
Cutaneous lymphadenoma in a young Saudi female: a case report
Introduction
Cutaneous lymphadenoma (CL) is a rare tumor that was first described in 1987 (1). The main pathogenesis is not yet fully understood; it may represent a form of basal cell carcinoma (BCC) with pilar or eccrine differentiation (1). Histologically, CL are well-circumscribed nests of dermal basaloid cells with peripheral palisading. Cells are pale in the center of the nests and lymphocytes surround the stroma (2).
To date, there are fewer than 60 cases reported, with extremely rare occurrence in Asian inhabitants. To our knowledge, this is the first case of CL to be reported in the Arabian Gulf countries. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-2/rc).
Case presentation
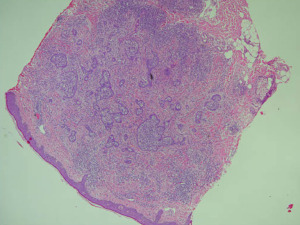
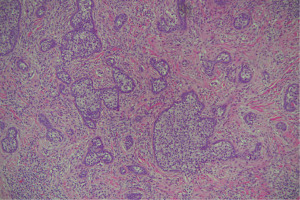
A 28-year-old healthy Saudi female presented to the outpatient clinic of the Dermatology Department in King Khalid University Hospital in January 2020 with a complaint of a completely asymptomatic skin lesion on her forehead that first appeared eight years back. The lesion was stable in size; new lesions had not appeared and other body areas had not been affected. Her main concern was only the appearance. Her past medical and surgical histories were unremarkable. No previous episodes of the same lesion had occurred in herself or her family. Physical examination showed a solitary, nontender, firm, skin-colored to pink nodule on the left side of her forehead with overlying telangiectasia. It measured 3 mm × 3.4 mm, and dermoscopic examination revealed pink-orange homogenous color with fine linear vessels. Differential diagnoses considered included trichoepithelioma, syringoma or BCC. A 4-mm skin punch biopsy was performed, and the pathology report revealed a well circumscribed dermal tumor made of irregularly shaped, differently sized nests of epithelial cells, with moderately dense inflammatory infiltrates (Figure 1). The tumor was made of epithelial nests of uniform, small basaloid cells with some peripheral palisading, with more pale to focally clear cells in the centers of the nests. The stroma was fibrotic, and some was connected to epithelial islands. Lympho-histiocytic inflammatory infiltrates were evident surrounding the tumor, with some within the tumor itself. There were no retraction artifacts, atypia or necrosis (Figure 2). Based on the clinical picture and histopathology results; the lesion was diagnosed as CL. The lesion was fully excised by skin punch biopsy without any residual tumor either clinically or histologically. The patient remains free of disease at the 1-year follow-up, with no complaints.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
CL is a benign skin neoplasm that affects individuals of both genders aged between 14 to 87 years. It is located in the head and neck area and rarely affects other sites, such as the extremities and lower back. Clinically, it presents as flesh-colored asymptomatic nodules for many months to years without any changes. It mimics BCC in the first clinical impression (3,4). Our case confirms the demographic data and clinical presentation of this tumor. The dermoscopic features seen in our case were nonspecific, and after searching the English literature, we did not find any dermoscopy findings mentioned in the reported cases.
Santa Cruz and Barr were the first to describe this uncommon tumor, which they renamed CL in 1991 (1). CL histogenesis is hugely debated; based on immunohistochemical studies, it is thought that it represents a variant of trichoblastoma and that the tumor origin is the hair follicle. Currently, CL is considered as a variant of nodular trichoblastoma with adamantinoid features as classified by the World Health Organization (5). Our patient’s case history supports the benign process of the tumor since she had it for the past 8 years without any changes in size, shape, symptoms or number of lesions.
The peculiar pathological findings of this unique subtype of trichoblastoma include the presence of epithelial nests of basaloid cells with peripheral palisading and clear cells in the centers of the nests, along with fibrous stroma and lymphocytic infiltrates surrounding the tumor (3). These findings support and confirm the diagnosis of cutaneous lymphadenoma in our patient, which has never been reported in Saudi Arabia before. In addition, the condition is extremely rare in the Asian population. After reviewing the English literature, there were only 4 Asian cases of cutaneous lymphadenoma reported to date, which could be due to ethnicity differences (6-9). All these 4 cases had a similar presentation, an asymptomatic, slowly growing nodule on the face (6-9). Two of these cases developed cutaneous lymphadenoma before the age of 30 (6,7).
The clinical presentation of cutaneous lymphadenoma is completely nonspecific; in turn, it may mimic a list of differentials, such as BCC, trichoepithelioma, dermatofibroma, syringoma, or any other adnexal neoplasm. The definitive diagnosis is made microscopically, based on the specific features of this unique rare tumor. The main histological differential diagnoses are clear cell variants of BCC, syringoma, and lymphoepithelioma-like carcinoma of the skin (LELC). The clear cell variant of BCC usually has some apoptotic bodies, atypia and mitosis, along with an artifact cleft filled with stromal mucin. Clear cell syringoma is evident histologically with tadpole-shaped ducts, and no dense lymphocytic infiltrate is found. LELC is characterized by islands of atypical epithelial cells with mitosis; these islands lie in the deep dermis and even the hypodermis (7).
The modality of treatment of such tumors is complete excision. Although the tumor is benign and almost never recurs, recurrence has been reported following shave excision (10). Furthermore, there is an ongoing debate about whether this tumor has a potential for malignant transformation (11). Kazakov et al. (11) reported a case with features of adamantinoid trichoblastoma histologically and possible malignant transformation—although the author supported that the case mainly represented carcinoma ab initio.
Cutaneous lymphadenoma presents a diagnostic pitfall, and many dermatologists may not recognize it in the initial clinical impression. It must be in the differential diagnosis of any asymptomatic, chronically presenting skin nodule in the head and neck area.
There are two major limitations in this report. First, we couldn’t provide a clinical examination image of the nodule prior to excision, nor could we provide a dermoscopy image to illustrate our findings. Second, cutaneous lymphadenoma is asymptomatic and not easily recognized, and therefore could be under-reported in the literature.
In conclusion, to our knowledge, this is the first case of cutaneous lymphadenoma in a Saudi patient to be reported. Although it is a rare tumor, there is a slight increase in the reporting of such neoplasms, and further studies are needed to explain the exact pathogenesis and to describe the condition’s dermoscopic features.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-2/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-2/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Santa Cruz DJ, Barr RJ, Headington JT. Cutaneous lymphadenoma. Am J Surg Pathol 1991;15:101-10. [Crossref] [PubMed]
- Goyal A, Solus JF, Chan MP, et al. Cytokeratin 17 is highly sensitive in discriminating cutaneous lymphadenoma (a distinct trichoblastoma variant) from basal cell carcinoma. J Cutan Pathol 2016;43:422-9. [Crossref] [PubMed]
- Yu R, Salama S, Alowami S. Cutaneous lymphadenoma: a rare case and brief review of a diagnostic pitfall. Rare Tumors 2014;6:5358. [Crossref] [PubMed]
- Allen JE, Lundin K, Erentaite D. Cutaneous lymphadenoma with unusual localization. J Plast Reconstr Aesthet Surg 2013;66:1300-2. [Crossref] [PubMed]
- Verdolini R, Stefanato CM. A pearly nodule on the upper eyelid. Cutaneous lymphadenoma. Clin Exp Dermatol 2010;35:561-2. [Crossref] [PubMed]
- Alsadhan A, Taher M, Shokravi M. Cutaneous lymphadenoma. J Am Acad Dermatol 2003;49:1115-6. [Crossref] [PubMed]
- Jiang Y, Chen H, Sun J. Cutaneous lymphadenoma. Indian J Dermatol Venereol Leprol 2012;78:652-4. [Crossref] [PubMed]
- Son SW, Kim YC, Kim IH. Cutaneous lymphadenoma. Clin Exp Dermatol 2005;30:89-90. [Crossref] [PubMed]
- Fujimura T, Itoigawa A, Haga T, et al. Cutaneous lymphadenoma: a case report and immunohistochemical study. Case Rep Dermatol 2012;4:50-5. [Crossref] [PubMed]
- Rajabi F, Kamyab K, Firooz A. Cutaneous Lymphadenoma: A Case of Recurrence after Shave Excision. Case Rep Dermatol Med 2021;2021:5543404. [Crossref] [PubMed]
- Kazakov DV, Banik M, Kacerovska D, et al. A cutaneous adnexal neoplasm with features of adamantinoid trichoblastoma (lymphadenoma) in the benign component and lymphoepithelial-like carcinoma in the malignant component: a possible case of malignant transformation of a rare trichoblastoma variant. Am J Dermatopathol 2011;33:729-32. [Crossref] [PubMed]
Cite this article as: Aldihan R, Alsubait N, Alhaddab M. Cutaneous lymphadenoma in a young Saudi female: a case report. AME Case Rep 2022;6:26.


