8) with poorly defined borders. The diameter of the patches generally ranges from less than 1 cm to several centimeters (1), with generally 2–10 cm size. Lesions progressively enlarge at a variable rate becoming more or less stable (2). Most commonly, it is localised to the skin and subcutaneous tissue (7), soft tissues of the trunk, shoulders, extremities, neck and head (14) and occasionally the proximal limbs (7). Involvement of other location like face, oral mucosa or lip are also know (5).
Microscopically, Tufted angioma has a classical morphology (5). It shows multiple scattered lobules or tufts having a cannonball appearance (7). The lesions are composed of multifocal, tightly packed knots or tufts of spindle and polygonal cells associated with endothelial cells (2). Tufted angioma and KHE (Kaposi Hemangioendothelioma) share several histopathologic and clinical features, that include the presence of glomeruloid structures and a lymphatic network and are thought to be part of the same neoplastic spectrum.
The pathogenesis of Tufted angiomas is not well understood. Vascular markers (CD31 and CD34), vascular endothelial growth factor receptor-3 (VEGFR-3), and lymphatic markers (D2-40 and PROX1) on the neoplastic cells suggest they may be derived from the endothelial cells of lymphatic vessels.
Cell marker studies suggest that the cell lobules of the angiomas consist of closely packed blood capillary endothelial and perithelial cells (4). The presence of endothelial cells and of Weibel-Palade bodies is confirmed by ultrastructural studies (2). Endothelial cells show reactivity for markers as CD31, CD34 AND Von Willebrand factor (factor VIII) (5). In TA, D2-40 is partially positive in the surrounding dilated vessels and negative in cannonball-like proliferative capillaries (15). The surrounding spindle and polygonal cells may show few cytofilaments or focal condensations of microfilaments Pericytes that surround the capillaries are the principal cells of Tufted angioma (5). The tufts may form capillaries. Dense fibrous connective tissue separates these lobules of cells TA has a slow and progressive growth, nevertheless malignant transformation has not been reported by follow-up studies (8), even if it could be local aggressive (16).
Sometimes, lesions can be surmounted by nodular formations. Occasionally, the lesions start or persist as small dusky red-to-violaceous large infiltrated plaque, that can be indurated and firm (17). Most of the lesions are asymptomatic (5), but they can be associated with hypertrichosis or hyperhidrosis (15), with the last one that occurs in 30% of patients (7).
Tufted angioma can also have the shape of tender lesions (18). Cases with spontaneous regression have been reported, commonly occurring when onset is before six months of age (7). Tufted angioma it can also show transient spontaneous regression between 6 months and 2 years or it can completely disappear (19). One particular case presented as recurrent acquired tufted angioma associated with pregnancy that disappeared after childbirth (20), and another one developed after liver transplant which regressed spontaneously (2). When the onset is later than six months of age, partial spontaneous regression of TA may occur, but complete disappearance is extremely rare (7).
The most serious complication of Tufted angioma is the Kasabach-Merritt phenomenon, a life-threatening coagulopathy that causes thrombocytopenia, consumption of fibrinogen and other coagulation factors. In those patient Tufted angioma are symptomatic, show an infiltrative pattern and have a poor cosmetic outcome (21). In this setting, the presence of petechial and ecchymotic patches should alert the physician to the development of KMS (1).
Persistent TA requires treatment. Treatment guidelines for Tufted angioma have not been laid out yet. Medical treatments such as corticosteroids, interferon-α and laser therapy have all shown variable treatment outcomes. However, the small size of mucosal TA yields well to surgical excision.
Moderate- to high-dose gluco-corticoids were considered the main therapy for Kasposiform hemoangioendothelioma and Tufted angioma (KHE/TA); however, these steroids are associated with poor response rates and multiple short-term/long-term side effects (22) such as Cushing Syndrome or opportunistic infections. Vincristine (VCR), an inhibitor of endothelial proliferation, is a promising pharmaco-therapeutic approach for treating KHE/TA, especially for steroid-resistant KHE. Large clinical trials have demonstrated the effectiveness of VCR in treating KHE. Other treatment modalities including interferon, radio-therapy, embolization, anti-platelet agents (aspirin), propranolol and sirolimus, which have been used alone or in combination are reserved as second- or third-line therapies. Nevertheless, none of the treatments mentioned above has been reported to have a uniform and reproducible effect. Xiao Han Liu et. Al conducted a meta-analysis of 15 clinical studies compared different therapies for KHE/TA. The findings demonstrated that vincristine was relatively more effective compared with other therapies, including systemic corticosteroids, interferon, radiotherapy, embolization, aspirin/ticlopidine and sirolimus.
Over 70% of KHE and TA cases are associated with Kasabach-Merritt syndrome or phenomenon (KMS or KMP), a life-threatening constellation of thrombocytopenia, coagulopathy and purpura with a mortality of 20%. Thus, enlarging tumours and tumours with KMP often require early interventions. Given the rarity of KHE/TA, there is presently no evidence-based standard therapy for the disease (23).
Conclusions
TA is a rare vascular neoplasm, localized in skin and subcutaneous tissue. The true incidence of Tufted Angioma is still unknown, because not all cases come to medical observation. It can be congenital or acquired, generally associated with immunodeficiency in adults. There is still much to know about this neoplasm, starting from predisposing factors and triggering factors that seem to differ in different age groups. The phenomenon of spontaneous regression that has been found in pediatric forms could suggest the presence of growth factors necessary for tumor development that are more common in developing organisms than in adulthood. However, the phenomenon of regression of Tufted Angiomas remains unexplained. Cases of Tufted angiomas diagnosed in adulthood are very rare. Nowadays immunodepression is considered one of the factors able to predispose some acquired forms. We suggest that the higher incidence in immunosuppressed patients could be indicate a possible viral involvement at the base of the phenomenon of tumorigenesis which at the moment is still unknown. Traumatism does not seem to have a major role in the formation of angioma; indeed we found only one case in the literature reported by Pesapane et al. which describes the development of a Tufted angioma on the site of a previous bite of an arthropod. There is not an evidence-based standard therapy for this disease. The various options include the use of glucocorticoide, VCR, Interferon, ASA administration or RT and embolization use.
In our case report, we have used surgery to treat a vascular lesion that was found to be a TA after histological examination, without recurrence or complications after a 6 months follow-up. As we reported in our review, surgery can be the main therapy for small, single TA. In these cases surgery offers a long term healing without side effect, loss of function or important aesthetic damages.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient to publish this manuscript and any accompanying images.
References
- Pesapane F, Nazzaro G, Alberti-Violetti S, et al. A case of acquired tufted angioma in adulthood. An Bras Dermatol 2015;90:16-8. [Crossref] [PubMed]
- Daley T. Acquired Tufted Angioma of the Lower Lip Mucosa. J Can Dent Assoc 2000;66:137. [PubMed]
- Al-Za'abi AM, Ghazarian D, Greenberg GR, et al. Eruptive tufted angiomas in a patient with Crohn’s disease. J Clin Pathol 2005;58:214-6. [Crossref] [PubMed]
- Jones EW, Orkin M. Tufted angioma (angioblastoma). A benign progressive angioma, not to be confused with Kaposi's sarcoma or low-grade angiosarcoma. J Am Acad Dermatol 1989;20:214-25. [Crossref] [PubMed]
- Mittal R, Tripathy D. Tufted angioma (Angioblastoma) of eyelid in adults-report of two cases. Diagn Pathol 2013;8:153. [Crossref] [PubMed]
- Heagerty AH, Rubin A, Robinson TW. Familial tufted angioma. Clin Exp Dermatol 1992;17:344-5. [Crossref] [PubMed]
- Prasuna A, Rao PN. A tufted angioma. Indian Dermatol Online J 2015;6:266-8. [Crossref] [PubMed]
- Vanhooteghem O, André J, Bruderer P, et al. Tufted angioma, a particular form of angioma. Dermatology 1997;194:402-4. [Crossref] [PubMed]
- Padilla RS, Orkin M, Rosai J. Acquired "tufted" angioma (progressive capillary hemangioma). A distinctive clinicopathologic entity related to lobular capillary hemangioma. Am J Dermatopathol 1987;9:292-300. [Crossref] [PubMed]
- Hiroto F. Angioblastoma. In: XVI Congressus Internationalis Dermatologiae. Tokyo, Japan: University of Tokyo Press; 1982:149.
- Kazuhiko N. Case report of angioblastoma of the skin. Jpn J Dermatol 1949;59:92-4.
- Chu P, LeBoit PE. An eruptive vascular proliferation resembling acquired tufted angioma in the recipient of a liver transplant. J Am Acad Dermatol 1992;26:322-5. [Crossref] [PubMed]
- Alessi E, Bertani E, Sala F. Acquired tufted angioma. Am J Dermatopathol 1986;8:426-9. [Crossref] [PubMed]
- Verma J, Singh A, Misra V, et al. Tufted Angioma of Eyelid in an Adult- A case Report. J Clin Diagn Res 2016;10:ED12-3. [PubMed]
- Arai E, Kuramochi A, Tsuchida T, et al. Usefulness of D2-40 immunohistochemistry for differentiation between kaposiform hemangioendothelioma and tufted angioma. J Cutan Pathol 2006;33:492-7. [Crossref] [PubMed]
- D'Amico RS, Zanazzi G, Hargus G, et al. Intracranial intraaxial cerebral tufted angioma: case report. J Neurosurg 2018;128:524-9. [Crossref] [PubMed]
- Osio A, Fraitag S, Hadj-Rabia S, et al. Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol 2010;146:758-63. [Crossref] [PubMed]
- Chiu CS, Yang LC, Hong HS, et al. Treatment of a tufted angioma with intense pulsed light. J Dermatolog Treat 2007;18:109-11. [Crossref] [PubMed]
- Ishikawa K, Hatano Y, Ichikawa H, et al. The spontaneous regression of tufted angioma - A case of regression after two recurrences and a review of 27 cases reported in the literature Article Literature Review. Dermatology 2005;210:346-8. [Crossref] [PubMed]
- Kim YK, Kim HJ, Lee KG. Acquired tufted angioma associated with pregnancy. Clin Exp Dermatol 1992;17:458-9. [Crossref] [PubMed]
- Adams D, Frieden IJ. Tufted angioma, kaposiform hemangioendothelioma, and the Kasabach-Merritt phenomenon. Available online: https://www.uptodate.com/contents/tufted-angioma-kaposiform-hemangioendothelioma-and-the-kasabach-merritt-phenomenon
- Liu X, Li J, Qu X, et al. Clinical Outcomes for Systemic Corticosteroids Versus Vincristine in Treating Kaposiform Hemangioendothelioma and Tufted Angioma. Medicine (Baltimore) 2016;95:e3431. [Crossref] [PubMed]
- Liu XH, Li JY, Qu XH, et al. Treatment of kaposiform hemangioendothelioma and tufted angioma. Int J Cancer 2016;139:1658-66. [Crossref] [PubMed]
Cite this article as: Fabbri N, Quarantotto F, Caruso A, Montinari E, Rubino S, Tamburini N, Maniscalco P, Cavallesco G. Surgical excision of a tufted angioma of the hand in an adult—a rare case report with a review of literature. AME Case Rep 2019;3:7.