A rare case report of leiomyosarcoma of tongue
Introduction
Primary leiomyosarcoma of tongue is an extremely rare mesenchymal malignancy with a high recurrence rate and metastatic potential. Barnes et al. reported that the most common sites of head and neck regions are the oral cavity (22%), the sino-nasal tract (19%) and the facial subcutis (17%) (1). Among the oral cavity, buccal mucosa is the common site and tongue is a very rare site. We report a case of leiomyosarcoma of tongue which had poor prognosis and died within 8 months of diagnosis.
Case presentation
A 45-year-old female known tobacco chewer presented to us with unable to open mouth for 1 year and mass tongue for 1 month. The mass was painless and small initially but gradually increase in size along with increasing pain which was radiating to ear. On examination mouth opening was one finger (trismus grade III). There was extensive submucosal fibrosis and visible proliferative growth at left lateral boarder of the tongue. Rest of the oral cavity appeared normal. Multiple sub-centimeter lymph nodes were present at left level Ib and level II.
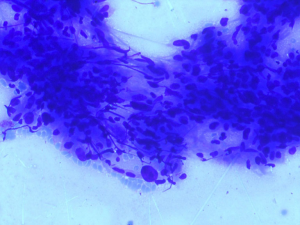
Fine needle aspiration cytology of the mass revealed high-grade mesenchymal lesion of the tongue (Figure 1). Contrast enhanced computed tomography (CECT) of face, neck and chest was done, which revealed the growth localized to the lateral boarder of anterior tongue, not crossing midline with multiple enlarged neck nodes. Naso-pharyngo-laryngoscopy revealed no abnormality. Other metastatic work up recommended was within normal limits.
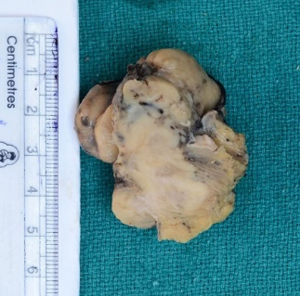
The surgery was planned as first line of treatment. After tracheostomy, oral cavity was accessed through midline mandibulotomy. Wide local excision of the tongue lesion with a margin minimum of 1 cm along with neck dissection was done (Figure 2). The post-operative period was uneventful and was discharged on 4th post-operative day.
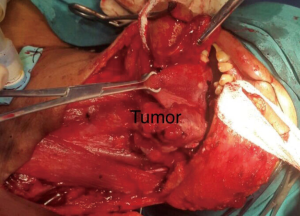
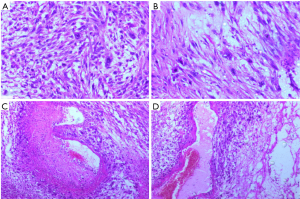
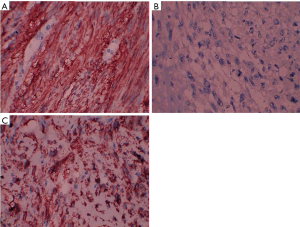
Grossly tumor measured 2 cm × 1.5 cm × 0.5 cm (Figure 3). Histopathological examination of the tumor showed predominantly spindle cell with eosinophilic fibrillary cytoplasm arranged in fascicles. The individual cell exhibited pleomorphism. Mitosis was 6-8/HPF (Figure 4A,B). Necrosis was evident focally (Figure 4C). Peritheliomatous arrangements, bizarre cells and tumor giant cells were also seen (Figure 4D). Total 30 nodes were dissected and all of them were free of tumor. Depth of invasion was 3 mm. Nearest margin was 1 cm. Immunohistochemistry was done on tumor tissue. It was found to be positive for desmin (Figure 5A), negative for cytokeratin (CK) (Figure 5B) and positive for smooth muscle actin (Figure 5C). The final diagnosis rendered was leiomyosarcoma on the basis of above findings.
Adjuvant radiotherapy was advised. She received 60 gray (30 fractions) radiotherapy over 6 weeks. She was kept on regular follow-up every 3 months. On 2nd follow-up (6 months after treatment), she had multiple soft tissue mass whole over neck (Figure 6). Fine needle aspiration cytology (FNAC) of mass revealed the features of metastatic leiomyosarcoma.
She was advised palliative chemotherapy, but she refused to take due to financial constraint. She was on supportive therapy and succumbed to the disease on 8th month of post-surgery.
Discussion
Leiomyosarcoma is a highly aggressive tumor arising from the smooth muscle. Due to paucity of smooth muscle in head and neck areas, it occurs rarely at this site (2). Enzinger and Weiss opined that it arises from smooth muscle lining of vascular wall (3). Primary leiomyosarcoma of tongue is a very rare tumor. A very few cases have been reported in the literature. Morphologically it resembles the spindle cell carcinoma, variant of squamous cell carcinoma. Therefore, it poses a diagnostic challenge for the histopathologist. But proper evaluation of multiple sections of tumor and immunohistochemistry help in confirming the correct diagnosis. Spindle cell carcinoma is CK positive and desmin negative whereas leiomyosarcoma is CK negative and desmin positive (4,5). The tumor is seen arising from squamous epithelium in carcinoma and keratinisation can be seen at focal areas. But the epithelium doesn’t reveal any dysplastic changes in sarcoma and lack keratinisation.
Verma and Ethunandan (2,6,7) have reported the same case and have concluded that the only effective treatment is complete resection with free margin and postoperative radiotherapy when necessary. Chemotherapy was recommended in cases with inoperable and metastatic disease (8).
In the present case, the patient had undergone surgery and was advised adjuvant radiotherapy irrespective of small tumor size and negative neck nodes with minimal depth of invasion based on aggressive nature of the disease. The adjuvant radiotherapy was completed in stipulated time. In spite of the adequate treatment, the patient developed metastasis of soft tissue and skin within 6 months of treatment. This case highlights that leiomyosarcoma has very poor prognosis and survival rate. We should be aware of this entity and further research is needed to document the proper protocol and guidelines of the treatment.
Acknowledgements
The authors would like to thank Shankar Agarwal (Director of Pushpadi Cancer Care Centre) and Tilak Raj Verma (Nursing staff of Pushpadi Cancer Care Centre).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the children of patient for publication of this case report and any accompanying images.
References
- Barnes L. editor. Surgical pathology of the head and neck. New York: Marcel Dekker, 1985:814-21.
- Verma M, Lal P. Leiomyosarcoma of tongue: A case report and review of literature. Asian J Oncol 2016;2:82-4. [Crossref]
- Enzinger FM, Weiss SW. editors. Soft tissue tumors. St. Louis, MO: Mosby Year Book Inc., 1995:491-510.
- Piattelli A, Artese L. Leiomyosarcoma of the tongue: a case report. J Oral Maxillofac Surg 1995;53:698-701. [Crossref] [PubMed]
- Croce A, Moretti A, Laus M, et al. Leiomyosarcoma of the base of the tongue and free edge of the epiglottis: A case report. J Med Case Rep 2012;6:400. [Crossref] [PubMed]
- Ethunandan M, Stokes C, Higgins B, et al. Primary oral leiomyosarcoma: A clinico-pathologic study and analysis of prognostic factors. Int J Oral Maxillofac Surg 2007;36:409-16. [Crossref] [PubMed]
- Dhanasekaran SV, Nair JS, Joyce ME. Leiomyosarcoma of tongue. Chrismed J Health Res 2014;1:271-3. [Crossref]
- Wertheimer-Hatch L, Hatch GF 3rd. Tumors of the oral cavity and pharynx. World J Surg 2000;24:395-400. [Crossref] [PubMed]
Cite this article as: Agarwal M, Agarwal L, Mathur V, Khandelwal G. A rare case report of leiomyosarcoma of tongue. AME Case Rep 2018;2:13.