
Bronchovascular sleeve resection of the right middle lobe in N1 lung cancer
Introduction
Sleeve lobectomy is a useful procedure for preserving postoperative lung function. In combination with vascular reconstruction, this procedure may further reduce the need for bi-lobectomy and pneumonectomy. However, the operative technique and the tips on how to perform bronchovascular sleeve resection (BVSR) of the right middle lobe are minimally described in textbooks and the literature.
Case presentation
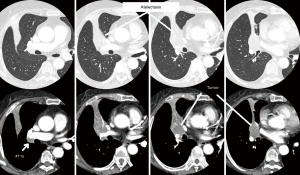
A 76-year-old woman was referred because of a 4.5-cm mass in the right middle lobe, seemed to involve the interlobar pulmonary artery (PA) with metastatic #11s lymph nodes radiographically (Figure 1), and a 2.0 cm mass in the left upper lobe. Simultaneous multiple squamous cell lung carcinomas were diagnosed: clinical T2aN1 (#11s) M0 stage IIB in the right middle lobe and T1bN0M0 stage IA2 in the left upper lobe. There were several comorbidities: the patient was a current heavy smoker and had ischemic heart disease and autoimmune enterocolitis. Because of the lung cancer stage, the right side should be treated first. Bi-lobectomy of middle and lower lobes would be appropriate for this situation. However, if it had been performed, the residual right lung function would not be adequate to assure treatment of the left side or maintenance of the quality of life after bilateral treatment. Thus, BVSR of the right middle lobe was planned.
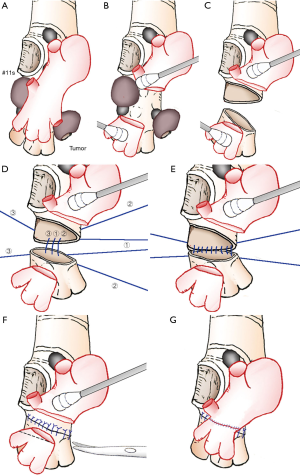
The video starts with a view of dissecting the superior pulmonary vein (PV) inside and outside the pericardium to preserve the PV from the upper lobe (Figure 2). The lower lobe PA was exposed at the level of the major fissure. After clamping the main PA followed by the superior and inferior PV without heparin administration, the interlobar PA could be divided and was not involved by tumor. However, the #11s lymph nodes invaded the wall of the bronchus intermedius, and the main tumor involved the central part of the middle lobe bronchus and anterior side of the bronchus intermedius. The length of cutting the bronchus was very long, and it was necessary to manipulate the invaded bronchus intermedius under better exposure. To obtain better exposure, the interlobar PA was transected (Figure 3A,B). The bronchus intermedius was cut off on the proximal side at the end of the upper lobe bronchus, including the underside of the bronchus to ensure an adequate surgical margin, and on the distal side along only the lower lobe bronchus inlet. The middle lobe with part of the bronchus intermedius was removed (Figure 3C). Intraoperative frozen sections were negative for tumor. An anastomosis was performed with interrupted 4-0 PDS sutures. Three threads were placed first (Figure 3D), and the center one was ligated. Another thread was placed, and the deeper one was then ligated. This maneuver was alternatively performed half way (Figure 3E), and then all threads were initially placed and ligated. After the sealing test, the interlobar PA was trimmed (Figure 3F) and anastomosed with 5-0 Prolene (Figure 3G). First, a running suture was continuously performed on the deeper side, and the superficial side was sutured later without turning over the PA. Flushing of the PA before finishing anastomosis was done with saline with heparin. No tissue interposition between the anastomosed PA and bronchus was used because the gap was so tight that it might cause kinking of the anastomosed PA. After that, mediastinal lymph node dissection was performed.
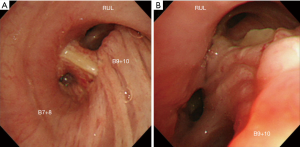
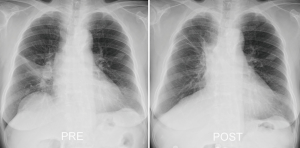
The total occlusion time of the PA was 47 minutes including bronchial anastomosis. The operation time was 307 minutes, and the blood loss was 200 mL. The postoperative course was uneventful, including the anastomotic site (Figure 4). Good expansion of the right lung was obtained (Figure 5). The pathological disease stage was T2aN1(#11s) M0 stage IIB. Two months after surgery, the patient refused upper division segmentectomy under video-assisted thoracoscopic surgery to treat the left-side cancer, and stereotactic radiotherapy was thus delivered. Even after completion of all treatments, the patient’s quality of life was well maintained.
Comments
Sleeve lobectomy is a useful procedure for preserving the lung parenchyma in lung cancer. The oncologic outcomes of this procedure have been reported to be noninferior to those of pneumonectomy, even in patients with N1 lung cancer (2). Of course, postoperative lung function will be maintained better than that after pneumonectomy, greatly contributing to the postoperative quality of life (3). If the tumor also involves the pulmonary artery, it is necessary to simultaneously perform vascular reconstruction. In such patients, bi-lobectomy of the middle and lower lobes is likely to be selected when only the right side is involved. However, when another contralateral lung cancer needs to be treated, and multiple comorbidities are recognized, the lung function of the right side should be preserved as much as possible. Fortunately, there were no postoperative complications, and the left side cancer was treated on schedule. Even after completing treatment of both sides, the patient’s quality of life was maintained well; the selection of this procedure seemed to be appropriate. For thoracic surgeons, it is important to be aware that this technique is rarely performed in daily practice. In 2011, only 403 (1.2%) sleeve lobectomies were performed in Japan (4). A meta-analysis of sleeve lobectomy showed that the outcomes of BVSR were similar to those of sleeve resection, with equivalent safety (5). In a previous study, BVSR was performed in only 78 (8.9%) of 876 patients who underwent sleeve lobectomies. In a large study of 213 patients who underwent sleeve lobectomies and BVSR, BVSR of the middle lobe was not performed in any patient (6). Our experience with bronchoplasty indicates that the calibers of both bronchi were large, and the difference in the calibers of the bronchi was minimal; needle maneuvers were therefore not difficult to perform. However, with respect to vascular reconstruction, as the bronchus was shortened, the length of PA became so long that trimming of the PA was required. We cut the lower lobe PA diagonally to adjust the caliber to that of the cranial-side PA. If the anastomosed PA was too long, kinking might occur. These points seemed to be very important in this procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ito H, Nakayama H, Nagashima T, et al. Bronchovascular sleeve resection of the right middle lobe. Asvide 2019;6:045. Available online: http://www.asvide.com/article/view/30032
- Berry MF, Worni M, Wang X, et al. Sleeve lobectomy for non-small cell lung cancer with n1 nodal disease does not compromise survival. Ann Thorac Surg 2014;97:230-5. [Crossref] [PubMed]
- Ferguson MK, Lehman AG. Sleeve lobectomy or pneumonectomy: optimal management strategy using decision analysis techniques. Ann Thorac Surg 2003;76:1782-8. [Crossref] [PubMed]
- Amano J, Kuwano H, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2011: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2013;61:578-607. [Crossref] [PubMed]
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [Crossref] [PubMed]
- Nagayasu T, Yamasaki N, Tsuchiya T, et al. The evolution of bronchoplasty and broncho-angioplasty as treatments for lung cancer: evaluation of 30 years of data from a single institution. Eur J Cardiothorac Surg 2016;49:300-6. [Crossref] [PubMed]
Cite this article as: Ito H, Nakayama H, Nagashima T, Samejima J. Bronchovascular sleeve resection of the right middle lobe in N1 lung cancer. AME Case Rep 2019;3:5.


