
Incidental paratracheal lymph node lung adenocarcinoma in a patient with goiter: a case report
Introduction
The paratracheal lymph nodes can be sites of metastasis for many malignancies including lung, esophagus, thyroid, and lymphoma (1,2). Depending on the tissue of origin, these metastases are treated differently: patients with head and neck cancers have improved regional control with resection as opposed to patients with lung and esophageal cancers who gain a survival benefit from systemic therapy (3-5). We describe a patient who underwent combined thoracoscopic and cervical resection of a multinodular goiter who was found to have incidental lung adenocarcinoma in an adjacent paratracheal lymph node despite having no pulmonary nodules. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-23/rc).
Case presentation
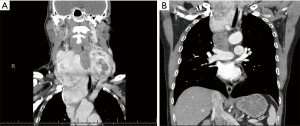
An otherwise healthy 62-year-old male with remote smoking history presented to his primary care doctor with slow growth of a known multinodular goiter for which he had undergone partial thyroidectomy 30 years before in the Philippines. He had no known radiation exposure. Family history was notable for an aunt with a goiter. He did not have any compressive symptoms and did not pursue surgery for many years as the goiter was of stable size. After repeatedly declining surgical resection, he eventually became amenable to surgery after being convinced by family and friends and was referred to otolaryngology. TSH and T4 values were within normal limits. Computed tomography imaging of the neck and chest showed a markedly enlarged multinodular thyroid gland (14.6×6.1×14.5 cm3) with extension into the mediastinum and a heterogeneous nodule (3.2×4.0×4.7 cm3) just inferior but adjacent to the presumed thyroid mass (Figure 1). After multidisciplinary review, it was thought that the thyroid gland nodule were parts of one benign goiter. Total thyroidectomy was planned by otolaryngology, and the patient was referred to thoracic surgery given possible need for median sternotomy due to the retrosternal component.
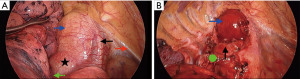
The patient underwent a total thyroidectomy via a right video-assisted thoracoscopic (VATS) and cervical approach. The patient was positioned in left lateral decubitus with 3 ports placed: camera port in the 7th intercostal space in the mid axillary line, posterior port in the 6th intercostal space in the posterior axillary line behind the scapula tip, and working anterior port in the 4th intercostal space in the anterior axillary line. The goiter was first completely dissected off the trachea, arch of the aorta, superior vena cava, and innominate artery via right VATS approach. The goiter was also successfully dissected off the vagus nerve and right recurrent laryngeal nerve. It was noted intraoperatively that what was thought preoperatively to represent the inferior portion of the goiter was actually a separate firm adherent 4 cm lymph node adjacent to the trachea and superior vena cava. This necrotic right paratracheal lymph node in the 4R location was meticulously completely dissected off the aorta, superior vena cava, and trachea using a combination of blunt and electrocautery dissection (Figure 2). Intraoperative frozen section of the lymph node revealed carcinoma of unknown origin. The goiter was then removed through a neck incision by otolaryngology. The patient was discharged on postoperative day 1 after removal of his 28 French chest tube. He re-presented to the emergency department later that day with increased neck swelling. His oxygen saturation was stable, and chest radiograph showed subcutaneous emphysema of the neck without right pneumothorax. He was observed with serial neck measurements and discharged the next day after significant improvement in neck crepitus and stable appearance of repeat chest radiographs. He was seen for follow up 3 days later at which point his neck swelling had further decreased, and his surgical drain was removed without issue.
His final surgical pathology showed hyperplastic thyroid nodules consistent with a benign thyroid goiter along with a poorly differentiated thyroid transcription factor 1-positive (TTF-1) positive carcinoma measuring 4 cm in size involving a cluster of several smaller lymph nodes concerning for lung adenocarcinoma with unknown primary. Tumor propensity scoring of programmed death-ligand 1 (PD-L1) expression showed 91–100%. He underwent a postoperative positron emission tomography scan which did not show any overt metastatic disease or lung nodules. He underwent multidisciplinary tumor board evaluation and was staged as TxN3M0 lung adenocarcinoma. He is currently undergoing definitive chemotherapy to the 4R nodal basin with cisplatin and pemetrexed and has been referred to radiation oncology. He will also eventually receive durvalumab. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Substernal thyroid goiter has been shown to require median sternotomy in 5–10% of cases. Risk factors associated with sternotomy include presence of goiter greater than 160 months, extension into the posterior mediastinum, subcarinal space or below the aortic arch,, and increased thyroid density, which is the strongest factor increasing the risk of sternotomy 47-fold (6). In the present case, dissection of the goiter via a right thoracoscopic approach spared the patient morbidity of a median sternotomy. This was achievable despite the goiter’s large size of 14.5 cm, extension beyond the aortic arch into the posterior mediastinum, and proximity to the pleura, great vessels, and trachea due to better visualization of the paratracheal space via a right thoracoscopic approach compared to that of a median sternotomy. The utility of a minimally invasive thoracic approach is further appreciated in a goiter with significant abutment of these vital structures which can further increase the risk of injury with a transcervical excision alone. Likewise, the 4R lymph node was able to be clearly seen to be separate and completely removed intact through a minimally invasive fashion. Even though the patient was shortly readmitted after discharge for neck crepitus, he was ultimately discharged home on postoperative day 2 with minimal pain and no longstanding pulmonary complications.
Another notable feature of this case is the final pathology of benign goiter and the paratracheal lymph node revealing an immunophenotype suggestive of lung adenocarcinoma. Given the lack of pulmonary nodules on imaging and the patient’s large goiter, the unexpected intraoperative finding of a suspicious paratracheal node with frozen pathology showing carcinoma was concerning for a primary lesion of head and neck origin instead of pulmonary. As nodal dissection is generally associated with improved regional control in head and neck cancers, the lymph node was resected completely despite its aggressive intraoperative features rather than simply biopsied. For example, cervical lymphadenectomy has been historically recommended in cases of nodal metastasis in differentiated thyroid cancer (7). However, the role of mediastinal node dissection in this case is controversial. In hindsight, the patient could have been spared resection of the lymph node given its pulmonary origin as the standard of care for stage IIIB non-small cell lung cancer is definitive chemoradiation and adjuvant immunotherapy (8). However, the patient did not suffer any increased morbidity by resection of the nodal tissue as the whole procedure was able to occur in a minimally invasive fashion.
One of the strengths of this case report is the availability of all clinical information including labs and imaging across multiple disciplines and institutions within one integrated health care system. Limitations include limited follow up as the patient just initiated definitive chemoradiation.
In conclusion, we describe a case of a patient with large substernal multinodular goiter who underwent combined thoracoscopic and cervical resection. Noteworthy to this case is the minimally invasive approach preventing the need for median sternotomy and preventing any increased morbidity for the patient’s incidentally found TxN3M0 lung adenocarcinoma. The unexpected final pathology would have changed his management from resection to definitive chemoradiation and adjuvant immunotherapy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-23/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-23/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharma A, Fidias P, Hayman LA, et al. Patterns of lymphadenopathy in thoracic malignancies. Radiographics 2004;24:419-34. [Crossref] [PubMed]
- Shirley LA, Jones NB, Phay JE. The Role of Central Neck Lymph Node Dissection in the Management of Papillary Thyroid Cancer. Front Oncol 2017;7:122. [Crossref] [PubMed]
- Arbour KC, Riely GJ. Systemic Therapy for Locally Advanced and Metastatic Non-Small Cell Lung Cancer: A Review. JAMA 2019;322:764-74. [Crossref] [PubMed]
- Ho AS, Kim S, Tighiouart M, et al. Association of Quantitative Metastatic Lymph Node Burden With Survival in Hypopharyngeal and Laryngeal Cancer. JAMA Oncol 2018;4:985-9. [Crossref] [PubMed]
- Fang R, Peng L, Chen L, et al. The survival benefit of lymph node dissection in resected T1-2, cN0 supraglottic cancer: A population-based propensity score matching analysis. Head Neck 2021;43:1300-10. [Crossref] [PubMed]
- McKenzie GA, Rook W. Is it possible to predict the need for sternotomy in patients undergoing thyroidectomy with retrosternal extension? Interact Cardiovasc Thorac Surg 2014;19:139-43. [Crossref] [PubMed]
- Wang LY, Ganly I. Nodal metastases in thyroid cancer: prognostic implications and management. Future Oncol 2016;12:981-94. [Crossref] [PubMed]
- Antonia SJ, Villegas A, Daniel D, et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. N Engl J Med 2018;379:2342-50. [Crossref] [PubMed]
Cite this article as: Kwak HV, Banks KC, Hsu DS, Debbaneh PM, Wang KH, Velotta JB. Incidental paratracheal lymph node lung adenocarcinoma in a patient with goiter: a case report. AME Case Rep 2022;6:29.


