
Syphilitic aortitis and ostial coronary stenosis treated by endarterectomy, bypass grafting and aortic valve replacement: a case report
Highlight box
Key findings
• A 47-year-old woman presented with acute decompensated heart failure due to bilateral ostial coronary stenosis and severe aortic insufficiency. She underwent successful aortic valve replacement, right coronary ostioplasty and bypass grafting of the left coronary system, with uneventful recovery. Serology and tissue histopathology confirmed presence of syphilitic aortitis.
What is known and what is new?
• The syphilitic aortic root is characterized by concomitant aortic regurgitation and coronary ostial stenosis. In the modern antibiotic era, its multimodality imaging and operative findings were rarely reported in the literature. In this case report, its unique diagnostic and therapeutic hurdles, including the nuances of surgical techniques addressing ostial coronary stenosis, were demonstrated.
What is the implication, and what should change now?
• The manifestations of cardiovascular syphilis are protean and can pose significant diagnostic challenges. Surgical strategy should be individualized. Preoperative multimodality imaging can assist operative planning.
Introduction
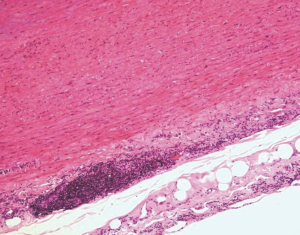
Syphilis is a systemic disease caused by the spirochete Treponema pallidum. The spirochetes localize to aortic adventitia early after primary infection, and eventually enter the media layer via lymphatics surrounding the vasa vasorum. This induces perivascular lymphoplasmacytic inflammation, leading to obliterative endarteritis, medial necrosis with intervening segments of wrinkling, classically known as tree-barking (1).
Dr. Denton Cooley divided the manifestations of cardiovascular syphilis into five categories: uncomplicated syphilitic aortitis, syphilitic aortic aneurysm, syphilitic aortic valvulitis with aortic regurgitation, syphilitic ostial coronary stenosis, and syphilitic myocarditis (1).
After primary infection, uncomplicated syphilitic aortitis occurs in 70–80% of untreated cases. The late complications of aortic aneurysm, aortic regurgitation, and ostial coronary stenosis typically manifest ten to twenty years after initial infection, usually during the forth to fifth decades of life.
Syphilitic ostial coronary stenosis as a disease entity was reported in the literature as early as 1929 (2). It was the third most common presentation of cardiovascular syphilis, accounting for 26% of cases in Heggveit’s historical autopsy series in 1964 (3). In Bruenn’s classic treatise on syphilitic coronary lesions, ostial coronary stenosis commonly involved both orifices. Furthermore, it was strongly associated with aortic regurgitation and likely reflected the severity of the contiguous inflammatory process (4).
Compared with traditional atherosclerotic multivessel coronary artery disease, patients with syphilitic ostial stenosis were younger, more often female, and typically reported a shorter duration of chest pain before presentation (5). Important differential diagnosis of isolated ostial coronary stenosis included prior chest irradiation, giant cell arteritis, Takayasu’s arteritis, fibromuscular dysplasia, Behçet disease, and trauma from percutaneous coronary angiography or intervention (6).
A 47-year-old woman presented in acute decompensated heart failure due to syphilitic ostial coronary stenosis and aortic insufficiency, eventually requiring urgent inpatient surgery. Diagnostic and therapeutic challenges were highlighted. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-32/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying multimedia content which were anonymized. A copy of the written consent is available for review by the editorial office of this journal.
A 47-year-old woman presented with crescendo chest pain, palpitations, and shortness of breath on exertion for two days. She was hypotensive, tachycardic and tachypneic at the emergency department. Physical examination showed bilateral fine basal crepitation, a grade 2 decrescendo diastolic murmur, and bilateral pitting lower limb edema.
She was an active smoker and worked as warehouse logistic worker. She had no history of substance or alcohol misuse. There was no family history of cardiovascular disease or sudden death.
Chest X-ray showed congested basal lung fields with mild bilateral pleural effusion. Electrocardiography showed ST-segment depression in inferior leads. The clinical findings were suggestive of acute pulmonary oedema.
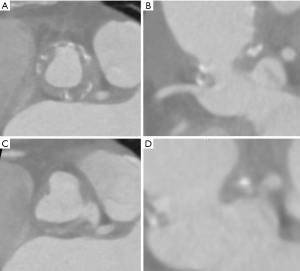
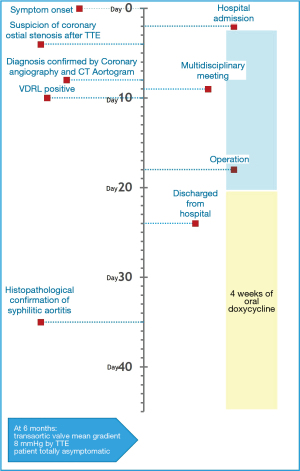
Transthoracic echocardiography (TTE) showed hypokinesia in the anterior wall as well as moderate-to-severe aortic insufficiency. An astute attending cardiologist noted immobile echogenic shadows in the ascending aorta on echocardiography obscuring the aortic valve, and thus arranged a computed tomography aortogram which excluded aortic dissection. Urgent cardiac catheterization showed an unusual picture of a slit-like left main coronary artery ostium, with the rest of the coronaries free from atherosclerotic plaque (Figure 1).

The atypical imaging findings prompted investigations for etiologies of infectious and inflammatory aortitis. Potential causative organisms of infectious aortitis included Treponema pallidum, Mycobacterium tuberculosis, Salmonella sp., Staphylococcus sp. and Campylobacter jejuni. Musculoskeletal examination and immunological assays were not suggestive of rheumatoid arthritis, systemic lupus erythematous, and Behçet disease. Ten days after hospitalization, the results of the Venereal Disease Research Laboratory (VDRL) test came back to be positive, which was further confirmed by a positive enzyme immunoassay for Treponema pallidum antibodies. Screening for co-infection of other sexually transmitted diseases including human immunodeficiency virus was negative.
While investigations for aortitis were ongoing, the case was discussed in a multidisciplinary team meeting. The decision was made to proceed with inpatient surgery for the critical left main stenosis and severe aortic regurgitation, after a brief period of medical optimization.
To facilitate operative planning, an electrocardiogram (ECG)-gated CT of the aortic root was performed, which demonstrated thickened and calcified circumferential plaque at the level of the sinotubular junction, causing subtotal obstruction of the left coronary ostium and partial obstruction of the right (Figure 2). Trans-esophageal echocardiography showed that the aortic valve was trileaflet. The leaflets were mildly calcified and thickened but free from vegetations. However, closure of the left coronary cusp was delayed, causing severe aortic insufficiency (Video 1).
The operation was performed two weeks after admission and commencement of guideline-directed heart failure and antimicrobial pharmacotherapy. Through a median sternotomy, aortic valve replacement, coronary ostioplasty and bypass grafting of the left anterior descending and obtuse marginal arteries was performed.
After institution of cardiopulmonary bypass and aortic cross-clamping, cold blood cardioplegia at 4 ℃ was administered via an aortic root cannula. Although the heart initially achieved electrical quiescence, it recovered a slow junctional rhythm shortly after aortotomy. Ice slush was applied and cold fibrillatory arrest was achieved. After excision of valve leaflets and brief period of debridement lasting a few minutes, antegrade cardioplegia can be delivered smoothly to both coronary ostia (Video 2).
Coronary ostioplasty was then attempted. The right coronary ostium was exposed, revealing a normal calibre orifice surrounded by healthy intima. Although cardioplegia can be given via the left coronary ostium, the ostium appeared atretic and the surrounding intima was thickened and fibrotic. This necessitated bypass grafting to the left coronary circulation, sparing the right. The left internal mammary artery was anastomosed to the anterior descending; a great saphenous vein graft, harvested endoscopically, was anastomosed to an obtuse marginal branch.
A size 19 On-X mechanical aortic valve was used (CryoLife, Kennesaw, GA, USA). We elected not to perform a root enlargement or replacement because her body surface area was only 1.44 m2. Given the presence of aortitis and the poor tissue quality, a more aggressive operation may be hazardous.
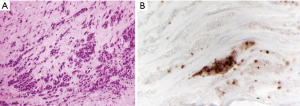
The crossclamp time was 97 min and she came off bypass without inotropes. Her postoperative course was unremarkable. She completed an additional four-week course of oral doxycycline at a dose of 100 mg twice daily. Histopathological examination confirmed the diagnosis of syphilitic aortitis (Figures 3,4). Seroreversion was confirmed at 6 months.
TTE 6 months postoperatively showed a mean gradient of 8 mmHg. She expressed satisfaction with her treatment as her recovery was swift and she is now asymptomatic. An overview of the patient’s course was presented in a timeline in Figure 5.
Discussion
Unlike atherosclerotic coronary artery disease, there is no consensus for the treatment of syphilitic ostial stenosis due to limited number of cases reported in the literature. A myriad of surgical techniques has been reported, including bypass grafting, percutaneous coronary intervention, endarterectomy or ostioplasty, and patch augmentation.
The first attempt at endarterectomy was reported in 1959 by Dubost and colleagues (6). Beck et al. also reported success with endarterectomy for two patients with the technique in 1965 (7). In 1983, Hitchcock et al. reported a small series of patients who underwent patch enlargement of left main coronary ostium with autogenous saphenous vein, with surgical exposure obtained by directly incising into the left sinus of Valsalva (8). Sullivan et al. subsequently reported a modification of the technique in 1989, by transecting the pulmonary trunk to approach the left main coronary artery, thus reducing bleeding and permitting exposure to a longer segment of coronary artery (5).
It is unclear whether ostioplasty or bypass grafting is the more durable option, given the young age at which these patients typically present. The decision to bypass the left coronary system in this patient was predicated on the fact that the left neo-ostium remained small and surrounded by unhealthy fibrotic tissue after debridement.
Intramuscular penicillin G benzathine once per week for 3 weeks is the standard regime for cardiovascular syphilis. Oral doxycycline or intravenous ceftriaxone are viable alternatives for those with penicillin allergy or those contraindicated for intramuscular injection such as warfarin therapy (9).
Conclusions
In conclusion, the manifestations of cardiovascular syphilis are protean. Isolated ostial coronary stenosis should alert the clinician to the possibility of cardiovascular syphilis. Our case highlights the unique diagnostic and therapeutic hurdles associated with the condition. The evolution and nuances of surgical techniques addressing ostial coronary stenosis was reviewed. Future endeavors to renew management of syphilitic aortitis should be pursued.
Acknowledgments
Prof. Fernand Lai prepared the histophotomicrographs of the aortic wall and aortic valve specimens.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-32/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-32/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-32/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and multimedia content which were anonymized. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Duncan JM, Cooley DA. Surgical considerations in aortitis. Part III: Syphilitic and other forms of aortitis. Tex Heart Inst J 1983;10:337-41. [PubMed]
- Pincoffs MC, Love WS. Observations upon syphilis of the heart, coronary ostia and coronary arteries with special reference to the clinical picture presented by syphilitic stenosis of the coronary ostia. Am J Syph Neurol 1934;XVIII:145.
- Heggtveit HA. Syphilitic aortitis. A clinicopathologic autopsy study of 100 cases, 1950 to 1960. Circulation 1964;29:346-55. [Crossref] [PubMed]
- Bruenn HG. Syphilitic disease of the coronary arteries. Am Heart J 1934;9:421-36. [Crossref]
- Sullivan JA, Murphy DA. Surgical repair of stenotic ostial lesions of the left main coronary artery. J Thorac Cardiovasc Surg 1989;98:33-6. [Crossref] [PubMed]
- Dubost C, Blondeau P, Piwnica A, et al. Syphilitic coronary obstruction: correction under artificial heart-lung and profound hypothermia. Surgery 1960;48:540-7. [PubMed]
- Beck W, Barnard CN, Schrire V. Syphilitic obstruction of coronary ostia successfully treated by endarterectomy. Br Heart J 1965;27:911-5. [Crossref] [PubMed]
- Hitchcock JF, Robles de Medina EO, Jambroes G. Angioplasty of the left main coronary artery for isolated left main coronary artery disease. J Thorac Cardiovasc Surg 1983;85:880-4. [Crossref] [PubMed]
- Workowski KA, Bolan GACenters for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1-137. Erratum in: MMWR Recomm Rep 2015;64:924. [PubMed]
Cite this article as: Ip SKF, Lim K, Wong RHL. Syphilitic aortitis and ostial coronary stenosis treated by endarterectomy, bypass grafting and aortic valve replacement: a case report. AME Case Rep 2023;7:15.


