Tracheopathia osteochondroplastica: a case report illustrating the importance of imaging in this rare disorder
Highlight box
Key findings
• Endoscopy imaging of the trachea is often required to diagnosis tracheopathia osteochondroplastica (TPO).
What is known and what is new?
• TPO is a disorder where cartilaginous nodules are found in the lumen of the trachea.
• Other forms of imaging are not effective at diagnosing TPO, which is often an incidental finding in endoscopy investigation of other concerns.
What is the implication, and what should change now?
• Bronchoscopy of the trachea should be more common in patients that report with atypical dyspnea, hemoptysis, or chronic cough.
• Patients with TPO should have longer follow-up times and consider bronchial lavage or biopsy for further understanding of the disease process and causes of recurrent infection.
Introduction
Tracheopathia osteochondroplastica (TPO) is a rare disorder that results in cartilaginous nodules in the lumen of the trachea. This is an idiopathic and benign condition that usually is asymptomatic (1). Common symptoms are dry cough, dyspnea, or hemoptysis, and there have been reports of difficult intubation associated with this disorder (2). TPO is associated with lower respiratory tract disease, asthma or asthma-like symptoms, and recurrent ear, nose, and throat (ENT) disease (3). Pulmonary function tests may show an obstructive defect in patients with TPO (4). As a result of poor diagnostic tools, TPO is commonly discovered as an incidental finding in fiberoptic bronchoscopy and/or chest computed tomography (CT), and the prevalence is believed to be underreported (3). The etiology of this disease is unknown and there are limit treatment options for patients. Biopsies demonstrating ossification of the tracheal nodules suggesting possible relationships to irritation (5). However, cases have been identified in both younger and older individuals with and without history of tobacco use (6). TPO has been reported in coexistence with thyroid pathologies and malignancies (7,8). The variation in disease presentation, severity, and course supports thorough investigation of clinical cases involving TPO. In this case, we present a patient with TPO that was identified during a bronchoscopy for an endobronchial lesion identified on a CT scan. This case goes through several clinical tests that were completed before the diagnosis and indicates the importance of including this disease as a possible differential when atypical dyspnea occurs. Lastly, it touches on the relationship between gastroesophageal reflux disease (GERD) and TPO, and the influence of treatment for these diseases that have not been investigated before. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-119/rc).
Case presentation
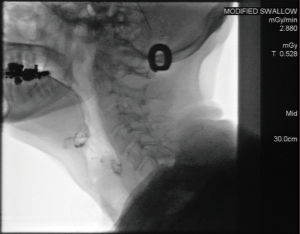
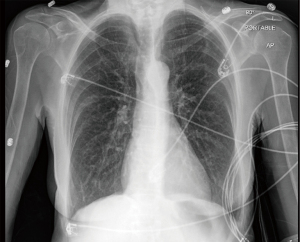
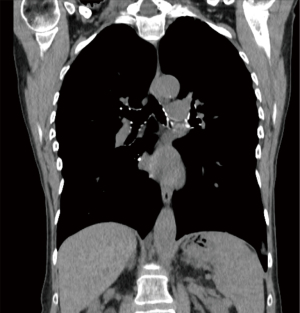
A 71-year-old female nonsmoker presented with a chief complaint of dyspnea on exertion and atypical chest pain. She has a past medical history of Takotsubo cardiomyopathy and GERD. There was no past medical history of asthma or respiratory infection. She reported several months of dyspnea on exertion and atypical chest pain. The patient denied unintentional weight changes, palpitations, or hemoptysis. Within the year prior to her diagnosis with TPO, she underwent pulmonary function testing (PFT), a barium swallow test, and multiple chest imaging scans. Results from the PFT demonstrated a normal forced expiratory flow maneuver, normal flow-volume loop shape, and no improvement with a bronchodilator. In addition, the use of an albuterol inhaler did not relieve her dyspnea. No abnormalities were noted when completing a barium swallow test (Figure 1). An magnetic resonance imaging (MRI) and X-ray of the chest had no major findings for the heart or lungs (Figures 2,3). A chest CT noted the presence of a 4 mm nodule in the upper left lobe (Figure 4). For further investigation of this nodule, a bronchoscopy was ordered. It showed prominent nodular lesions on the cartilaginous rings of the trachea with tortuous small subsegmental airways (Figure 5). From this observation, a diagnosis of TPO was made. All procedures in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent from the patient was obtained for publication of this case report and accompanying images. A copy of this consent if available for review by the editorial office of this journal.

After diagnosis, the patient was referred to a pulmonologist. She was informed that treatment for TPO is based on symptom management, and there are no major risks associated with having the diagnosis. Months after the initial diagnosis, the patient developed increasing GERD symptoms and underwent an esophageal dilation with improvement in her symptoms. From the patient’s perspective, she was relieved to learn that her shortness of breath was caused by a benign condition, but overall, it was frustrating for her to have gone through multiple invasive tests.
Discussion
TPO is a rare, benign condition that is assumed to be underdiagnosed due to the wide variation of nonspecific symptoms, and that it is usually diagnosed as an incidental finding of imaging (1). In the presented case, the patient reported atypical dyspnea on exertion but denied other symptoms or histories associated with TPO, such as hemoptysis or recurrent respiratory infection (8). She has a medical history of GERD, which has been reported in 14% of TPO cases, but PFTs were normal unlike a majority of cases (9). Further imaging and testing failed to reveal this disease. Like many other cases, the diagnosis arose from an incidental finding as a result of suspected bronchial lesion noted on a CT scan. Although abnormal CT scans have previously been reported in cases of TPO, imaging through bronchoscopy has been used more commonly for diagnosis (2,3). This patient underwent a number of different imaging techniques of the chest and throat, but TPO was not suspected until the diagnosis was made through bronchoscopy. This finding alludes to the importance of including TPO as a differential diagnosis in patients presenting with atypical dyspnea, and the need for bronchoscopy exploration for diagnosis. Being able to distinguish these patients from other respiratory diseases is important to determine the etiology, risks, and possible treatment for this disease. A previous study has shown recurrent respiratory infections as a risk and suggested that intubations may be more difficult on these patients (2). These patients may also benefit from bronchial lavage to studying the infections responsible for respiratory infection and bronchial biopsies to better understand disease etiology and risk for progression. Further analysis of tissue from these patients will help lead researcher in understanding the cause of future risk of TPO. In addition, increased follow-up and attention to these patients is necessary to reduce harm during future medical procedures and treatment for infections. A longer follow-up will also improve overall understanding of the disease process and possible need for more extreme treatments in the case of disease progression or in cases where malignancy may arise. In cases of large nodules and obstruction of the airway, laser therapy and mucosal resection have been considered as possible therapies (3,6). In this case, the patient reported improved symptoms from an atypical treatment related to another condition: esophageal dilation for GERD. Relief of TPO symptoms has not previously been attributed to this procedure, and this outcome suggest possible treatments for future cases. It also suggests that further investigation into the etiology, treatment, disease progression, and related diseases of TPO could be influential in relieving symptoms of dyspnea and recurrent infection.
Conclusions
The prevalence and etiology of TPO is unknown, and most diagnosis occurs as an incidental finding on bronchoscopy. This case demonstrates the variability of symptoms and poor sensitivity of current diagnostic tests to identify individuals with this disease. Due to the difficulty in diagnosis of this disease, there is a limitation on the treatment options for and possible risks of this disease. A greater focus on bronchial exploration in the setting of dyspnea is needed to understand the impacts of TPO. In severe cases, treatments, such as esophageal dilation may provide relief for patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-119/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-119/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-119/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent from the patient was obtained for publication of this case report and accompanying images. A copy of this consent if available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Garg R, Kushwaha RA, Goel MM, et al. An Unusual Cause of Respiratory Distress: Solitary Tracheopathia Osteochondoplastica-A Rare Entity. J Bronchology Interv Pulmonol 2015;22:274-7. [Crossref] [PubMed]
- Coëtmeur D, Bovyn G, Leroux P, et al. Tracheobronchopathia osteochondroplastica presenting at the time of a difficult intubation. Respir Med 1997;91:496-8. [Crossref] [PubMed]
- Leske V, Lazor R, Coetmeur D, et al. Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore) 2001;80:378-90. [Crossref] [PubMed]
- Cho HK, Jeong BH, Kim H. Clinical course of tracheobronchopathia osteochondroplastica. J Thorac Dis 2020;12:5571-9. [Crossref] [PubMed]
- Luo S, Wu L, Zhou J, et al. Tracheobronchopathia osteochondroplastica: two cases and a review of the literature. Int J Clin Exp Pathol 2015;8:9681-6. [PubMed]
- Uchimura K, Yamasaki K, Yatera K, et al. Multiple Tracheobronchial Polyposis Caused by Tracheobronchopathia Osteochondroplastica. Intern Med 2016;55:3165-7. [Crossref] [PubMed]
- Erelel M, Yakar F, Bingol ZK, et al. Tracheopathia osteochondroplastica: two unusual cases. J Bronchology Interv Pulmonol 2010;17:241-4. [Crossref] [PubMed]
- Nielsen SW, Stevens JR, Dion GR, et al. Dyspnea, Dysphonia, and Cough: Varied Presentations of Tracheobronchopathia Osteochondroplastica. Ann Otol Rhinol Laryngol 2015;124:829-33. [Crossref] [PubMed]
- Dumazet A, Launois C, Lebargy F, et al. Tracheobronchopathia osteochondroplastica: clinical, bronchoscopic, and comorbid features in a case series. BMC Pulm Med 2022;22:423. [Crossref] [PubMed]
Cite this article as: Lauinger AR, Yu-Ballard A. Tracheopathia osteochondroplastica: a case report illustrating the importance of imaging in this rare disorder. AME Case Rep 2024;8:32.