
Conservative management of a specific subtype of Maisonneuve fractures: a report of two cases
Introduction
Maisonneuve fractures are characterised by a pattern of the following lesions: a medial malleolar fracture or deltoid ligament rupture, a disruption of the ankle syndesmosis ligaments and a fracture of the proximal fibula. It was originally described by the French surgeon Jules Germain François Maisonneuve in 1840 (1). Diagnosis is often overlooked and probably occurs more often than assumed; among ankle fractures, Maisonneuve fractures accounting for 0.7% to 10% in some studies (2-4). It is frequently a sport-related injury, occurring in a relatively young population (4-6).
The main injury mechanism proposed is an external rotation of a pronated and fixed foot (1). The sequence of the injury is described as follows: the talus performs an external rotation and creates a strain on the medial column of the mortise. The force is then transmitted anteriorly, with the talus acting as a wedge, resulting in rupture of the anterior tibiofibular and interosseous ligaments. Disruption of the interosseous membrane (IOM) usually progresses to the neck of the fibula with a concomitant spiral fracture. Lesions most frequently associated with Maisonneuve fractures are the interosseous and anterior inferior tibiofibular ligaments (AITFL), the posterior malleolus, the deltoid ligament and the medial malleolus (7). Posterior tibiofibular ligament (PTFL) may be intact, resulting in partial diastasis of the mortise (8). The ankle joint can be considered as 2 columns: medial and lateral. Some authors consider the ankle as a ring where the bone and ligament structures contribute to its stability. If the ring is ruptured on one place, which means that only one column is broken, the joint remains stable. But if it is ruptured on 2 places, it becomes unstable. Therefore, in theory, a Maisonneuve fracture is unstable, since both columns are affected (9).
Maisonneuve fractures are a part of syndesmotic lesions. Syndesmosis lesions reach a consensus in the literature for surgical treatment in case of diastasis of the distal tibiofibular joint or associated fracture around the ankle (10-12). It is admitted that a syndesmosis lesion may be associated with a significant instability of the joint, which could lead to osteoarthritis if not adequately stabilized (13).
For ankle fractures in general, it is recognized that restoring anatomical congruence to the ankle joint is important to improve function and decrease post-traumatic osteoarthritis. Surgical or conservative methods are employed to allow the joint to heal in this sense. According to two recent meta-analyses, there is, to date, insufficient evidence to say which modality is the best to treat an ankle fracture considered unstable (14,15).
However, in most studies about the management of a Maisonneuve fracture, surgical stabilization of the syndesmosis is the first choice regardless of syndesmotic stability (16).
Nevertheless, some authors recommend conservative treatment for certain type of Maisonneuve fractures in case of partial disruption of the syndesmosis, in the absence of diastasis, or in the absence of ligament or bone lesion of the medial malleolus (8,17). However, posterior syndesmotic injury in the form of tibial avulsion fracture of the posterior inferior tibiofibular ligament (PITFL) (considered equivalent to a posterior malleolus fracture) was not considered in these studies, nor was the role of the medial column. Outcomes of conservative treatment are rarely described in the literature. The last comparison study was published in 1998 and found better outcomes in the operative group (18). Charopoulos et al. (19) published a case report of conservative treatment of a Maisonneuve fracture with integrity of the deltoid ligament, and with a non-weight bearing protocol.
Literature does not establish well-defined criteria for the decision of conservative treatment for Maisonneuve fractures. The purpose of this study was to describe for the first time the outcomes of two patients with Maisonneuve fracture injuries associated with an avulsion fracture of the PITFL and an intact deltoid ligament, treated successfully by conservative therapy with an early weight bearing protocol. Information from this report should provide a useful reference for physicians who treat these injuries. We present the following two cases in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-21-67/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the two patients for publication of these two cases and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The first patient was a 40-year-old man who presented to the emergency department after a skiing accident with external rotation trauma of the ankle. The second patient was a 50-year-old woman who twisted her ankle in a fall down to the stairs. Clinical examinations revealed ankle swelling and tenderness on palpation of the ankle and also proximal fibula.
For both patients, radiographs at day 1 demonstrated a Maisonneuve fracture with an associated fracture of the posterior malleolus without talar subluxation (Figures 1,2).
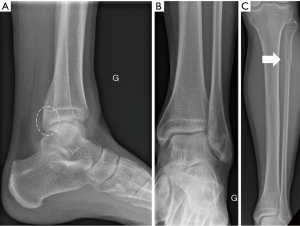
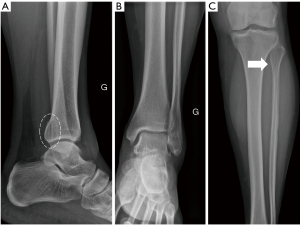
At one week post-injury, radiological evaluation was completed with out of plaster weight-bearing radiographs, which showed no fracture displacement or diastasis of the distal tibio-fibular joint. Although stress radiographs are recommended to establish an accurate diagnosis (3), for reasons related to patient pain and anxiety and the need for anesthesia, we did not obtain such exams. Instead, magnetic resonance imaging (MRI) was performed in an effort to more accurately assess the status of the soft tissues and showed no rupture of the deltoid ligament, an intact PITFL, and a fibula anatomically positioned in the tibial notch (Figure 3,4). Complete MRI workup of the ankle ligaments can be found in Table 1.
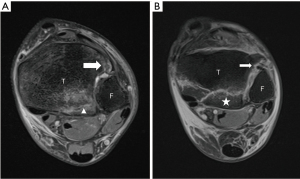
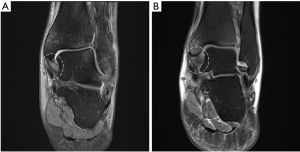
Table 1
| Anatomical structure | Case 1 | Case 2 |
|---|---|---|
| DL | Intact | Intact |
| AITFL | Tibial bony avulsion | Mid-substance rupture |
| PITFL | Tibial bony avulsion | Tibial bony avulsion |
| FCL | Rupture | Intact |
| IOM | Intact | Intact |
| Fibula in tibial notch | Centered | Centered |
MRI, magnetic resonance imaging; DL, deltoid ligament; AITFL, anterior inferior tibiofibular ligament; PITFL, posterior inferior tibiofibular ligament; FCL, fibula-calcaneal ligament; IOM, interosseous membrane.
Both patients were treated with a short leg walking cast for 6 weeks and were advised with partial weight-bearing aided by two crutches. After cast removal they were allowed to gradually begin full weight-bearing, under the supervision of the physiotherapist.
Standing radiographs at 6 and 12 weeks post-injury showed fracture healing and confirmed stability of the ankle (Figure 5).

Both patients were able to walk without limitation at 3 months after the injury. At 1 year, full range of motion of the ankle joint was achieved and the AOFAS scores were 90/100 and 82/100 for the first and second patients respectively. The second patient reported chronic ankle pain for several years related to hyperlaxity dating from before the accident.
Discussion
Clinical examination of the traumatic ankle includes an inspection of the skin followed by a palpation of deltoid ligament, lateral ligaments, syndesmosis and proximal fibula. If the proximal fibula shows tenderness, radiographs of the entire leg is mandatory (2). This allowed us to detect the two cases presented in this article. The workup was completed by weight-bearing radiographs, which attested to the stability of the syndesmosis throughout the follow-up.
Maisonneuve fractures don’t have a specific classification. They are integrated into several commonly used classifications for ankle fractures. Pankovich developed a 5-stage classification based on the successive development of lesions leading to a Maisonneuve fracture (20). Fracture of the proximal fibula occurs in the fourth stage of the classification, while the rupture of the deltoid ligament or the fracture of the medial malleolus correspond to the fifth stage. In the Lauge-Hansen classification, Maisonneuve fracture is a subtype of pronation external rotation trauma (PER) of stage 3 (fracture of the fibula above the mortise) up to stage 4 (fracture of the posterior malleolus or PITFL injury) (21). In the current cases, the fractures may be classified as PER 4 according to Lauge-Hansen. In the PER subtypes, deltoid ligament rupture or medial malleolus fracture is present as early as stage 1. In contradiction to this classification, our two patients did not show either of these two lesions significantly. This contradiction shows that it cannot be based only on these classifications, because Maisonneuve fractures are apparently a continuum of different lesions, which cannot be integrated into one classification. Thus, to decide on a treatment, it appears important to make a thorough assessment of the lesions.
Based on the fracture stability of our patients on radiographs, we raised the possibility of conservative treatment. In this context, we chose to assess the ligament and cartilage lesions in details before deciding on such a treatment modality.
An important point to evaluate for conservative treatment is the competence of the medial structures. The medial column has been considered for the last 20 years, following various cadaveric studies, as the most important structure in the stability of the mortise.
A study by Michelsen tested the loading of cadaveric ankles by progressively simulating the different fracture stages of the SER classification according to Lauge-Hansen. It showed that the stability of a loaded ankle is mainly due to the deltoid ligament (22).
The absence of damage to the deltoid ligament and the medial malleolus, as in the Masionneuve fractures of our two patients, allowed to preserve the integrity of one column out of two of the ankle joint and thus to consider it as stable. This point, in line with Michelsen’s study, made us feel comfortable with an early weight-bearing protocol, especially since the mortise remained in an anatomical position during weight-bearing radiographs. The fact that the IOM was not affected in our two patients also supported this choice of management.
As biomechanical studies have shown (23), the stability of the syndesmosis is mainly determined by the PITFL. In our 2 cases, the posterior syndesmosis was affected only in the form of bony tibial avulsion of the PITFL, equivalent to a posterior malleolar fracture. MRI demonstrated the absence of mid-substance ligament damage, talar subluxation or articular impaction, which would have required surgical stabilization (24). MRI also demonstrated the integrity of the IOM in our two patients. Although Maisonneuve’s fracture is often associated with gross instability of the ankle, some authors have described it in association with a partial diastasis making the syndesmosis relatively stable because of the persistence of the IOM and the PITFL (8). Subsequent radiographs did not show any secondary displacement of the posterior malleolus, which would support our hypothesis, suggesting that a non-displaced PITFL bone avulsion has a better healing potential than a pure ligamentous injury of the PITFL. Thus, in association with an intact IOM, we can also, in our opinion, consider syndesmosis as relatively stable. In addition, the presence of the bone lesion has the advantage of allowing radiographic monitoring of PITFL healing in position, unlike a mid-substance PITFL lesion.
We have advocated that in addition to stability of the ankle, positioning of the fibula in the fibular notch is of paramount. Weening et al. (25) emphasized the importance of the correct position of the distal fibula, as this means that the distal tibio-fibular joint is anatomically reduced and this is a very important factor for a good functional outcome. Methods are described to evaluate the correct positioning of the fibula in its notch. We were able to confirm, using that of Bartoníček et al. and Futamura et al. (7,26) that the positioning in our cases was anatomical.
The results of fibular malpositioning, especially as a result of surgical treatment, have shown poor results (27). Thus, anatomical positioning of the fibula in its notch is fundamental to consider a conservative treatment. Even with proper fibular position on mortise and lateral views, malposition of the fibula in its tibial notch may be possible, as shown in a study of 24 patients who underwent syndesmosis fixation with screws followed by postoperative CT monitoring of repositioning (26). We believe that a CT or an MRI are mandatory if conservative treatment is being considered, and not to rely solely on radiographs.
In the current cases, we observed that conservative treatment of Maisonneuve fractures with a non-displaced posterior malleolus lesion and integrity of the medial structures provides good clinical and radiological results, considering that the following criteria were obtained. In addition, we believe that a weight-bearing protocol can be introduced if these criteria are met and that it will lead to results comparable to a non-weight bearing protocol such as the one that Charopoulos et al. (19) introduced for his Maisonneuve fracture case with medial column integrity.
Criteria for conservative treatment of Maisonneuve fracture proposed in regard to this study:
- Initial radiographs with an anatomic position of the mortise without diastasis.
- Fracture of the posterior malleolus without talar subluxation or articular impaction.
- Persistence of anatomic mortise position on follow-up weight-bearing radiographs.
- Absence of secondary displacement of the posterior malleolus on weight-bearing radiographs at follow-up.
- CT-scan or MRI showing good position of the distal fibula in its tibial notch.
- Absence of deltoid ligament rupture on MRI.
Conclusions
We report two cases of Maisonneuve fracture with posterior malleolus fracture and integrity of the medial structures. Following a detailed analysis of anatomic injury characteristics, we suggest that these lesions are at low secondary displacement risk provided they meet the criteria presented in this article. Based on the experience of these patients, in contrast to other subtypes of Maisonneuve fractures, we recommend conservative treatment for these lesions.
Further studies comparing operative and conservative treatments should be performed to validate the above criteria. In the future, if some Maisonneuve fractures could be treated conservatively, this may reduce the number of surgical treatments, their complications, and also reduce the length of hospital stay and potential costs.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-21-67/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-21-67/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-21-67/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the two patients for publication of these two cases and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maisonneuve MJG. Recherches sur la fracture du perone. Arch Gen Med 1840;7:165-87.
- Duchesneau S, Fallat LM. The Maisonneuve fracture. J Foot Ankle Surg 1995;34:422-8. [Crossref] [PubMed]
- Gudas CJ. Current concepts in the management of the ankle repair. In: American College of Foot Surgeons. Complications in foot surgery: Prevention and management. Baltimore, MD, USA: Williams & Williams, 1976.
- Babis GC, Papagelopoulos PJ, Tsarouchas J, et al. Operative treatment for Maisonneuve fracture of the proximal fibula. Orthopedics 2000;23:687-90. [Crossref] [PubMed]
- Sproule JA, Khalid M, O'Sullivan M, et al. Outcome after surgery for Maisonneuve fracture of the fibula. Injury 2004;35:791-8. [Crossref] [PubMed]
- Obeid EM, Amr M, Hirst P, et al. Percutaneous fixation of Maisonneuve and Maisonneuve-type fractures: a minimally invasive approach. Injury 1998;29:619-22. [Crossref] [PubMed]
- Bartoníček J, Rammelt S, Kašper Š, et al. Pathoanatomy of Maisonneuve fracture based on radiologic and CT examination. Arch Orthop Trauma Surg 2019;139:497-506. [Crossref] [PubMed]
- Merrill KD. The Maisonneuve fracture of the fibula. Clin Orthop Relat Res 1993;218-23. [PubMed]
- Gougoulias N, Sakellariou A. When is a simple fracture of the lateral malleolus not so simple? how to assess stability, which ones to fix and the role of the deltoid ligament. Bone Joint J 2017;99-B:851-5. [Crossref] [PubMed]
- Hunt KJ, Phisitkul P, Pirolo J, et al. High Ankle Sprains and Syndesmotic Injuries in Athletes. J Am Acad Orthop Surg 2015;23:661-73. [Crossref] [PubMed]
- Schnetzke M, Vetter SY, Beisemann N, et al. Management of syndesmotic injuries: What is the evidence? World J Orthop 2016;7:718-25. [Crossref] [PubMed]
- Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther 2006;36:372-84. [Crossref] [PubMed]
- Jeong BO, Baek JH, Song WJ. Ankle Arthritis Combined With Chronic Instability of the Syndesmosis After Ankle Fracture With Syndesmotic Injury: A Case Report. J Foot Ankle Surg 2018;57:1000-4. [Crossref] [PubMed]
- Donken CC, Al-Khateeb H, Verhofstad MH, et al. Surgical versus conservative interventions for treating ankle fractures in adults. Cochrane Database Syst Rev 2012;CD008470. [Crossref] [PubMed]
- Javed OA, Javed QA, Ukoumunne OC, et al. Surgical versus conservative management of ankle fractures in adults: A systematic review and meta-analysis. Foot Ankle Surg 2020;26:723-35. [Crossref] [PubMed]
- Stufkens SA, van den Bekerom MP, Doornberg JN, et al. Evidence-based treatment of maisonneuve fractures. J Foot Ankle Surg 2011;50:62-7. [Crossref] [PubMed]
- Lock TR, Schaffer JJ, Manoli A 2nd. Maisonneuve fracture: case report of a missed diagnosis. Ann Emerg Med 1987;16:805-7. [Crossref] [PubMed]
- Wang M, Jiang C, Yang S, et al. Maisonneuve fracture of the fibula: clinical and experimental study. Zhonghua Wai Ke Za Zhi 1998;36:658-60,133.
- Charopoulos I, Kokoroghiannis C, Karagiannis S, et al. Maisonneuve fracture without deltoid ligament disruption: a rare pattern of injury. J Foot Ankle Surg 2010;49:86.e11-7. [Crossref] [PubMed]
- Pankovich AM. Maisonneuve fracture of the fibula. J Bone Joint Surg Am 1976;58:337-42. [Crossref] [PubMed]
- Tartaglione JP, Rosenbaum AJ, Abousayed M, et al. Classifications in Brief: Lauge-Hansen Classification of Ankle Fractures. Clin Orthop Relat Res 2015;473:3323-8. [Crossref] [PubMed]
- Michelsen JD, Ahn UM, Helgemo SL. Motion of the ankle in a simulated supination-external rotation fracture model. J Bone Joint Surg Am 1996;78:1024-31. [Crossref] [PubMed]
- Michelson JD, Hamel AJ, Buczek FL, et al. Kinematic behavior of the ankle following malleolar fracture repair in a high-fidelity cadaver model. J Bone Joint Surg Am 2002;84:2029-38. [Crossref] [PubMed]
- White TO. In defence of the posterior malleolus. Bone Joint J 2018;100-B:566-9. [Crossref] [PubMed]
- Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 2005;19:102-8. [Crossref] [PubMed]
- Futamura K, Baba T, Mogami A, et al. Malreduction of syndesmosis injury associated with malleolar ankle fracture can be avoided using Weber's three indexes in the mortise view. Injury 2017;48:954-9. [Crossref] [PubMed]
- Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma 2012;26:439-43. [Crossref] [PubMed]
Cite this article as: Dietrich G, Prod’homme M, Müller J, Ballhausen T, Helfer L. Conservative management of a specific subtype of Maisonneuve fractures: a report of two cases. AME Case Rep 2022;6:17.


