
Machine-vision image guided C4-C5 unilateral cervical pedicle screw insertion: case report and review of literature
Introduction
Roy-Camille performed the first posterior cervical screw fixation in 1979. Since then, middle and lower cervical spine fixation methods have evolved (1). Cervical spine fixation by pedicle screws is an established technique at C2 and C7, this technique is more challenging in the C3 to C6 region as the pedicles are frequently smaller in size as compared to C2 and C7 (2).
Over the past decade, spinal surgery has significantly evolved as a result of increased need for spinal fusion procedures. The number of spinal fusion procedures have risen in recent decades, and is expected to continue to steadily rise in the coming decades as the population ages (3). Computer-assistance was introduced to improve accuracy and safety of operative procedures; however, successful implementation of posterior cervical instrumentation remains a challenge. A posterior approach is most common, with lateral mass screws inserted and fixated using rods (4). Since pedicles in the cervical spine are smaller, there are risks such as injury to the spinal cord and nerve roots, or injury to the vertebral artery by placing pedicle screws in this area. Also due to the very lateral to medial angulation of the cervical pedicle trajectory, cervical pedicles are rarely performed because of the significantly wide and morbid exposure required in order to insert the screws in this area. As such, cervical pedicle screws at the C3-6 levels are less commonly performed.
Computer-assisted navigation aims to improve the accuracy of screw placements at all spinal levels. While it has been reported that 12–40% of cervical pedicle screws inserted using freehand techniques have breached outside of the intended trajectory, the use of neuronavigation hopes to reduce the breach rate to under 10%, which should in turn lower the risk of acute neurovascular injury and longer-term mechanical construct failure (5). The operation discussed in this case report used machine vision and optical topographical navigation (7D Surgical Inc., Toronto, Canada) to co-register bony anatomy with pre-existing imaging without using any radiation. Registration is rapid and can be repeated within seconds if the patient tracker is displaced. Unique to this spinal navigation system, it can capture >480,000 data points in a 40×30 cm area with a 4–6 points/mm2 resolution (6).
We present the following article in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/acr-21-62) (7).
Case presentation
A 49-year-old man fell down a flight of stairs with a subsequent brief loss of consciousness. Thereafter he was able to stand and mobilize independently. Due to persistent neck pain, he went to see his family physician and plain cervical radiographs were performed, demonstrating fractures resulting in subsequent admission to hospital for investigation.
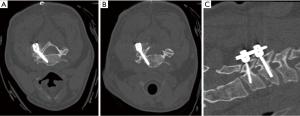
CT imaging demonstrated Klippel-Feil syndrome of C2-3, a sagittal split fracture of C4 (AO Classification type A4), and a left lateral mass fracture of C5 (AO Classification type F1) with anterior depression and 50% height loss. MRI showed STIR signal in the interspinous and supraspinous ligaments (AO Classification type B2). Paravertebral edema related to the sagittal oriented fracture of the C5 spinous process was discovered and there was fluid within the left C4-C5 facet. The fracture on C5 involved the right lamina and the spinous process. There was a nondisplaced fracture of the left C5 superior articular process. There was no dislocation or subluxation. The patient also had a left vertebral artery dissection for which consideration was taken prior to the surgery (Figure 1). Given the unstable nature of his cervical injury, the patient consented for posterior short segment C4-C5 instrumented fusion which was deemed the most appropriate treatment to provide stability while preserving range of motion, taking into consideration his Klippel-Feil syndrome.

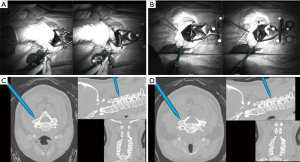
Using image guided navigation, the level and angle of the spinal fracture were registered with excellent accuracy. Registration was done in a segmental fashion to ensure accuracy by eliminating inter-segmental mobility. The complete details of navigation registration technique and workflow are covered in a prior publication (5). Briefly, the 7D Surgical navigation head unit was brought above the surgical field following standard posterior midline exposure of the cervical spine. Structured light imaging was used to generate a 3D point cloud of the exposed osseous anatomy, with high-speed automatic registration to the thin-slice pre-operative CT scan. Image guided instrumentation was then performed with optically tracked tools (5).
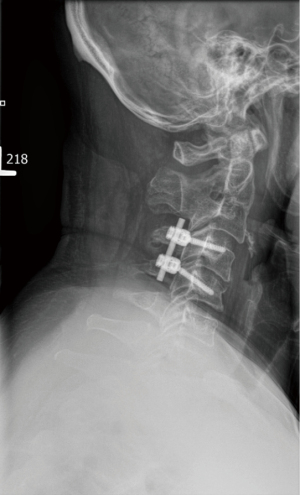
Using a navigated drill guide, the C4 and C5 pedicle screws were cannulated on the left side (Figure 2) through a separate paramedian percutaneous stab incision. The cervical instrumentation system (Zimmer Biomet Spine Inc., Westminster, CA, USA) was used to place a 4.5×24 mm pedicle screw at C4 and a 4.5×26 mm pedicle screw at C5, both on the left side. A 3.5 mm rod was placed to connect the two pedicle screws. Since these screws cannulated the pedicle as well as the anterior column for both levels, a conscious decision was made to preserve the right side as it remained uninjured.
After decortication, morselized bone graft from spinous processes were placed as autologous bone graft through a small midline incision for bone graft application for fusion. The patient tolerated the procedure well, had an unremarkable post-operative course and was discharged the following day. CT showed good placement of the left pedicle screws at C4 and C5 (Figure 3). Longer-term follow-up is needed to determine if fusion has occurred.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Cervical pedicle screws are an alternative option for posterior cervical fixation, with increased pullout and rotational strength relative to standard lateral mass instrumentation (8,9). The use of subaxial cervical pedicle screws has been limited by the relatively low margin for error afforded by the smaller pedicle diameters relative to the thoracolumbar spine, with increased potential for catastrophic neurologic or vascular injury with inaccurate placement. Multiple techniques for improving the accuracy of subaxial pedicle screw placement have been described, including intra-operative fluoroscopy, 3D-printed patient-specific drill guides, and computer-assisted navigation (4,10). Traditional navigation requires additional intra-operative radiation or significant time cost with intra-operative imaging devices. We show here a technique for safe and efficient insertion of subaxial cervical pedicle screws with machine-vision image-guidance.
In the case of this young patient, conventional lateral mass fixation would have necessitated a multilevel construct extending above and below the injured levels, significantly diminishing range of motion. With pedicle screw based fusion technique, given that the pedicles were intact, a much shorter construct from C4 to C5 provided adequate stabilization and sufficient mechanical strength since the longer pedicle screws provide both posterior and anterior column support. Pedicle screws have been found to have significantly improved pullout strength relative to lateral mass screws in both flexion, extension and axial rotation (8,9).
A unilateral left sided approach avoided the risk of injuring the only remaining intact vertebral artery for this patient. Overall, this approach provided a balanced trade-off between mechanical strength for fusion, motion preservation in the context of Klippel-Feil syndrome, and risk of arterial injury. The use of machine-vision image-guided surgery allowed accurate placement of C4 and C5 pedicle screws through a separate paramedian stab incision, with a small midline incision for bone graft application for fusion.
The machine vision image guidance system (7D Surgical) is substantially more time efficient than an intraoperative CT-based navigation system. As shown in Table 1, the 7D navigation system took under 2 min to register the points of both vertebrae. Comparatively, an intraoperative CT-based navigation system could take between 5–10 min for each vertebra if segmental registrations of each spinal levels were attempted (6).
Table 1
| Intraoperative registration | C4 | C5 |
|---|---|---|
| Registration workflow time | 64 s | 48 s |
| Registration processing time | 1.73 s | 4.82 s |
| Number of points used for registration | 710 | 722 |
| Calculated registration error, mm | 0.3259 | 0.3111 |
Immediate post-operative CT scans were taken to ensure accurate placement of the pedicle screws in the C4 and C5 vertebrae (Figure 3). At the three-month follow-up, imaging results revealed that good hardware placement and alignment were maintained, and the fracture was healing well (Figure 4).
Over the past few decades, computer-assisted navigation for spinal indications have become more widespread, with computer-assisted navigation procedures demonstrating greater accuracy and precision. The benefits of navigation in spine surgery have been shown in multiple research studies, as seen in Table 2. In a study by Rajasekaran et al. (11), which compared non-navigated versus navigated screw insertion in the thoracic spine, the non-navigation group had 54 (23%) pedicle breaches compared to only 5 (2%) in the C-arm based navigation group. Another study by Barsa et al. (12) found that of 295 screws inserted throughout C0 to S1 using intraoperative CT-based spinal navigation, only 4 (1.3%) pedicle screws were incorrectly inserted. Lastly, Shin et al. (13) compared the perforation risk for computer-navigated versus freehand insertion in all spinal regions and found the risk of pedicle perforation in navigated screw insertion to be 6% whereas non-navigated insertion was 15%.
Table 2
| Authors | No. of patients | Primary objective | Principal findings |
|---|---|---|---|
| Navigation improves accuracy at all levels of the spine | |||
| Rajasekaran et al., 2007 (11) | 27 | To compare the accuracy of pedicle screw fixation in thoracic spine deformities correction surgery between a non-navigation group and a group where C-arm based navigation was used | C-arm navigation was able to increase accuracy while reducing total time of surgery |
| Barsa et al., 2014 (12) | 50 | To investigate the accuracy, intraoperative complications and accessibility of CT-based computer-assisted spinal navigation | CT-based computer-assisted spinal navigation has higher accuracy in screw insertion, therefore it has the possibility of lowering surgical complications as well as lowering the total time of surgery |
| Shin et al., 2012 (13) | 8,539 screws | To compare the accuracy of computer-navigated to non-navigated techniques in the insertion of pedicle screws in published literature | For all spinal regions, navigated screw insertion had a significantly lower risk of pedicle perforation as compared with non-navigated insertion |
| Navigation improves accuracy specifically for subaxial cervical instrumentation | |||
| Kotani et al., 2003 (14) | 17 | To compare accuracy, surgical outcomes and complication rates in a group that used computer assistance to insert a screw and a group that used manual insertion to insert a screw | Cervical pedicle screw insertion with computer-assistance was safer and more accurate when compared to the manual technique of screw insertion |
| Ishikawa et al., 2011 (15) | 21 | To evaluate the use of an intraoperative, full-rotation, 3D image (O-arm)-based navigation system in terms of reliability and accuracy when placing a cervical pedicle screw | The use of the O-arm offered high-quality navigation with high-resolution images helping with the accurate and safe insertion of cervical pedicle screws |
| Bredow et al., 2015 (16) | 64 | To examine 3D fluoroscopy navigation in its accuracy of pedicle screw insertion | 3D-fluoroscopy-based navigation systems allow for the accurate insertion of axial and subaxial screws |
| Navigation can reduce operating room personnel radiation | |||
| Bilhar et al., 2018 (17) | 8 | To determine whether fluoroscopic guidance or computer-assisted navigation methods is more accurate in the insertion of pedicle screws into the thoracic spine | The accuracy of both techniques were shown to be equal. Computer-assisted navigation had the added benefit of not using radiation which improves safety of operating room personnel |
| Smith et al., 2008 (18) | 4 | To compare the risk of radiation exposure to the operative surgeon when inserting pedicle screw-rod constructs using C-arm fluoroscopy versus computer-assisted image guidance | When the operative surgeon used computer-assisted image guidance there was a significantly lower exposure to ionizing radiation to the torso as opposed to when the C-arm was used for the same procedure |
| Navigation can be cost efficient | |||
| Dea et al., 2016 (19) | 502 | To determine whether computer-assisted surgery has economic advantages as compared to fluoroscopy | Computer-assisted surgery was shown to reduce the need for reoperations as compared with the group which used fluoroscopy. This means that it has the potential to be cost-efficient |
| Al-Khouja et al., 2015 (20) | 13 studies | To analyse whether there are any economic benefits to using image-guided surgery and navigation in spine surgery | Despite some studies showing lower costs associated with intra-operative imaging, there is still a need for further investigation into the added economic benefits of using these techniques |
Navigation has also shown to specifically improve the accuracy for subaxial cervical instrumentation. A controlled trial by Kotani et al. (14) compared patients undergoing computer-assisted navigation cervical pedicle screw insertion with a control group which underwent manual cervical pedicle screw insertion. Compared to the control group, the computer-assisted navigation group had a lower rate of pedicle wall perforation, and screw trajectory in the horizontal plane was considerably closer to the anatomical pedicle axis. Another study by Ishikawa et al. (15) found that of 108 cervical pedicle screws placed using an intraoperative, full-rotation, 3D image (O-arm)-based navigation system, there were minor pedicle violations in 8.3% of cases and major pedicle violations in 2.8% of cases. They concluded that 3D image-based navigation may be more accurate and reliable if used with other techniques. Lastly, a study by Bredow et al. (16), found that in 64 patients undergoing screw implantation using 3D-fluoroscopy-based navigation, 93.9% of the screws implanted at C1 or C2 and 78.51% of the screws implanted at C3-7 showed placement accuracy grade 2 or better according to the modified Gertzbein and Robbins classification.
Another benefit of using image-guided navigation is that it can reduce operating room personnel radiation exposure. A study by Bilhar et al. (17) found that the accuracy of pedicle screw insertion into the thoracic spine using fluoroscopic guidance relative to computer-assisted navigation techniques was equal and consistent; however, the advantage of using the computer-assisted navigation technique versus fluoroscopic guidance is that the surgical team is not exposed to radiation. Smith et al. (18) found that when performing lumbar pedicle screw placement, the mean radiation to the torso of the surgeon was 4.33±2.66 millirem when using standard fluoroscopy compared to 0.33±0.82 millirem when using computer-assisted image-guidance. The higher radiation by using standard fluoroscopy came with no increased accuracy as both techniques had equal accuracy of screw placement.
Several barriers exist before navigation can be implemented in spinal surgery. A major barrier is the cost of the navigation systems. Despite the high initial costs of navigation, evidence exists that navigation can have long-term cost-efficiency. A study by Dea et al. (19) found a 95.2% accuracy rate for a treatment group that used computer assistance and an 86.9% accuracy for a control group that used conventional fluoroscopy. Within one year following surgery, two patients from the treatment group underwent revision surgery whereas 15 patients from the control group underwent revision surgery. The high cost of computer-assisted technologies can be counterbalanced by the overall reduction in revision surgeries necessary. A literature review by Al-Khouja et al. (20) found that the cost for revision surgery was between $17,650 and $39,643. This cost could be reduced if the need for revision surgery diminishes with the use of image-guidance systems. While there is promising data, an insufficient amount of studies reporting on the economics of spinal navigation currently exists to accurately conclude on its cost-effectiveness in clinical practice.
Conclusions
The benefits of using computer-assisted navigation while inserting pedicle screws into the spine has been widely reported. Not only does computer-assisted navigation reduce screw misplacement rates, it has also been proven to improve accuracy and precision, and also contributes to a significant reduction in revision surgeries following spinal procedures. As demonstrated through this case report, the use of machine vision spinal navigation was able to provide accurate and precise placement of pedicle screws without significantly increasing surgical time. In the case of cervical pedicle screws, precision in screw insertion is of particular importance since cervical pedicles are small, and pedicle screws are an alternative option for fixation when lateral masses are fractured. Cervical pedicle screws can lead to a shorter segment fusion as demonstrated in this case report, which unlike lateral mass screws, also provides fixation to support the anterior, middle and posterior columns of the spine. Computer-assisted navigation has the potential to allow for the safe and accurate insertion of cervical pedicle screws and to reduce the rate of pedicle breach which could avoid significant neurovascular injury.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/acr-21-62
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/acr-21-62). VXDY is a co-founder of 7D Surgical Inc., the manufacturer of the spinal navigation machine used in this study. There are no financial or other conflicts of interest arising from this role. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abumi K, Itoh H, Taneichi H, et al. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 1994;7:19-28. [Crossref] [PubMed]
- Kast E, Mohr K, Richter HP, et al. Complications of transpedicular screw fixation in the cervical spine. Eur Spine J 2006;15:327-34. [Crossref] [PubMed]
- Rajaee SS, Bae HW, Kanim LE, et al. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67-76. [Crossref] [PubMed]
- Ryken TC, Owen BD, Christensen GE, et al. Image-based drill templates for cervical pedicle screw placement. J Neurosurg Spine 2009;10:21-6. [Crossref] [PubMed]
- Jakubovic R, Guha D, Gupta S, et al. High Speed, High Density Intraoperative 3D Optical Topographical Imaging with Efficient Registration to MRI and CT for Craniospinal Surgical Navigation. Sci Rep 2018;8:14894. [Crossref] [PubMed]
- Malham GM, Wells-Quinn T. What should my hospital buy next?-Guidelines for the acquisition and application of imaging, navigation, and robotics for spine surgery. J Spine Surg 2019;5:155-65. [Crossref] [PubMed]
- Gagnier JJ, Kienle G, Altman DG, et al. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. Glob Adv Health Med 2013;2:38-43. [Crossref] [PubMed]
- Ito Z, Higashino K, Kato S, et al. Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: a biomechanical study on strength of fixation. J Spinal Disord Tech 2014;27:80-5. [Crossref] [PubMed]
- Johnston TL, Karaikovic EE, Lautenschlager EP, et al. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J 2006;6:667-72. [Crossref] [PubMed]
- Reinhold M, Bach C, Audigé L, et al. Comparison of two novel fluoroscopy-based stereotactic methods for cervical pedicle screw placement and review of the literature. Eur Spine J 2008;17:564-75. [Crossref] [PubMed]
- Rajasekaran S, Vidyadhara S, Ramesh P, et al. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 2007;32:E56-64. [Crossref] [PubMed]
- Barsa P, Fröhlich R, Sebek F, et al. Intraoperative CT-based spinal navigation: the initial 295 implants experience. Rozhl Chir 2014;93:16-20. [PubMed]
- Shin BJ, James AR, Njoku IU, et al. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 2012;17:113-22. [Crossref] [PubMed]
- Kotani Y, Abumi K, Ito M, et al. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 2003;99:257-63. [PubMed]
- Ishikawa Y, Kanemura T, Yoshida G, et al. Intraoperative, full-rotation, three-dimensional image (O-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine 2011;15:472-8. [Crossref] [PubMed]
- Bredow J, Oppermann J, Kraus B, et al. The accuracy of 3D fluoroscopy-navigated screw insertion in the upper and subaxial cervical spine. Eur Spine J 2015;24:2967-76. [Crossref] [PubMed]
- Bilhar RPO, de Lima DA, Leite JAD, et al. Accuracy of Pedicle Screw Insertion: A Comparison Between Fluoroscopic Guidance and Navigation Techniques. Acta Ortop Bras 2018;26:397-400. [Crossref] [PubMed]
- Smith HE, Welsch MD, Sasso RC, et al. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med 2008;31:532-7. [Crossref] [PubMed]
- Dea N, Fisher CG, Batke J, et al. Economic evaluation comparing intraoperative cone beam CT-based navigation and conventional fluoroscopy for the placement of spinal pedicle screws: a patient-level data cost-effectiveness analysis. Spine J 2016;16:23-31. [Crossref] [PubMed]
- Al-Khouja L, Shweikeh F, Pashman R, et al. Economics of image guidance and navigation in spine surgery. Surg Neurol Int 2015;6:S323-6. [Crossref] [PubMed]
Cite this article as: Yeretsian T, Lai C, Guha D, Ramjist J, Yang VXD. Machine-vision image guided C4-C5 unilateral cervical pedicle screw insertion: case report and review of literature. AME Case Rep 2022;6:9.


