Hiding in the bone: a case of miliary tuberculosis with bone marrow involvement
Introduction
Dissemination of tuberculosis is known as miliary tuberculosis. It can present from first to seventieth year of life. The onset is insidious with weight loss and weakness being the most common constitutional symptoms. Clinical signs are also inconsistent and vary in patients. Bone marrow involvement is rare. Our case highlights the importance of considering tuberculosis dissemination in patients who present with extra pulmonary manifestations in order to start treatment in a timely manner.
Case presentation
Patient is a 74-year Caucasian male with the past medical history of diabetes mellitus, CKD-3 and chronic obstructive pulmonary disease (COPD) presented to hospital with complain of generalized weakness and low-grade fevers which started for the last couple of weeks. His average fever had been around 100–101 F. He also complained about decreased appetite, trouble with his balance and some back pain. Otherwise, he denied any headache, night sweats, cough, chest pain, sob, abdominal pain or any bowel changes, sick contacts or any travel outside the United States. The patient was seen recently seen by the primary care with the same complain and was recommended a 10-day course of doxycycline for possible atypical pathogen causing pyrexia of unknown origin (PUO). However, the patient continued having persistent low-grade fevers. The patient also had a concern for transaminitis in the recent past, however, testing for hepatic viral markers, leptospirosis, babesiosis, Lyme and anaplasmosis came back negative.
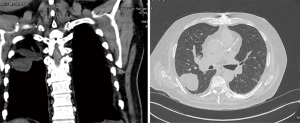
On presentation, he had a temperature of 99.9 with fair pressures and saturation on room air. The physical examination was benign except decreased breathing sounds with inspiratory and expiratory rhonchi. The lab workup revealed pancytopenia with white blood cell count (WBC) 2.2, Hgb 7.1 and platelets 31. The lactate dehydrogenase (LDH) was also elevated. Blood, respiratory and fungal cultures taken didn’t grow any organisms. Plain chest X-ray did not reveal any active pulmonary infiltrates. A computed tomography (CT) chest (Figure 1) does reveal multiple centrilobular nodules in the upper lung zone predominant distribution as seen in the images below.
The autoimmune workup and pan-cultures were negative. There was a suspicion for tuberculosis and workup revealed negative acid-fast bacilli (AFB) but positive QuantiFERON-tuberculosis with a Nil tube value of <8.0 IU/mL. The patient was immediately put on airborne isolation. Pulmonology was consulted and patient underwent bronchoscopy which was unremarkable for any endobronchial lesion. Patient was also discussed with the Infectious diseases and Oncology team for the concern of ongoing pancytopenia. The peripheral blood smear (PBS) showed normocytic anemia with anisocytosis, absolute lymphopenia and thrombocytopenia. Later, the bone marrow biopsy was done which showed hypercellular marrow with well-formed epithelioid granulomas having central caseating necrosis as seen in the H/P images below (Figure 2).
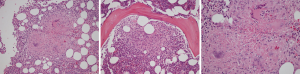
Patient was diagnosed with miliary tuberculosis with bone marrow involvement which is very rare. It was determined to be the cause of pancytopenia. The anti-tuberculosis treatment was started for a 6-month of total duration of therapy. After the successful treatment of tuberculosis, patient blood count improved to the normal limit.
Discussion
There has been a significant decline in the incidence rate of tuberculosis due to early diagnosis and treatment, however extra pulmonary tuberculosis has remained unchanged due to delay in the recognition of the disease pattern secondary to uncommon presentation (1). Miliary tuberculosis is diagnosed by presence of diffuse miliary infiltrates in lungs on chest imaging. However, imaging does not always show classical signs. Therefore, a high degree of clinical suspicion and systematic approach is needed to establish the diagnosis of miliary tuberculosis. In our patient chest X-ray didn’t show the disease focus and skin test have not been reported helpful for miliary tuberculosis diagnosis either (2).
The disease can present with various patterns including hematological abnormalities. It rarely causes pancytopenia. There has been different hypothesis to explain pancytopenia in miliary tuberculosis which include hypersplenism, histiocytic hyperplasia (3), and maturation arrest during the development phase of the cells. The possibility of infiltration of the bone marrow by granulomatous pattern leading to fibrosis is also present (4). However, it is very rare and incidence ranges from 0.4% to 2% (5).
The mortality rate and prognosis has been reported in literature in different ranges. In contrast the localized disease process of the lungs, miliary tuberculosis carries high mortality rate. One of the retrospective study showed the mortality rate of 50% (6). The explanation in this study for high mortality was late presentation. Other factors include, but not limited to, disease severity, immunocompetent status of the patient and macrophage-activating syndrome. Our patient presented with very quick improvement without any long-term complication which probably was because of the initial stage of the disease, early diagnosis with good compliance and follow up.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Verbal informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Le Hô H1. Barbarot N, Desrues B. Pancytopenia in disseminated tuberculosis: Think of macrophage activation syndrome. Rev Mal Respir 2010;27:257-60. [PubMed]
- Sharma SK, Mohan A, Sharma A, et al. Miliary tuberculosis: new insights into an old disease. Lancet Infect Dis 2005;5:415-30. [Crossref] [PubMed]
- Avasthi R, Mohanty D, Chaudhary SC, et al. Disseminated tuberculosis: interesting hematological observations. J Assoc Physicians India 2010;58:243-4. [PubMed]
- Kuo PH, Yang PC, Kuo SS, et al. Severe immune hemolytic anemia in disseminated tuberculosis with response to antituberculosis therapy. Chest 2001;119:1961-3. [Crossref] [PubMed]
- Singh KJ, Ahluwalia G, Sharma SK, et al. Significance of haematological manifestations in patients with tuberculosis. J Assoc Physicians India 2001;49:788-790-4. [PubMed]
- Eid A, Carion W, Nystrom JS. Differential diagnoses of bone marrow granuloma. West J Med 1996;164:510-5. [PubMed]
Cite this article as: Tahir M, Nida A, Qamar S. Hiding in the bone: a case of miliary tuberculosis with bone marrow involvement. AME Case Rep 2018;2:36.