
Pneumonectomy in an elderly patient with congenital unilateral lung hypoplasia and recurrent Aspergillus: a case report
Introduction
Lung hypoplasia is a congenital disorder that is usually detected in childhood. Although the true incidence is not known, it is estimated to have a prevalence of 9% to 28% in cases of premature rupture of membranes at 15–18 weeks gestation (1). The majority of patients with lung hypoplasia have congenital abnormalities of other organs, which often leads to further complications. However, patients with various degrees of pulmonary underdevelopment occasionally remain asymptomatic and can be followed closely for symptom progression over time (2-5).
The development of diffuse cystic disease in the hypoplastic lung has not been previously described. In this report, we present an elderly patient with unilateral right lung hypoplasia which was complicated by recurrent Aspergillus infections. Given gradual progression of symptoms later in adulthood, he underwent pneumonectomy, which yielded significant improvement in his respiratory difficulties. This case serves to emphasize that age and other comorbidities should not be absolute contraindications for surgical intervention in these patients, particularly when optimal medication therapy is not sufficient for symptom control. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-38/rc).
Case presentation
A 72-year-old man with a history of type 2 diabetes mellitus and chronic immune thrombocytopenic purpura presented with acute on chronic cough. He reported first receiving a diagnosis of right lung underdevelopment at the age of 6. Recent computed tomography (CT) scans confirmed congenital hypoplasia of his right lung, absence of his pulmonary artery with numerous bronchial artery collaterals, diffuse bronchial atresia, and peripherally distributed cystic disease. In addition to his diabetes medications, his current medication regimen consisted of tiotropium/olodaterol (Stiolto Respimat) 2.5-2.5 µg/actuation 2 inhalations per day, theophylline 200 mg daily, and as needed ipratropium/albuterol (Combivent). Several sputum cultures, the first of which was over 10 years from the current presentation, showed Aspergillus fumigatas, for which he was treated with extended courses of voriconazole, ranging from weeks to months. He experienced mild hemoptysis prior to starting his first course of voriconazole, though did not have any recurrence of this symptom later in life. However, voriconazole was often restarted when he experienced worsening cough or dyspnea and sputum cultures showed Aspergillus. In total, he received voriconazole for 46 months over this 10-year period. Recent serological studies for Aspergillus antibodies were negative. Radiographically, his repeat fungal infections correlated with multiple scattered mycetomas on serial CT scans (Figure 1A,1B). Additionally, he was empirically treated for bacterial pneumonia or acute bronchitis at least 16 times over a 15-year period in the setting of worsening cough and intermittent pleurisy.
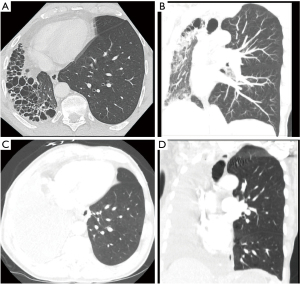
Due to his favorable functional status and frequency of Aspergillus infections, along with inadequate symptom control with his inhaler regimen to date, he was felt to be a suitable candidate for right-sided pneumonectomy. His pre-operative pulmonary function tests (PFTs) were compatible with long standing obstructive lung disease, with predicted forced expiratory volume in one second (FEV1) and diffusing lung capacity for carbon monoxide (DLCO) of 61% and 98% respectively, and preserved bronchodilator response. He underwent successful right pneumonectomy (Figure 1C,1D), with intraoperative findings revealing large cystic disease with purulence (Figure 2). Final pathology revealed prominent bronchiectasis with associated lymphocytic infiltrates and clusters of fungal microorganisms with hyphae-forms in the dilated airways of all three lobes, especially in the lower lobe. He had an uneventful postoperative course and is currently doing well, approaching 1 year from his surgery. He is using albuterol as needed for symptom control and is gradually increasing his exercise tolerance. Serial follow-up imaging has shown a well aerated left lung.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Unilateral pulmonary hypoplasia has been reported to have a mortality rate of up to 50% in the neonatal period (6). Most often, the underdevelopment of the lung is secondary to other congenital abnormalities, including but not limited to congenital diaphragmatic hernia, congenital heart diseases, and genitourinary malformations (7). The primary form of hypoplasia is rarer and thought to be idiopathic; as in this patient, it is not associated with other congenital disorders. While the majority of individuals with unilateral hypoplasia are diagnosed at a young age, a minority have none to minimal symptoms and are diagnosed in adulthood, often incidentally on chest imaging. In patients with agenesis, which refers to complete absence of pulmonary parenchyma, bronchi, and vessels, there is some evidence that right-sided agenesis is associated with decreased survival than left-sided agenesis possibly due to higher incidence of heart failure in the neonatal period, as well as increased incidence of multiorgan congenital underdevelopment (8). However, this mortality difference has not been reported in those with unilateral hypoplasia.
This patient’s obstructive pattern on PFTs with a response to bronchodilators was suggestive of an asthma physiology, for which he was trialed on several inhalers and oral medications with moderate benefit. However, the gradual worsening of his respiratory status over a long period of time may have been due to his recurrent pulmonary infections. Specifically, the diffuse cystic disease in his hypoplastic lung likely served as a nidus for Aspergillus infections. An aspergilloma has been previously reported in a patient with congenital cystic adenomatoid malformation (CCAM), a rare congenital cystic lung disease (9). However, cystic disease in CCAM is often localized to one lobe and is not associated with pulmonary artery agenesis and bronchial atresia, suggesting that this was not the underlying etiology for this patient.
The role of pneumonectomy in this patient population is unclear. One retrospective study of various surgical interventions in adult patients with congenital lung diseases showed similar rates of complications and length of hospitalization with video-assisted thoracoscopic surgery (VATS) interventions versus thoracotomy approaches (10). The extensive adhesions in this patient would have made VATS challenging in this case, however the aforementioned study indicates that there may be a role for minimally invasive interventions in this population. Moreover, the patient in this case is one of the oldest reported to have undergone definitive surgical intervention for his hypoplastic lung. We anticipate that evaluation for surgical intervention may have been delayed initially due to this patient’s age. While older age is generally thought to be a risk factor for post-operative morbidity and mortality, studies have suggested that age itself should not be a contraindication for pneumonectomy and instead should be one component of a comprehensive risk-assessment approach (11,12). Additionally, there may be higher rates of perioperative complications for right-sided versus left-sided pneumonectomies, including but not limited to bronchopleural fistulas and pulmonary edema, though further investigation is needed to clarify true differences in outcomes between the two procedures (13).
Conclusions
This case report serves to highlight the potential beneficial role of pneumonectomy for progressive obstructive lung physiology in a rare patient presentation. Regular evaluation of this patient’s dyspnea and other respiratory symptoms was key to his eventual successful outcome. Ultimately, the role of surgical interventions remains to be further defined for this patient population, and reports such as this will add to existing, limited data on adults with congenital lung conditions. It is crucial to determine both optimal medical management as well as timing for surgical intervention in adult patients with congenital lung disease.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-38/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-38/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-38/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Katsenos S, Antonogiannaki EM, Tsintiris K. Unilateral primary lung hypoplasia diagnosed in adulthood. Respir Care 2014;59:e47-50. [Crossref] [PubMed]
- El-Badrawy A, El-Badrawy MK. Adult presentation of asymptomatic right lung agenesis: a rare anatomical variation. Surg Radiol Anat 2019;41:247-9. [Crossref] [PubMed]
- Kaya O, Gulek B, Yilmaz C, et al. Adult presentation of symptomatic left lung agenesis. Radiol Case Rep 2017;12:25-8. [Crossref] [PubMed]
- Kumar P, Tansir G, Sasmal G, et al. Left Pulmonary Agenesis with Right Lung Bronchiectasis in an Adult. J Clin Diagn Res 2016;10:OD15-7. [Crossref] [PubMed]
- Papadopoulos D, Misthos P, Chorti M, et al. Unilateral pulmonary hypoplasia in an adult patient. Monaldi Arch Chest Dis 2018;88:829. [Crossref] [PubMed]
- Delgado-Peña YP, Torrent-Vernetta A, Sacoto G, et al. Pulmonary hypoplasia: An analysis of cases over a 20-year period. An Pediatr (Barc) 2016;85:70-6. [Crossref] [PubMed]
- Currarino G, Williams B. Causes of congenital unilateral pulmonary hypoplasia: a study of 33 cases. Pediatr Radiol 1985;15:15-24. [Crossref] [PubMed]
- Gilbert EF, Opitz JM. The pathology of some malformations and hereditary diseases of the respiratory tract. Birth Defects Orig Artic Ser 1976;12:239-70.
- Feng A, Cai H, Sun Q, et al. Congenital cystic adenomatoid malformation of lung in adults: 2 rare cases report and review of the literature. Diagn Pathol 2012;7:37. [Crossref] [PubMed]
- Ceylan KC, Batihan G, Üçvet A, et al. Surgery in congenital lung malformations: the evolution from thoracotomy to VATS, 10-year experience in a single center. J Cardiothorac Surg 2021;16:131. [Crossref] [PubMed]
- Annessi V, Paci M, Ricchetti T, et al. Is age over 70 years a risk factor for pneumonectomy? Asian Cardiovasc Thorac Ann 2009;17:272-7. [Crossref] [PubMed]
- Minervini F, Kocher GJ, Bertoglio P, et al. Pneumonectomy for lung cancer in the elderly: lessons learned from a multicenter study. J Thorac Dis 2021;13:5835-42. [Crossref] [PubMed]
- Fuentes PA. Pneumonectomy: historical perspective and prospective insight. Eur J Cardiothorac Surg 2003;23:439-45. [Crossref] [PubMed]
Cite this article as: Ramesh N, Velotta JB. Pneumonectomy in an elderly patient with congenital unilateral lung hypoplasia and recurrent Aspergillus: a case report. AME Case Rep 2023;7:9.



