Concomitant a giant pulmonary bulla on the left lower lobe and hamartoma successfully treated by video-assisted thoracoscopic pulmonary wedge resection
Introduction
Giant bullous emphysema (GBE), referred to as vanishing lung syndrome (VLS) as a clinical syndrome, was first described by Burke in 1937 (1). Roberts et al. established the radiographic criteria for this syndrome as the presence of giant bullae in one or both upper lobes occupying at least one-third of the hemithorax and compressing the normal surrounding parenchyma (2). Here, we describe a woman with a GBE involves the dorsal segment of left lower lobe and associated with a pulmonary hamartoma arising from the bulla wall.
Clinical summary
A 48-year-old woman, never a smoker, was admitted with an 8-month history of left thoracic pain and a chronic low back pain. The pain slowly appeared without physical activity, cough or trauma. Physical examination showed left upper lung with diminished breath sounds specifically on the left apex and posterior over the left anterior chest,we could not find palpable subcutaneous emphysema in neck and chest and the patient has normal oxygen saturation. The patient with no significant medical history, and her family history was noncontributory.
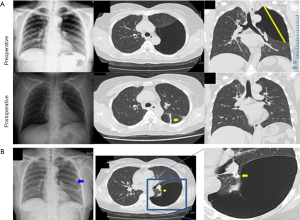
A chest X-ray showed large lucent area over the left thorax (Figure 1A), in the air space the lack of vessels coursing, the location of the upper lobes absence of visible other smaller bullae and concave surface of lung was not present on image findings were suggestive of a pneumothorax. And then, a venous catheter as left chest tube was inserted under the diagnosis of spontaneous pneumothorax but follow-up chest radiography showed no expansion of the left lung (Figure 1B). Computed tomography of chest subsequently demonstrated that a giant bulla occupying the left thorax with left upper and lower lobes compressive atelectasis and a nodular shadow was presented in the oblique fissure of left lung (Figure 1A). Laboratory studies were unremarkable.
Through the video-assisted thoracic surgery (VATS) with left-sided, two-port technique was used to gain to the thoracic cavity. The giant bulla was located at the dorsal segment of lower lobe presents as a about 16-cm-sized single giant emphysematous bulla, majority compression of the left upper lobe, the multiple pleural adhesions and a nodule was a base of 1.5 cm arose from the giant bulla wall showing grayish-white, protruding, rigid and clear boundary were identified (Figure 2A).
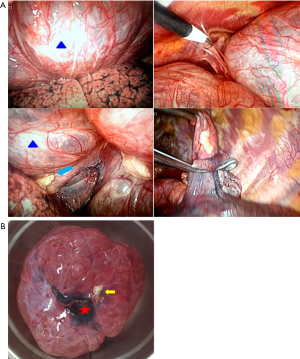
The bulla was not collapsed even by differential lung ventilation, so the walls of the bulla were punctured. The giant bulla and the nodule were successful thoracoscopic pulmonary wedge resected with two 45 mm Ethicon linear stapling devices (Johnson & Johnson, USA) the staple line was set in the normal lung tissue along the bases of the bulla (Figure 2A). After surgical removal of bulla and nodule (Figure 2B), the compressed left upper lobe was re-expanded by manual ventilation without difficulty and one chest-tube was inserted.
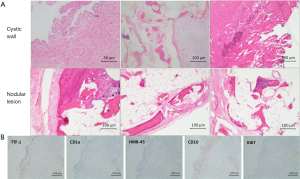
Microscopical examination of the giant bulla showed the bulla wall is fibrous connective tissue, coating layer of flat cells, accompanied by a small amount of inflammatory cell infiltration (Figure 3A) (hematoxylin and eosin, original magnification ×4). The epithelial lining of bulla wall was positive for thyroid transcription factor 1 (TTF-1) and negative for CD1a, human melanoma black-45 (HMB-45), CD-10 or Ki-67 (Figure 3B). In addition, trabecular bone, cartilage, adipose tissue and irregular glandular cavity like structure were found in the nodular lesion, and the cell atypia was not obvious (Figure 3A). In accordance with the above findings, the final diagnosis was consistent with concomitant GBE and a pulmonary hamartoma arose from the bulla wall. After surgical resection via VATS, the lung was re-expanded well and no air leak was noted (Figure 1A), chest tube was removed on second postoperative day. The patient was completely recovered without any event and was discharged. She is currently asymptomatic and doing well after 9 months of follow-up.
Discussion
In this report, we describe the case of a woman with co-existence of a giant bulla and pulmonary hamartoma which arising from the bulla wall. To the best of our knowledge, this disorder was also very rare reports in the literature.
GBE, also referred to as VLS, is a progressive bullous disease usually afflicts young male cigarette smokers and characterized by large bulla that involve at least one-third of one or both hemithorax. The bullae are mostly limited to the upper lobes of the lungs (2,3). In this case, the bulla is unusual for its lower lobe involvement of a nonsmoking female.
Both microscopic and histological features of present case showed the bulla is an airspace demarcated by a thin wall that is no greater than 1 mm in thickness, and accompanied by emphysematous, and measuring more than 16 cm in diameter that involve at least one-third of left hemithorax and was originated from the left lower lobe which were consistent with the previous description of giant pulmonary bulla (4). Pathological findings showed the bulla wall is fibrous connective tissue, coating layer of flat cells, accompanied by a small amount of inflammatory cell infiltration (Figure 3A). The epithelial lining of bulla wall showed positive for TTF-1, which suggested type 2 pneumocytes were scattered, but negative for CD1a or HMB-45, even the epithelium exhibited low expression of Ki-67, that was less than 1.0% (Figure 3B). Pulmonary lymphangioleiomyomatosis and Langerhans cell histiocytosis should be excluded, neither the endometriosis and metastatic endometrial stromal sarcoma lack of expression of CD10. Thus, the case could be classified as a pulmonary giant bulla and complicating pulmonary hamartoma which arising on the bulla wall. The case presented herein both in clinical roentgenology and pathological studies were different from a recent case report described a novel hamartomatous disorder in a woman of reproductive age with a giant bulla in the upper lobe of right lung. In their case report, Yorita et al. described the bullous lesion wall with ciliated, nonatypical epithelium and layers of nonatypical spindle cells which were positive for smooth muscle markers and sex steroid hormone receptors [e.g., estrogen receptor (ER) and progesterone receptor (PgR)] which may be a novel form of hamartoma and has not been reported in the literature (5). The present case is also different from another very rare disease, mesenchymal cystic hamartoma (MCH) of the lung was primarily described by Mark in 1986 (6). The disease is characterized by nodules of primitive mesenchymal cells that gradually increase in size and then become cystic.
The other notable fact was a giant bulla of the lung is suggested as a risk factor for lung cancer. Nakamura et al. reported that the frequency of lung cancer in subjects with bullous disease was approximately 32 times higher than in those without this abnormality (7). In the present case, the chest computed tomography scan showed a nodular shadow in the left lower lobe of the lung (Figure 1A). The nodular shadow with clear margin and high density, a pulmonary hamartoma was considered. However, the ground glass opacity (GGO) shadow with a coexistent giant bulla should keep in mind the lung cancer. The suspected case should be checked with frozen sections to increase the rate of cure. It is considered to be important to detect giant bulla prior to lung cancer, and periodical follow-up must be done to find early stage lung cancer (8,9).
As an old topic, the giant bullae of the lung and pneumothorax were usually mimicking each other (10-14), the diagnosis may sometimes pose a challenge. Since the differentiation between tension pneumothorax (TPX) and a giant bulla may be very difficult (10), in present case, chest radiography findings also easy to be misdiagnosed as TPX and a venous catheter as chest tube was inserted left thorax, fortunately without rupturing the bulla (Figure 1B). But in fact, the therapies of these two similar lesions are completely different. So that, we must be comprehensive analysis of medical history, sex, smoking and family history, physical examination and radiology for true diagnosis.
Successful treatments of giant bulla with VATS have been widely reported (15,16). Complete resection of the bulla was considered importance since the risk of development of lung cancer is much higher in patients with GBE. For this reason, it is worth noting that because the nonfunctioning bullae that compresses normal lung of patients will expand after a surgical procedure and the preoperative impairment of FEV1 could significant improve after operation, the low FEV1% (<35%) should not be considered a contraindication to bullectomy (15). Other treatments such as endobronchial valve (EBV) can be used to offer a treatment option for GBE in selected patients via placing EBV in the airways communicating with the bulla (17,18). But in the present case, EBV was not an appropriate therapy, since there was no supply airway of the giant bulla is found.
In conclusion, we described giant bulla complicating pulmonary hamartoma of the left lower lobe of the lung in a female nonsmoker. This is a rare case and previously unreported of a giant bulla complicating pulmonary hamartoma that originated in the bullous wall, the bulla with hamartoma successfully treated by pulmonary wedge resection using VATS and relief of the compressed the surrounding normal lung after operation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Burke RM. Vanishing lungs: a case report of bullous emphysema. Radiology 1937;28:367-71. [Crossref]
- Roberts L, Putman CE, Chen JT, et al. Vanishing lung syndrome: upper lobe bullous pneumopathy. Rev Interam Radiol 1987;12:249-55.
- Sharma N, Justaniah AM, Kanne JP, et al. Vanishing lung syndrome (giant bullous emphysema): CT findings in 7 patients and a literature review. J Thorac Imaging 2009;24:227-30. [Crossref] [PubMed]
- Hansell DM, Bankier AA, MacMahon H, et al. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008;246:697-722. [Crossref] [PubMed]
- Yorita K, Ayabe T, Chosa E, et al. Unusual cystic hamartomatous lung lesion with clinical manifestation of subpleural bullae in a woman of reproductive age: A case report. Pathol Int 2015;65:558-62. [Crossref] [PubMed]
- Mark EJ. Mesenchymal cystic hamartoma of the lung. N Engl J Med 1986;315:1255-9. [Crossref] [PubMed]
- Nakamura H, Takamori S, Miwa K, et al. Rapid-growth lung cancer associated with a pulmonary giant bulla: a case report. Kurume Med J 2003;50:147-50. [Crossref] [PubMed]
- Sato S, Asakura J, Suzuki H, et al. Study on surgical treatment for lung cancer associated with giant bullous disease. Jpn J Thorac Cardiovasc Surg 1998;46:260-6. [Crossref] [PubMed]
- Hirai S, Hamanaka Y, Mitsui N, et al. Primary lung cancer arising from the wall of a giant bulla. Ann Thorac Cardiovasc Surg 2005;11:109-13. [PubMed]
- Gökçe M, Saydam O, Altin R, et al. Giant bulla mimicking tension pneumothorax. Tuberk Toraks 2009;57:435-8. [PubMed]
- Chen CK, Cheng HK, Chang WH, et al. Giant emphysematous bulla mimicking tension pneumothorax. Am J Med Sci 2009;337:205. [Crossref] [PubMed]
- Waseem M, Jones J, Brutus S, et al. Giant bulla mimicking pneumothorax. J Emerg Med 2005;29:155-8. [Crossref] [PubMed]
- Chiappetta M, Nachira D, Porziella V, et al. Multiple giant bullae of the lung mimicking massive pneumothorax in a patient with osteogenesis imperfecta. Thorax 2016;71:577. [Crossref] [PubMed]
- Gonzalez M, Krueger T, Ris HB, et al. Images in thorax. Tension pneumothorax mimicking giant emphysematous bullae. Thorax 2010;65:1028. [Crossref] [PubMed]
- Huang W, Han R, Li L, et al. Surgery for giant emphysematous bullae: case report and a short literature review. J Thorac Dis 2014;6:E104-7. [PubMed]
- Van Bael K, La Meir M, Vanoverbeke H. Video-assisted Thoracoscopic Resection of a Giant Bulla in Vanishing Lung Syndrome: case report and a short literature review. J Cardiothorac Surg 2014;9:4. [Crossref] [PubMed]
- Tian Q, An Y, Xiao BB, et al. Endobronchial valve to treat large bulla at right middle lobe in chronic obstructive pulmonary disease patients. J Thorac Dis 2015;7:E374-7. [PubMed]
- Çetinkaya E, Özgül MA, Gül Ş, et al. Successful Treatment of Bulla with Endobronchial Valves. Case Rep Pulmonol 2015;2015:947403.
Cite this article as: An J, Long M, Jiang Y, Jin Y. Concomitant a giant pulmonary bulla on the left lower lobe and hamartoma successfully treated by video-assisted thoracoscopic pulmonary wedge resection. AME Case Rep 2017;1:2.


