Concomitant umbilical endometriosis with catamenial pneumothorax: a case report
Introduction
Catamenial pneumothorax is a rare pathology among females with spontaneous pneumothorax, accounting for only 7% of all cases of pneumothorax in women of reproductive age (1). This disease is the most common form of thoracic endometriosis syndrome and also represents a subset of extra-pelvic endometriosis (2). The umbilical endometriosis is also a rare manifestation of extra-pelvic endometriosis and when it occurs together with catamenial pneumothorax this remarks the uniqueness of this case.
Here, we report a unique case of a woman who presented with concomitant catamenial pneumothorax and umbilical endometriosis. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-21-70/rc).
Case presentation
This case report was approved by the Institutional Review Board of Vajira hospital, Navamindradhiraj University (COE number: 17/2021X). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
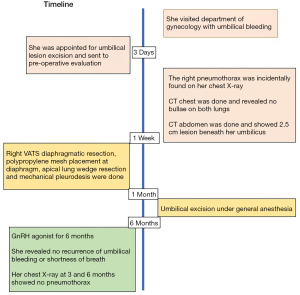
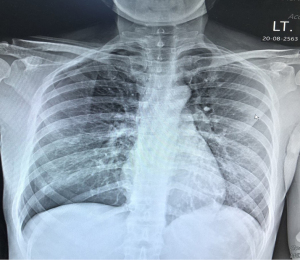
A 35-year-old Thai female presented with umbilical pain and bleeding during her menstrual period for 3 months (Figure 1). At first, she was scheduled for excision of umbilical lesion and was sent for pre-operative evaluation as shown in the timeline (Figure 2). She neither had any chest pain nor shortness of breath. She also didn’t have any history of smoking. She denied any history of pneumothorax in her relatives. At physical examination, the primary care doctor didn’t note any abnormal in respiratory examination and the both sides of breath sound showed equal. Right pneumothorax was incidentally found on her chest X-ray during pre-operative evaluation for umbilical lesion excision. (Figure 3). Chest and abdominal computed tomography revealed a 2.5-cm enhancing lesion below the umbilicus, without any bullae within the lung parenchyma (Figure 4). Pelvic examination and ultrasonography did not show any abnormalities in the ovaries or uterus.
As a result, the patient was diagnosed as concomitant Catamenial pneumothorax and umbilical endometriosis. The interesting aspect of this case is the primary doctor didn’t suspect of Catamenial pneumothorax and didn’t request for CT chest but for us as a thoracic surgeon who have a high index of suspicious in young female with pneumothorax may be a Catamenial pneumothorax is the one who request it. Therefore, the cardiothoracic surgery department was consulted for the management of right pneumothorax.
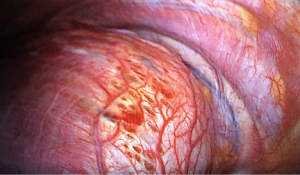
After discussing the risks and benefits of video-assisted thoracoscopic surgery (VATS) with the patient and risk of recurrent pneumothorax if treated conservatively, we performed VATS procedure to explore the thoracic cavity as single-port VATS technique. Intraoperatively, we found a diaphragmatic fenestration defect (Figure 5), and the lung parenchyma appeared to be normal. Therefore, we performed a partial diaphragmatic resection, followed by the placement of continuous 2-0 polypropylene sutures and implantation of a polypropylene mesh. Then, an endo-stapler was used to resect an apical lung wedge, and mechanical pleurodesis was performed to create pleural adhesion. Upon completion of surgery, an intercostal chest drain was inserted. On the next day, drain was removed and patients was discharge on the day after. For umbilical lesion, the patient was schedule for excision under general anesthesia after a month of lung surgery.
Pathological analysis of the tissue specimens obtained from both the diaphragm and umbilicus suggested the presence of endometriosis. Hence, following consultation with a gynecologist, we initiated hormonal therapy with a gonadotropin-releasing hormone agonist to control her extra-pelvic endometriosis. At 3- and 6-month follow-ups, the patient had no evidence of umbilical bleeding or recurrent pneumothorax on chest X-ray. The patient also revealed she had a better quality of life, denied any adverse events and volunteered to be in a part of this case report.
Discussion
Umbilical endometriosis, which is a rare form of extra-pelvic endometriosis, is hypothesized to be caused by endometrial cells migrating via hematogenous or lymphatic routes. It may manifest as swelling, pain, or bleeding of the umbilicus (2). Catamenial pneumothorax represents another rare form of extra-pelvic endometriosis and is most likely to result from the clockwise flow of the peritoneal fluid containing endometrial cells. This can explain why the right side is more frequently affected than the left side (1).
To the best of our knowledge, there are only 2 cases of concomitant catamenial pneumothorax and umbilical endometriosis in the literatures (3,4), with the case presented herein being the third report of its kind. Numerous theories, such as the retrograde menstruation theory, coelomic metaplasia, and hematogenous or lymphatic dissemination, have been put forward to explain how endometrial cells spread to extra-pelvic sites. Here, we believe that retrograde menstruation might have been at play, that is, endometrial cells might have reached the right subdiaphragmatic area and umbilicus due to the clockwise flow of the peritoneal fluid. When endometrial cells created the pores at diaphragm, air can pass through these and result in pneumothorax.
Although the main strategy for the treatment of extrapelvic endometriosis involves hormonal therapy with gonadotropin-releasing hormone agonists or oral contraceptive drugs, it is suggested that surgery should also be performed to help sufficiently control the disease and achieve the best possible outcomes in these patients (1,5). However, the gonadotropin-releasing hormone agonists do have benefits in term of avoiding recurrence up to 4 years of follow-up and is suggested to be an adjunct to surgical treatment from BTS guideline 2010 (6). From current literature review, there is no standard guideline recommendation in term of duration of treatment. Our gynecologist prefers to extend the treatment for 6–12 months as same as in pelvic endometriosis.
In conclusion, as a holistic care approach, it is essential to search for other manifestations of extrapelvic endometriosis in patients with catamenial pneumothorax and treat the patient with multidisciplinary team.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-21-70/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-21-70/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-21-70/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This case report was approved by the Institutional Review Board of Vajira hospital, Navamindradhiraj University (COE number: 17/2021X). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gil Y, Tulandi T. Diagnosis and Treatment of Catamenial Pneumothorax: A Systematic Review. J Minim Invasive Gynecol 2020;27:48-53. [Crossref] [PubMed]
- Hirata T, Koga K, Osuga Y. Extra-pelvic endometriosis: A review. Reprod Med Biol 2020;19:323-33. [Crossref] [PubMed]
- Arunthari V, Sevin BU, Krishna M, et al. Catamenial pneumothorax with umbilical and diaphragmatic endometriosis: a case report and review of the literature. South Med J 2008;101:1043-5. [Crossref] [PubMed]
- Mowad C, Andreychik C, Murphy T. Umbilical endometriosis elucidates cause of recurrent pneumothorax. J Am Acad Dermatol 2014;71:e79-80. [Crossref] [PubMed]
- Laohathai S, Wannadilok P, Poopipatpab S, et al. Nonintubated Video-Assisted Thoracoscopic Surgery Using Local Anesthesia for Catamenial Pneumothorax. Ann Thorac Surg 2021;111:e245-6. [Crossref] [PubMed]
- MacDuff A, Arnold A, Harvey JBTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65:ii18-31. [Crossref] [PubMed]
Cite this article as: Yu J, Laohathai S. Concomitant umbilical endometriosis with catamenial pneumothorax: a case report. AME Case Rep 2022;6:16.