Know the name: acute epiploic appendagitis—CT findings and review of literature
Introduction
Acute epiploic appendagitis is a benign inflammatory process involving the appendages epiploicae which are found adjacent the tenia coli of the colon from caecum to rectosigmoid. This condition can often be mistaken for diverticulitis or acute appendicitis leading to unnecessary laparoscopy or other surgical interventions; however, unlike these other conditions, this is a disease process which can be treated with anti-inflammatory medication. Due to the elusive nature of the clinical presentation of acute epiploic appendagitis, it has only been diagnosed correctly preoperatively 2.5% of the time. We present two cases of epiploic appendagitis with classic computed tomographic (CT) findings with the educational objective of increasing awareness of this condition, with the hope of reducing potentially harmful and unnecessary surgical interventions.
Case presentation
Case 1
A 23-year-old male presented to the emergency department (ED) with acute right lower quadrant abdominal pain. The pain was described as achy in nature, does not radiate, and without aggravating or relieving factors. The patient reported associated nausea, but without vomiting or fever. A computed tomography (CT) scan was obtained in the ED, which demonstrated a hyperattenuating lesion along the right colon (Figure 1) compatible with epiploic appendagitis.

Case 2
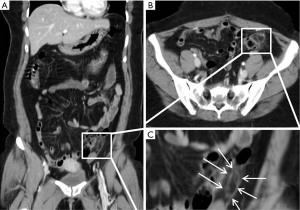
A 35-year-old female presented with acute left lower quadrant abdominal pain. The pain is described as moderate in severity, achy in nature. The patient reported associated nausea. The patient was found to have elevated white blood cell count in the ED. The working differential diagnosis at the time was diverticulitis or colitis. A CT scan obtained demonstrated an oval fat density with subtle hyperattenuating center (Figure 2).
Discussion
Appendage epiploicae are pedunculated peritoneal outpouchings consisting of adipose tissue and blood vessels. The appendages align themselves in anterior and posterior rows bordering tenia coli on the anti-mesenteric surface of the colon from cecum to the rectosigmoid colon (1-3). Variable in size (0.5–5 cm in length), shape, and location, their exact function remains unknown, although it has been postulated that the appendages may function as a blood reservoir, assist in colon absorption, provide cushioning, or protect against pathogens (1,4,5). However, there have been documented case of appendages >15 cm (1,4). They are found in groups of 50–100, the most substantial of which protrude off the sigmoid colon. Normal epiploic appendages remain indistinguishable from retroperitoneal fat on CT unless surrounded by inflammation or fluid (1).
A mechanical manipulation resulting in torsion or inflammation of these appendages can lead to venous and arterial constriction and subsequent ischemia and thrombosis (1). Therefore, torsion and inflammation are the leading causes of acute epiploic appendagitis (6). Acute epiploic appendagitis is often found in association with obesity, hernia, and exercise injury (7,8). It is most prevalent in patients in their 30–50 s with a higher frequency in males versus females (9).
The clinical presentation of acute epiploic appendagitis is strikingly similar to acute diverticulitis, with the hallmark manifestation of acute lower quadrant abdominal pain. However, acute epiploic appendagitis abdominal pain and tenderness is often localized to the affected area, unlike acute diverticulitis pain which is often diffuse (7,10). Due to the high frequency of sigmoid colon appendage involvement, the pain is often localized to the left lower side (11). Most frequently the pain has a rapid onset, is sharp and non-radiating, and may worsen with stretching of the abdomen or cough (12-14). Uncommonly, patients will experience changes in bowel movements, constipation, or diarrhea (6). Nausea, vomiting, appetite changes, and other associated symptoms are rare (15,16). Physical examination may be positive for rebound (10). Less than 30% of acute epiploic appendagitis cases may have an abdominal mass identifiable with palpation (6). Unlike acute diverticulitis, acute epiploic appendagitis will usually not cause changes in white blood cell count and body temperature (17). These patients will typically have normal vital signs and appear mildly ill (8). Lab work-up is generally unremarkable there may be a slight increase in inflammatory markers (9).
This benign condition is self-limited and most patients will see resolution of symptoms within two weeks (10). Conservative therapy without antibiotics is indicated with oral anti-inflammatories for pain management. In rare cases, acute epiploic appendagitis may lead to adhesion, bowel obstruction, intussusception, intraperitoneal loose body, peritonitis, and/or abscess formation (18). Patients should be closely monitored and encouraged to seek medical attention if symptoms worsen (15,16). In rare occurrence, patients who have recurrent acute epiploic appendagitis, surgery, preferably laparoscopic, may be necessary (9,19).
Due to the elusive nature of the clinical presentation of acute epiploic appendagitis, it has only been diagnosed correctly pre-operatively 2.5% of the time (6,7). Historically, acute epiploic appendagitis was encountered during surgery while searching for another cause of acute abdomen, such as appendicitis or diverticulitis. Imaging studies, used in conjunction with clinical judgment in the face of a germane patient presentation, are of critical importance to properly diagnose acute epiploic appendagitis in order to avoid unnecessary surgery or treatment. Most frequently acute epiploic appendagitis has been characterized using CT, but US and MRI have also been utilized.
On CT study, acute epiploic appendagitis consists of an oval lesion with fatty tissue attenuation that is commonly 1.5–3.5 cm in diameter, but no larger than 5 cm, lying adjacent to the anterior surface of the colon wall (7). The lesion is surrounded by a hyperattenuating ring, reflective of inflammatory changes. A central high attenuation region indicating venous thrombosis is frequently visualized (7). Occasionally, inflammation will cause parietal peritoneum thickening (1,7). Acute epiploic appendagitis rarely causes colonic wall thickening or occurs in hernia sacs, although Singh et al. documented the first case within an incisional hernia sac in 2004. Although symptoms should subside within weeks, CT changes are slower to occur, but will resolve by 6 months (20-22). Ultrasound imaging at the point of maximum tenderness will demonstrate an oval non-compressible hyperechoic mass, circumscribed with a hypoechoic rim, abutting the colon wall (22-24). The color Doppler will indicate no central blood flow (24,25). Although acute epiploic appendagitis can be distinguished on ultrasound, Danse et al. recommend that ultrasounds be used only in thin patients at experienced centers. MRI shows a focal lesion with fat attenuation (26).
Mimics of acute epiploic appendagitis include acute diverticulitis, acute omental infarction, mesenteric panniculitis, sclerosing mesenteritis, tumor or metastasis to the mesocolon, or other inflammatory changes affecting the colon (7). For females, the differential diagnosis may also include ovarian torsion, ovarian cyst rupture, and ectopic pregnancy (27). Acute epiploic appendagitis can be distinguished from acute diverticulitis with the recognition of diverticula, inflammation, and colonic wall thickening on CT imaging. Additionally, patients with acute diverticulitis are more likely to present with fever, nausea, vomiting, elevated white blood cell count, and rebound tenderness (20,28).
A non-enhancing mass with non-uniform attenuation and fat stranding is likely to indicate acute omental infarction. Typically, patients present with right sided abdominal pain lasting a few days, causing it to be mistaken for acute appendicitis, and the masses are located anterior to the ascending or transverse colon (7,29). Compared to acute epiploic appendagitis, acute omental infarctions have a higher incidence in pediatric patients and can lead to the development of acute appendicitis due to the anatomical location involved (7,30,31). Both acute omental infarction and acute diverticulitis are likely to affect areas larger than 5 cm (7). Sclerosing mesenteritis, a condition affecting persons in the 6th–7th decade of life, has a clinical presentation involving abdominal pain, weight loss, fever, nausea, vomiting, and diarrhea. Similar to acute epiploic appendagitis, it is a usually a benign and self-limited.
Conclusions
Acute epiploic appendagitis can be diagnosed more precisely with careful characterization on imaging studies. Although a rare occurrence, it is critical to add the recognition of acute epiploic appendagitis to the repertoire of abdominal pathologies that clinicians have grown accustomed to detecting. The combination of clinical judgment and supporting imaging study can help prevent unnecessary surgery or treatments.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: It was waived as it was not required in the writing of this article. Case data has been entirely deidentified from a person, location, and date.
References
- Sand M, Gelos M, Bechara FG, et al. Epiploic appendagitis–clinical characteristics of an uncommon surgical diagnosis. BMC Surg 2007;7:11. [Crossref] [PubMed]
- Ghahremani GG, White EM, Hoff FL, et al. Appendices epiploicae of the colon: radiologic and pathologic features. Radiographics 1992;12:59-77. [Crossref] [PubMed]
- van Breda Vriesman AC. The hyperattenuating ring sign. Radiology 2003;226:556-7. [Crossref] [PubMed]
- Linkenfeld F. Deutsche Ztschr f Chir. 1908;92:383. [Crossref]
- Marinis TP, Cheek JH. Primary inflammation of the appendices epiploicae: with review of the literature and report of six additional cases. Ann Surg 1949;129:533-7. [Crossref] [PubMed]
- Thomas JH. Epiploic appendagitis. Surg Gynecol Obstet 1974;138:23-5. [PubMed]
- Singh AK, Gervais DA, Hahn PF, et al. Acute epiploic appendagitis and its mimics. Radiographics 2005;25:1521-34. [Crossref] [PubMed]
- Chowbey PK, Singh G, Sharma A, et al. Torsion of appendices epiploicae presenting as acute abdomen: laparoscopic diagnosis and therapy. Indian J Gastroenterol 2003;22:68-9. [PubMed]
- Nugent JP, Ouellette HA, O'Leary DP, et al. Epiploic appendagitis: 7-year experience and relationship with visceral obesity. Abdom Radiol (NY) 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Akinosoglou K, Kraniotis P, Thomopoulos K, et al. Epiploic appendagitis: A non-surgical cause of acute abdomen. Ann Gastroenterol 2015;28:296-8. [PubMed]
- Macari M, Laks S, Hajdu C, et al. Caecal epiploic appendagitis: an unlikely occurrence. Clin Radiol 2008;63:895-900. [Crossref] [PubMed]
- Michael A, Zakry Y, Hanif H. Epiploic Appendagitis: An uncommon surgical diagnosis. Med J Malaysia 2017;72:128-9. [PubMed]
- Singh AK, Gervais DA, Hahn PF, et al. Acute epiploic appendagitis and its mimics. Radiographics 2005;25:1521-34. [Crossref] [PubMed]
- Baker ME. Imaging and interventional techniques in acute left-sided diverticulitis. J Gastrointest Surg 2008;12:1314-7. [Crossref] [PubMed]
- Schnedl WJ, Krause R, Tafeit E, et al. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol 2011;8:45-9. [Crossref] [PubMed]
- Legome EL, Belton AL, Murray RE, et al. Epiploic appendagitis: the emergency department presentation. J Emerg Med 2002;22:9-13. [Crossref] [PubMed]
- Ryen C. Epiploic appendagitis in a female patient with situs ambiguous abnormality. J Radiol Case Rep 2009;3:30-4. [Crossref] [PubMed]
- Carmichael DH, Organ CH. Epiploic disorders: conditions of the epiploic appendages. Arch Surg 1985;120:1167-72. [Crossref] [PubMed]
- Hwang JA, Kim SM, Song HJ, et al. Differential diagnosis of left-sided abdominal pain: primary epiploic appendagitis vs colonic diverticulitis. World J Gastroenterol 2013;19:6842-8. [Crossref] [PubMed]
- Singh AK, Gervais DA, Hahn PF, et al. CT appearance of acute appendagitis. AJR Am J Roentgenol 2004;183:1303-7. [Crossref] [PubMed]
- Rao PM, Wittenberg J, Lawrason JN. Primary epiploic appendagitis: evolutionary changes in CT appearance. Radiology 1997;204:713-7. [Crossref] [PubMed]
- Mollà E, Ripolles T, Martinez MJ, et al. Primary epiploic appendagitis: US and CT findings. Eur Radiol 1998;8:435-8. [Crossref] [PubMed]
- Rioux M, Langis P. Primary epiploic appendagitis: clinical, US, and CT findings in 14 cases. Radiology 1994;191:523-6. [Crossref] [PubMed]
- Danse EM, Van Beers BE, Baudrez V, et al. Epiploic appendagitis: color Doppler sonographic findings. Eur Radiol 2001;11:183-6. [Crossref] [PubMed]
- Hanson JM, Kam AW. Paracolic echogenic mass in a man with lower abdominal pain. Is epiploic appendagitis more common than previously thought? Emerg Med J 2006;23:e17. [Crossref] [PubMed]
- Şirvanci M, Balci NC, Karaman K, et al. Primary epiploic appendagitis: MRI findings. Magn Reson Imaging 2002;20:137-9. [Crossref] [PubMed]
- Sorser SA, Maas LC, Yousif E, et al. Epiploic appendagitis: the great mimicker. South Med J 2009;102:1214-7. [Crossref] [PubMed]
- Son HJ, Lee SJ, Lee JH, et al. Clinical diagnosis of primary epiploic appendagitis: differentiation from acute diverticulitis. J Clin Gastroenterol 2002;34:435-8. [Crossref] [PubMed]
- Grattan-Smith JD, Blews DE, Brand T. Omental infarction in pediatric patients: sonographic and CT findings. AJR Am J Roentgenol 2002;178:1537-9. [Crossref] [PubMed]
- Puylaert JB. Right-sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology 1992;185:169-72. [Crossref] [PubMed]
- Gupta N, Sapire JM, Marrinan G, et al. Some Stones Are Precious—Extraluminal Appendicoliths. Indian J Surg 2016;78:507-8. [Crossref] [PubMed]
Cite this article as: Patel H, Abdelbaki A, Steenbergen P, Chanana C, Li S. Know the name: acute epiploic appendagitis—CT findings and review of literature. AME Case Rep 2018;2:8.


