
Lobular capillary hemangioma post-chemotherapy for T-cell leukemia treated with an antibiotic: a case report
Highlight box
Key findings
• A 32-year-old male, known to have T-cell acute lymphoblastic leukemia treated with chemotherapy, currently on methotrexate and 6-mercaptopurine, presented with 1-month history of rapidly growing ulcerated nodules on his right hand. Skin biopsy revealed inflamed pyogenic granuloma (PG). Tissue cultures tested positive for Pseudomonas aeruginosa growth. Ciprofloxacin 500 mg twice daily, a 2-week course was started. Both lesions completely resolved at 10th-day of antibiotic course with no recurrence. This is a case of PG of the hand that was treated with no recurrence using an oral antibiotic.
What is known and what is new?
• PG is a benign vascular tumor of the skin and mucus membranes. Many theories discussed the potential of an angiogenic stimulus and an imbalance of inducers and inhibitors triggering the hyperplastic and neovascular response. The most frequently treatment for PG is surgical treatment, including shave and base electrocautery.
• This case represents an unexpected evolution to a possible therapeutic measure. Indeed, PG of the hand responds effectively to an oral antibiotic. In addition, the cosmetic outcome shown is superior to that of the conventional surgical one.
What is the implication, and what should change now?
• This case highlighted the unexpected role of a conservative measure rather than the conventional surgical method in treating vascular tumors. Moreover, its excellent cosmetic outcome has been demonstrated. We hypothesize that Gram negative infection may be a primary trigger inducing the angiomatous proliferation. We theorize that if such triggers were to be removed chances of curing PG can be achieved.
Introduction
Lobular capillary hemangioma, also known as pyogenic granuloma (PG), is a relatively common benign rapidly growing friable vascular tumor of the skin and mucus membranes (1). The angiomatous proliferation occurs in both genders of potentially any age with a predilection to affect individuals in their second and third decades of life (1,2). In adults, PG tends to occur on the trunk and upper extremities. In pediatric patients however the lesion is more frequently seen involving the head and neck (1). Although the exact pathogenesis of PG is unknown, many theories discussed the potential of an angiogenic stimulus and an imbalance of inducers and inhibitors triggering the hyperplastic and neovascular response (1,3). A previous study where 11 PGs have been analyzed, identified embryonic stem cells markers in the endothelial cells, while more differentiated forms were recognized in the interstitial cells suggesting de novo vasculogenesis originating from the primitive stem cells (4). Trauma has been described as a potential trigger, although history of trauma at the site of PG was reported in only 7% to 23% of patient (5). The most frequently used modality for treatment of PG is surgical treatment (6). It allows for histologic confirmation and carries the lowest rate of recurrence (7). Various surgical procedures are used including shave and base electrocautery (8,9). In this report, we present a case of two PGs that were completely resolved using antibiotics in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-159/rc).
Case presentation
A 32-year-old male, known to have T-cell acute lymphoblastic leukemia treated successfully with chemotherapy, currently maintained on methotrexate (MTX) 40 mg and 6-mercaptopurine, 100 mg, presented with 1-month history of painful rapidly growing ulcerated nodules on his right-hand palm and middle finger. The palmar skin lesion was noted first. A week later, a similar ulcerated nodule grew distally on the finger.
Both skin lesions developed approximately 3 months following patient initiation of maintenance treatment. Patient does not recall a history of trauma, burn or insects’ bites. Upon initial presentation to dermatology clinic the nodules have already attained the shape of fungating masses that bled easily on manipulation. Physical examination revealed two crusted nodules. A proximal lesion was observed over the palmar aspect between the second and third fingers, with the other one occurring alongside the distal phalanx of the third finger, measuring 2.5 cm × 1.5 cm, and 2.5 cm × 3.5 cm respectively (Figure 1).

In order to confirm the diagnosis as well as to provide therapeutic relief, a shave biopsy followed by cauterizing the floor were performed to the proximal PG. The specimen was sent for histologic examination, bacterial, mycobacterial and fungal cultures.
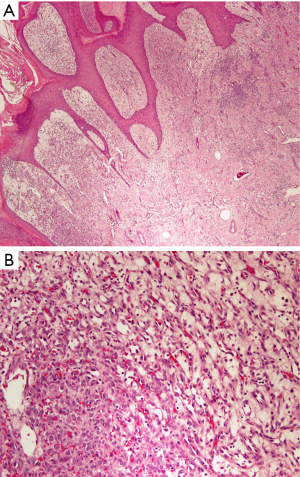
A week later following shave removal, the proximal nodule was noted to regrow and the distal one continued enlarging (Figure 2). A 2 mm punch biopsy was then obtained from the distal lesion and was sent to undergo similar sets of examinations. The result of the histologic examination was consistent with the finding in palmar lesion shave biopsy, and it revealed inflamed PG (Figure 3). Tissue cultures of both specimens tested positive for Pseudomonas aeruginosa growth while no fungal and tuberculosis were cultured. Based on positive Pseudomonas aeruginosa culture, ciprofloxacin 500 mg twice daily, a 2-week course was started. Both lesions completely resolved at 10th-day of antibiotic course with no recurrence (Figure 4). A timeline of events, highlighting patient’s key findings and interventions is illustrated (Figure 5).

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Surgical excision is the most frequently used treatment for PG. The aim of starting patient on antibiotic treatment was to manage any concurrent infection prior to treating the primary lesion using excisional techniques. Few published cases in the literature reported tumor regression following antibiotic treatment. Up to our knowledge, complete tumor resolution with no residual lesions has not been reported. The two cases previously reported in which conservative treatment has shown efficacy, shared similar presentation in regard to age of presentation and the potential trigger. Indeed, pediatric age group with a history of scalded burn were documented (10,11). Our case described an adult male with PG occurring spontaneously. Furthermore, the cosmetic outcome of our conservative treatment is superior to that of surgical management. Upon follow-up, the patient’s fingerprints were examined and noted to be intact. Besides its anti-microbial action, ciprofloxacin poses a well-known anti-inflammatory effect, which can potentially exert synergistic effect in treating PG, however treatment response cannot be explained solely by anti-inflammatory action since an organism has been isolated from PG lesion (12,13). Given the tissue culture results in our study and other formerly reported cases, we hypothesize that Gram negative infection may be a primary trigger inducing the angiomatous proliferation. We theorize that if such triggers were to be removed chances of curing PG can be achieved.
Conclusions
The proposed case represents an unexpected evolution to a possible therapeutic measure. This is a case of a patient with lobular capillary hemangioma of the hand treated successfully with an oral antibiotic. With the description of the above study, we believe that antibiotic treatment can potentially be promising in patients with PG. It is necessary to conduct further studies in order to comprehend the ethological hypothesis and clarify treatment options in PG.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-159/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-159/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-159/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Giblin AV, Clover AJ, Athanassopoulos A, et al. Pyogenic granuloma - the quest for optimum treatment: audit of treatment of 408 cases. J Plast Reconstr Aesthet Surg 2007;60:1030-5. [Crossref] [PubMed]
- Harris MN, Desai R, Chuang TY, et al. Lobular capillary hemangiomas: An epidemiologic report, with emphasis on cutaneous lesions. J Am Acad Dermatol 2000;42:1012-6. [Crossref] [PubMed]
- Kroumpouzos G, Cohen LM. Dermatoses of pregnancy. J Am Acad Dermatol 2001;45:1-19; quiz 19-22. [Crossref] [PubMed]
- Chen SY, Takeuchi S, Moroi Y, et al. Concordant overexpression of phosphorylated ATF2 and STAT3 in extramammary Paget's disease. J Cutan Pathol 2009;36:402-8. [Crossref] [PubMed]
- Pagliai KA, Cohen BA. Pyogenic granuloma in children. Pediatr Dermatol 2004;21:10-3. [Crossref] [PubMed]
- Schneider MH, Garcia CFV, Aleixo PB, et al. Congenital cutaneous pyogenic granuloma: Report of two cases and review of the literature. J Cutan Pathol 2019;46:691-7. [Crossref] [PubMed]
- Lee J, Sinno H, Tahiri Y, et al. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg 2011;64:1216-20. [Crossref] [PubMed]
- Mills SE, Cooper PH, Fechner RE. Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 1980;4:470-9. [Crossref] [PubMed]
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol 1991;8:267-76. [Crossref] [PubMed]
- Zhao H, Zhao H, Zhang C, et al. Multiple Pyogenic Granulomas After Burns: Response to Conservative Treatment in Five Children. Pediatr Dermatol 2015;32:e175-6. [Crossref] [PubMed]
- Ceyhan AM, Basak PY, Akkaya VB, et al. A case of multiple, eruptive pyogenic granuloma developed on a region of the burned skin: can erythromycin be a treatment option? J Burn Care Res 2007;28:754-7. [Crossref] [PubMed]
- Zusso M, Lunardi V, Franceschini D, et al. Ciprofloxacin and levofloxacin attenuate microglia inflammatory response via TLR4/NF-kB pathway. J Neuroinflammation 2019;16:148. [Crossref] [PubMed]
- Lahat G, Halperin D, Barazovsky E, et al. Immunomodulatory effects of ciprofloxacin in TNBS-induced colitis in mice. Inflamm Bowel Dis 2007;13:557-65. [Crossref] [PubMed]
Cite this article as: Al-Haddab M, Almughera TN, Alsalhi A, Alfurayh N. Lobular capillary hemangioma post-chemotherapy for T-cell leukemia treated with an antibiotic: a case report. AME Case Rep 2024;8:44.




