
Imaging diagnosis of rudimentary horn pregnancy: a case report
Highlight box
Key findings
• Only one cornual and with endometrium can be seen, furthermore, ultrasound diagnostic features of the rudimentary horn pregnancy (RHP) include visualization of uterus with an empty cavity along with a gestational sac (GS) containing a fetus. The presence of myometrial tissue surrounds the GS and connects to the displaced empty unicornuate uterus.
What is known and what is new?
• RHP is a rare form of gestation inside a rudimentary horn with endometrium and can be misdiagnosed as abdominal pregnancy, ruptured ectopic pregnancy, miscarriage and so on.
• Asking patients if there is a history of dysmenorrhea and be careful scanning, combined vaginal and abdominal methods to confirm the continuity of GS and cervix, and observing whether there has muscular structure around GS is of great significance for diagnosis. Sometimes blood flow can be helpful.
What is the implication, and what should change now?
• Differential diagnosis should be fully considered and excluded. If necessary, other imaging such as magnetic resonance imaging can be combined to make a clear diagnosis and treatment as soon as possible.
Introduction
Rudimentary horn is often accompanied by unicornuate uterus, a muscular structure with or without endometrium, which is adjacent to the unicornuate. The anatomic basis of this disease is an abnormal fusion of the bilateral accessory mesonephric duct during the embryonic period. A rare form of gestation inside a rudimentary horn with endometrium is called rudimentary horn pregnancy (RHP) and its incidence is difficult to evaluate, frequently reported incidence ranging from 1 per 76,000 to 1 per 140,000 pregnancies (1,2). The nonspecific of symptoms and variability in presentation depend on the classification, most commonly seen in a noncommunicating cavitary horn. Transperitoneal migration of sperm through the contralateral fallopian tube might be the explanation for the occurrence of pregnancy (3). Around 40% of women with RHP are asymptomatic especially in their first trimester, and many women often have a history of normal pregnancy and vaginal delivery which results in late or missed clinical diagnosis (3-5). RHP is reported to be misdiagnosed as abdominal pregnancy, ruptured ectopic pregnancy, miscarriage and so on (6,7). In magnetic resonance imaging (MRI), RHP always shows that gestational sac (GS) is surrounded by myometrium in contact with the round ligament, noncommunication with the cervix (8). We reported a case of RHP, which was initially suspected by ultrasound and MRI and further confirmed by subsequent surgery pathology. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-164/rc).
Case presentation
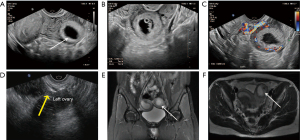
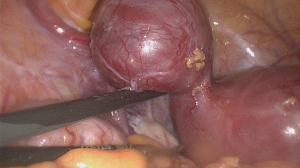
A 27-year-old woman came to Peking Union Medical College Hospital with a suspected ectopic pregnancy. She had a seven-week history of amenorrhea and a significant increase of blood human chorionic gonadotropin (hCG) (>200,000 IU/L). Her medical and gynecologic histories were normal, without irregular menstruation and significant dysmenorrhea. Sonographic examination showed uterus only had the right horn and endometrium was thickened about 1.7 cm. There was no GS in the uterine cavity. However, a 3.5×3.0 cm GS was found between the left ovary and corpus uteri, in which a 1 cm fetal bud can be seen with fetal heart. Abundant circumferential blood flow was observed around the GS. Furthermore, a thick-walled muscular structure about 0.5 cm surrounded the GS, which connected to the right myometrium (Figure 1). A right unicornuate uterus with left RHP was highly suspected. MRI showed a right unicornuate and a GS surrounded by myometrium in the left horn. In addition, her renal anomalies were excluded. The patient underwent laparoscopy which showed the small unicornuate skewed to the right. The rudimentary horn was enlarged with superficial hyperemia, and the junction was narrow (Figure 2). Gynecologists removed the rudimentary horn and the left fallopian tube. The patient made a good recovery and was soon discharged home after surgery. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Normal uterus is formed by complete development and fusion of bilateral accessory mesonephric ducts. If only one accessory mesonephric tube developed and the other underdeveloped, a unicornuate uterus with rudimentary horn generated. Rudimentary horn has only corpus uteri and fallopian tube, but no cervix and vagina, and the end of corpus uteri is blind. It is generally divided into three types in clinical. Type I: rudimentary horn has endometrium and communicates to unicornuate cavity with fistula. Type II: rudimentary horn has endometrium and do not connect to unicornuate cavity, which often accounts for about 90%. Type III: rudimentary horn has no endometrium and cavity. Type II often leads to periodic abdominal pain or progressive dysmenorrhea due to hematocele in the rudimentary horn after menarche, and even develops into endometriosis. Ultrasound shows a hypoechoic muscular tissue structure, next to the unicornuate which contains with echoless hematocele. Type I and III are often ignored because of no symptom. Ultrasound can only detect a hypoechoic solid mass beside the uterus, with or without endometrial echo. If sonographer lacks experience to this disease, it is easily to be missed. Just as the patient in this case has undergone gynecological ultrasound examination many times before, but showed no abnormality. When rudimentary horn is pregnant, 80–90% of cases may rupture during the second or third trimester due to hypoplasia of musculature, and increasingly reported the presence of placenta percreta resulting in life-threatening hemorrhage (9,10). Therefore, early diagnosis is necessary. Ultrasound is the preferred imaging method because of its convenience. However, due to the great dependence of the operator’s technology, it is necessary to clarify the ultrasonic characteristics of RHP. Based on the analysis of this case and previous literature (3), we suggest the following points for early sonographic diagnosis of RHP: (I) only one cornual with endometrium, (II) visualization of uterus with an empty cavity along with a GS containing a fetus. (III) The presence of myometrial tissue which surrounding the GS and connecting to the displaced empty unicornuate uterus, (IV) absent continuity between cervical and pregnant horn, (V) abundant blood flow around the GS. In this case, a GS surrounded by a myometrial wall and lack of continuity with the cervix in ultrasound findings strongly suggests RHP. In addition, it is always need to differentiate RHP from the following diseases: (I) tubal pregnancy, the shape of uterine cavity is normal, the GS is not communicated with the uterine cavity, and the myometrial tissue beside the GS is thin and incomplete. (II) Cornual pregnancy, the shape of uterine cavity is normal, the GS is located at one side of cornua uteri and expanded outside of the uterus, while the GS is partially communicated with uterine cavity. (III) An intrauterine pregnancy in a bicornuate uterus, uterine cavity where the GS is located communicates with the cervical canal. If two-dimensional ultrasonography is not clear due to artifact or poor patient condition, three-dimensional ultrasonography is helpful (11). MRI could be performed to improve the accuracy of diagnosis of RHP (6,8). We suggest combination ultrasound and MRI when facing patients suspected RHP, so as to formulate appropriate individualized treatment plans as soon as possible.
Conclusions
Although RHP is a rare disease, its danger is self-evident, thus early diagnosis and surgical resection are needed. By mastering the ultrasonic characteristics, we can make a definite diagnosis in the early pregnancy. We suggest that we should pay attention to the morphological characteristics of uterus when ultrasound is carried out in patients with suspected ectopic pregnancy in the first trimester, so as to find uterine malformation with ectopic pregnancy as soon as possible. In this case, we put forward the main points of ultrasonic diagnosis of RHP in order to improve the sensitivity and provide more information for clinicians to further diagnose and treat it.
Acknowledgments
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-164/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-164/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-164/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johansen K. Pregnancy in a rudimentary horn. Two case reports. Obstet Gynecol 1969;34:805-8. [PubMed]
- Nahum GG. Rudimentary uterine horn pregnancy. A case report on surviving twins delivered eight days apart. J Reprod Med 1997;42:525-32. [PubMed]
- Tsafrir A, Rojansky N, Sela HY, et al. Rudimentary horn pregnancy: first-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med 2005;24:219-23. [Crossref] [PubMed]
- Jayasinghe Y, Rane A, Stalewski H, et al. The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 2005;105:1456-67. [Crossref] [PubMed]
- Chopra S, Keepanasseril A, Rohilla M, et al. Obstetric morbidity and the diagnostic dilemma in pregnancy in rudimentary horn: retrospective analysis. Arch Gynecol Obstet 2009;280:907-10. [Crossref] [PubMed]
- Bidiga S, Henry K, Augustino O, et al. Rudimentary horn pregnancy, a differential diagnosis of an intraabdominal pregnancy: a case report. J Med Case Rep 2023;17:210. [Crossref] [PubMed]
- Nathan H, Sornum A. Diagnosis and management of a ruptured rudimentary horn pregnancy in a low-resource setting. BMJ Case Rep 2013;2013:bcr2013009957. [Crossref] [PubMed]
- Hamet B, Hoeffel C, Fague V, et al. Pregnancy in a rudimentary horn: multicenter’s MRI features of a rare condition. Abdom Radiol (NY) 2022;47:4195-204. [Crossref] [PubMed]
- Nahum GG. Rudimentary uterine horn pregnancy. The 20th-century worldwide experience of 588 cases. J Reprod Med 2002;47:151-63. [PubMed]
- Siwatch S, Mehra R, Pandher DK, et al. Rudimentary horn pregnancy: a 10-year experience and review of literature. Arch Gynecol Obstet 2013;287:687-95. [Crossref] [PubMed]
- Walker C, Collins L, Pham A, et al. Avoiding the fatal misdiagnosis of pregnancy in a noncommunicating rudimentary horn using 3D transvaginal ultrasound. J Clin Ultrasound 2020;48:553-6. [Crossref] [PubMed]
Cite this article as: Ji J, Tan L, Lv K. Imaging diagnosis of rudimentary horn pregnancy: a case report. AME Case Rep 2024;8:34.


