Postoperative hemorrhage after right upper lobectomy associated with apixaban use: a case report
Introduction
Direct oral anticoagulants (DOACs) are a new class of drugs that are better at preventing thromboembolisms (1). DOACs guarantee better handling and do not require strict and frequent laboratory monitoring or dosing adjustments (1). DOACs are currently used in many patients with atrial fibrillation. However, there are no indicators for their anticoagulant effect, and there are some unclear points about safety associated with their use, as there are limited clinical data available after their release. Moreover, if hemorrhage occurs, there is no established treatment guideline for controlling bleeding in patients treated with DOACs. We experienced a patient who was considered to have postoperative hemorrhage related to apixaban use after right upper lung lobectomy for lung cancer.
Case presentation
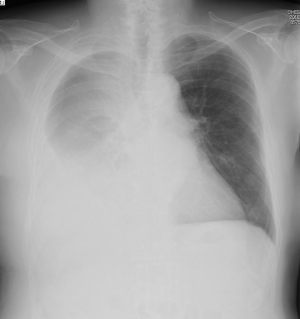
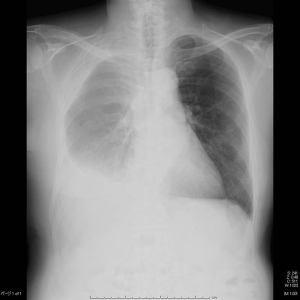
A 76-year-old man with atrial fibrillation and a history of myocardial infraction was admitted to our hospital for undergoing operation for lung cancer. He had been treated with apixaban (5 mg twice daily). His preoperative body weight was 63.5 kg, and his creatinine level was 0.88 mg/dL. We stopped his apixaban use 3 days before surgery. Then we performed right upper lobectomy and lymph node resection (ND2a-1). The operative time was 3 hours 25 minutes, and total blood loss was 449 mL because a #10 lymph node adhered strongly to the main pulmonary artery, which made lobectomy and lymph node resection difficult (pT3N1M0 stage IIIA, adenocarcinoma). However, his postoperative course was uneventful, and his thoracic drain, which showed no hemorrhage or air leakage, was removed on the second postoperative day (POD). His hemoglobin levels were 15.3 g/dL preoperatively, 13.5 g/dL on POD1, and 13.5 mg/dL on POD7. At that point, the chest X-ray showed no major abnormal findings (Figure 1). He was discharged from the hospital 9 days postoperatively. On POD10, apixaban was restarted. On POD18, he was evaluated as an outpatient. He complained of fatigue, and his hemoglobin level had decreased to 8.5 mg/dL. The chest X-ray showed right pleural fluid (Figure 2), and his right chest wall was swollen. His vital signs showed no change. We considered the condition to be postoperative hemorrhage associated with apixaban use. We stopped apixaban immediately, and performed puncture of the thoracic cavity with a 14-gauge catheter to confirm the property of the pleural effusion, and we removed about 400 mL of bloody pleural effusion. The effusion was bloody with a hemoglobin level of 3.8 g/dL. We diagnosed this as a postoperative bleeding complication and administered an infusion of 560 mL of red blood cells. Computed tomography after puncture of the thoracic cavity showed massive right pleural effusion and subcutaneous hematoma (Figure 3). We considered that postoperative bleeding had occurred in the thoracic cavity and subcutaneous area. A few days later, his subcutaneous bleeding trace became gradually clear (Figure 4). The patient had no further bleeding after stopping apixaban, and he was discharged on POD30 (Figure 5).

Discussion
In this report, we described a patient who was considered to have postoperative hemorrhage related to apixaban use after right upper lung lobectomy for lung cancer. The frequency of postoperative hemorrhage in lung lobectomy is not very high, and 0.3–1.8% of patients with lung lobectomy require blood transfusion (2-4). The bleeding points of postoperative hemorrhage in lung lobectomy include the thoracotomy wound site, port site, adhesiotomy site, pulmonary arteriovenous ligation site, lymph node dissection site, and so on (5). In the present case, we could not confirm the bleeding point. However, considering that the progression of anemia was relatively slow, his condition was relieved only by stopping DOACs and after red blood cell transfusion, and since bleeding occurred in the intrathoracic cavity and subcutaneous site at the same time, it was less likely that rupture of the treated blood vessels had occurred. We think that the bleeding occurred from a wound area or the lymph node dissection site. We injured the pulmonary artery intraoperatively; however, the injury was not severe. We were able to control the bleeding by only applying pressure to the bleeding point, and then we covered the bleeding point with a TachoSil tissue-sealing sheet. Blood loss associated with this injury was not substantial, so we do not think the injury was related to postoperative bleeding.
Compared to warfarin, DOACs have faster absorption, a shorter half-life, and less drug interaction and are not affected by food (6). The predictable anticoagulant effects of DOACs enable the administration of fixed doses without the need for routine coagulation monitoring, thereby simplifying treatment (7). According to a meta-analysis of large-scale clinical trials targeting atrial fibrillation, DOACs as a whole as compared to warfarin tend to be excellent in stroke prevention and safety of major bleeding (7,8). With the aging of surgical patients, the proportion of patients using DOACs in the perioperative period is expected to be high.
On the other hand, problems such as prevention of bleeding complications, emergency countermeasures, and management in the perioperative period have been pointed out (6). In 2015, the United States Food and Drug Administration approved idarucizumab as a reversal agent for dabigatran. However, there are no known agents for reversing bleeding in patients receiving rivaroxaban, apixaban, and edoxaban. Furthermore, in the clinical setting, the magnitude of the bleeding risk that is associated with DOACs remains unclear (9). There are few reports of perioperative bleeding events with DOACs, and there is no established treatment guideline for controlling bleeding complications associated with DOACs; therefore, clinical judgment about bleeding associated with the use of DOACs is difficult. Only one case of a bleeding complication after lung lobectomy associated with DOACs has been reported by Kuwata et al. (10). However, with aging of patients and widespread use of DOACs, we consider that cases of bleeding complications like ours will increase.
Aspirin was also used in our case because stent therapy for myocardial infraction was performed about a year earlier. Thus, the possibility that the combined use of aspirin and apixaban promoted postoperative hemorrhage cannot be denied. Low-dose aspirin alone does not substantially increase the risk of clinically important bleeding after invasive procedures (11). However, the risk of intracranial hemorrhage is increased with the combined use of DOACs and antiplatelet agents (12,13). In this case, it was considered that the combined use of an anticoagulant with aspirin may have increased the risk of bleeding.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hassan K, Bayer N, Schlingloff F, et al. Bleeding Complications After Use of Novel Oral Anticoagulants in Patients Undergoing Cardiac Surgery. Ann Thorac Surg 2018;105:702-8. [Crossref] [PubMed]
- Daniels LJ, Balderson SS, Onaitis MW, et al. Thoracoscopic lobectomy: a safe and effective strategy for patients with stage I lung cancer. Ann Thorac Surg 2002;74:860-4. [Crossref] [PubMed]
- McKenna RJ Jr, Wolf RK, Brenner M, et al. Is lobectomy by video-assisted thoracic surgery an adequate cancer operation? Ann Thorac Surg 1998;66:1903-8. [Crossref] [PubMed]
- Asamura H, Kawachi R, Oyama M, et al. Estimation of the volume of postoperative intrathoracic bleeding after pulmonary resection: Is the volume of chest tube output predictive of that of intrathoracic hematoma? J Jpn Assoc Chest Surg 2011;25:696-701. [Crossref]
- Fujino S, Okumura T, Watanabe M. Postoperative bleeding. Jpn J Chest Dis 2013;72:708-16.
- Yasaka M, Okada Y. Several issues accompanied by novel oral anticoagulants. Nosotchu 2013;35:121. [Crossref]
- Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 2014;383:955-62. [Crossref] [PubMed]
- Yamashita T. The Cutting-edge of Medicine: New era of anticoagulation. Nihon Naika Gakkai Zasshi 2016;105:2245-50. [Crossref] [PubMed]
- Yagyuu T, Kawakami M, Ueyama Y, et al. Risks of postextraction bleeding after receiving direct oral anticoagulants or warfarin: a retrospective cohort study. BMJ Open 2017;7. [Crossref] [PubMed]
- Kuwata T, Kanayama M, Hirai A, et al. Postoperative thoracic hemorrhage after right upper lobectomy with thoracic wall resection during rivaroxaban anticoagulant therapy for deep leg vein thrombosis: A case report. Int J Surg Case Rep 2017;41:340-2. [Crossref] [PubMed]
- Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med 2013;368:2113-24. [Crossref] [PubMed]
- Hankey GJ. Intracranial hemorrhage and novel anticoagulants for atrial fibrillation: what have we learned? Curr Cardiol Rep 2014;16:480. [Crossref] [PubMed]
- Takenaka T, Shibano K, Umegamki M, et al. Surgical Treatment of Traumatic Intracranial Hemorrhage in Patients with Novel Oral Anticoagulant (NOAC) Administration: A Report of Three Cases. Jpn J Neurosurg 2015;24:327-33. [Crossref]
Cite this article as: Ema T, Neyatani H, Yamamoto S, Iizuka S, Funai K, Shiiya N. Postoperative hemorrhage after right upper lobectomy associated with apixaban use: a case report. AME Case Rep 2018;2:46.