
Endoscopic decompression of L3 nerve root in a case of adult spinal deformity correction with post-operative neurological deficit: a case report
Introduction
Adult spinal deformities (ASD) have as high as 23 percent incidence of postoperative neurological decline (1). The post-surgery neurological deficit can be addressed in multiple ways which vary from conservative expectant management to immediate surgical exploration depending upon various clinical scenarios. However, undergoing an extensive exploratory surgery again can be a very hard decision for the patient to make. As the advantages as well as safety of endoscopic spine surgery (ESS) have been established, spine surgeons all over the world are extending the boundaries of ESS with similar or better outcomes to other conventional/traditional minimally invasive spine surgeries (MISS) (2). In this report we present a case of L3 radiculopathy post deformity correction surgery and its management with endoscopic decompression surgery.
We present the following case in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/acr-21-58).
Case presentation
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
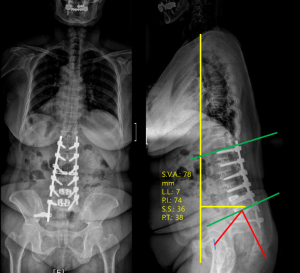
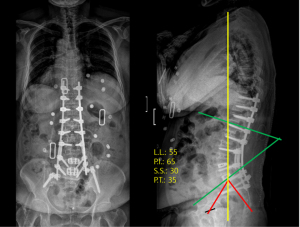
A 78-year-old female patient presented with backache, buttock pain and right-side dominant radiating leg pain. Radiographs revealed distal junctional failure with left rod fracture between L5-S1 and screw loosening (Figure 1). Her radiographs showed a gross sagittal imbalance with C7-sagittal vertical axis (SVA) of 78 mm, pelvic incidence (PI) of 74°, lumbar lordosis (LL) of 15° and pelvic tilt (PT) of 38°. This meant that her PI-LL value was 59°, which should ideally be ≤10° (3). She was thus treated with L4 pedicle subtraction osteotomy (PSO) with T10 to iliac posterior fixation with the use of multiple rod construct with satellite rods at the PSO site (Figure 2).
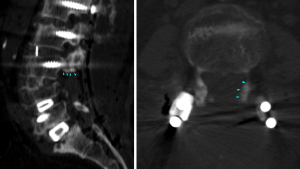
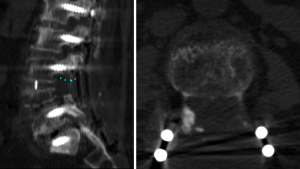
Soon after the surgery the patient complained of weakness (Grade 2 power) in knee extension on left side. On careful radiological evaluation, the CT scan and MRI revealed that the left sided L3 nerve root was being compressed by a bone fragment (Figure 3). A decision was made to perform decompression the L3 nerve root at the earliest since an urgent treatment of neurologic complications is very important when helping patients recover from neurological deficits after lumbar spine surgeries (4). As the patient was an old lady who had just undergone a major spine surgery, we decided to perform endoscopic spine surgery under the awake anaesthesia (5-7).
The diagnostic injection in this case could have been used to re-confirm the diagnosis. However, since the cause of deficit was radiologically visible as root compression by the surrounding bone spur, an additional intervention of a diagnostic block was not considered. Instead getting rid of the compressing structure was given preference.
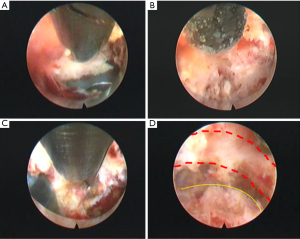
Patient was given prone position with both hips and knees flexed. After infiltrating the skin with local anaesthesia, an 18-G spinal needle was used under fluoroscopic guidance to target the left L2-L3 interlaminar window. A blunt guidewire was introduced through the needle and the needle was removed. A 1-cm incision was taken, followed by serial dilatation and finally insertion of endoscopic working canula of 11.5 mm diameter. This was followed by insertion of rigid endoscope (iLLESYS delta, Joimax GmbH, Germany) with 1cm outer diameter and 6 mm working channel. Radiofrequency probe was used to achieve haemostasis and endoscopic laser and graspers were used to remove soft tissues. An endoscopic high-speed drill was used to remove the bone at the base of L3 pedicular screw which was compressing on L3 nerve root (Figure 4).
Post-operatively, the patient had rapid relief of the radicular pain with improvement in the left quadriceps (L3) power and was discharged. The post operative CT scan showed removal of the compressing bony part (Figure 5). The patient has completed 1-year follow up and remains symptom free with good sagittal spinal alignment (Figure 6).

Discussion
ASD correction by 3CO (three-column osteotomy, either PSO or vertebral column resection) is a powerful tool to achieve significant correction of spinal alignment but has a high complication rate. A multicentric-study of 82 ASD cases treated with 3CO, found that rod fracture (31.7%) was the most common complication followed by dural tear, new-onset neurological deficit and proximal junctional kyphosis (9.8% each) (8). Overall, 78% patients had at least 1 complication with 61% patients having at least 1 major complication.
Addition of supplementary rods reduces the chances of hardware failure and thus should be used while correcting ASD with 3CO. When compared amongst the additional rod constructs, accessory-rods (connected to primary rods) have more failures than the satellite-rods (independently anchored in the pedicles) (9). Thus, we used 4-rod construct with satellite-rods for augmenting the L4-PSO fixation. We believe, since the L3 pedicular screw had to be inserted deeper than the other screws to accommodate the satellite-rod, the bone in the area near the screw head (part of either the pedicle or facet) caused compression of the left L3 nerve root.
There are a few reports on ESS being used for treating post-operative complications after spine surgeries. Wagner et al. reported the use of ESS in treating post-operative S1-radiculopathy developed due to protruding screw passed during minimally invasive sacroiliac joint fusion. In their case, the tip of the Sacroiliac joint fusion implant was impinging upon the S1 nerve root which was decompressed by drilling out the protruding part of the screw endoscopically (10). Another report describes a case of post-operative right L2 radiculopathy in a 72-year-old patient after undergoing kyphoplasty (11). On CT scan, cement leak was found on the superomedial aspect of right L2 pedicle which was removed endoscopically. McGrath et al. used ESS in the patients treated with lumbar spinal fusions who developed unilateral radiculopathies. The causes were foraminal stenosis at adjacent segment in 7 patients, at arthrodesis segment in 3 patients, and stenosis caused by displacement of the interbody cage in 1 patient. They reported successful outcomes in all the 11 patients with no complications (12).
Our case is the first reported complication related with satellite rod construct which was treated by ESS. This report assumes more importance in the sense that the scope of ESS nowadays is not just limited to MISS. This technique can very well be used to treat complications caused after traditional open surgeries and can prevent an open revision surgery. ESS results in minimal blood loss, avoids general anaesthesia and hence very useful especially for old age patients with high risk of anaesthesia (5). The important advantage of having an awake and aware patient during surgery is that the surgeon can determine the end point/adequacy of decompression as per the feedback from the patient. This also prevents the surgeon from causing iatrogenic neurological injury. The patient who is fully aware communicates with the surgeon when surgeon works near the nerve roots or manipulates the nerve roots. To determine if a patient will be benefited from ESS, the decision is made based on whether the same surgical goals as open surgery can be achieved while reducing the invasiveness of the procedure (6). The use of ESS in our case could prevent an extensive open revision surgery in a patient who had already been subjected to various spine surgeries.
All the complications of ASD surgery however, cannot be managed endoscopically. There are instances where the alignment of the rods needs to change, in some cases the trajectory of the pedicle screw needs to be changed. In such cases the open revision surgery is unavoidable. Thus, the indications for ESS need to be tailor made for each patient, based mainly on the cause of the deficit and whether it is amenable to endoscopic spine surgery. Presence of localised compressing mass or hematoma, treatment of herniated discs/degeneration at the adjacent levels are good candidates for ESS.
As the techniques such as satellite rod construct become more popular, in future there can be more such cases of the nerve root irritation due to the screw head/bone fragment compressing the nerve root. We believe, this report will be helpful to all those clinicians, who may encounter a similar post-operative neurological complication after the use of multiple rod constructs.
Thus, to conclude, the advances in endoscopic spine surgery techniques have opened a new avenue in the treatment of complications of spine surgery in a minimally invasive manner. We could successfully treat a case of iatrogenic left-sided L3-radiculopathy, with endoscopic spine surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/acr-21-58
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/acr-21-58). JB and SHL are consultants with Joimax GmbH. AHS has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fehlings MG, Kato S, Lenke LG, et al. Incidence and risk factors of postoperative neurologic decline after complex adult spinal deformity surgery: results of the Scoli-RISK-1 study. Spine J 2018;18:1733-40. [Crossref] [PubMed]
- Chung AS, Wang JC. The rationale for endoscopic spinal surgery. Neurospine 2020;17:S9-12. [Crossref] [PubMed]
- Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38:E803-12. [Crossref] [PubMed]
- Wang R, Li C, Yi X, et al. Causes of lower extremity weaknesses after posterior lumbar spine fusion surgery and therapeutic effects of active surgical exploration. J Orthop Surg Res 2020;15:435. [Crossref] [PubMed]
- Butler AJ, Alam M, Wiley K, et al. Endoscopic Lumbar Surgery: The State of the Art in 2019. Neurospine 2019;16:15-23. [Crossref] [PubMed]
- Hasan S, Härtl R, Hofstetter CP. The benefit zone of full-endoscopic spine surgery. J Spine Surg 2019;5:S41-56. [Crossref] [PubMed]
- Kambin P. Diagnostic and therapeutic spinal arthroscopy. Neurosurg Clin N Am 1996;7:65-76. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Klineberg E, et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 2017;27:444-57. [Crossref] [PubMed]
- Gupta M, Henry JK, Schwab F, et. al. Reducing Rod Breakage and Pseudarthrosis in Pedicle Subtraction Osteotomy: The Importance of Rod Number and Configuration in 264 patients with 2-Year Follow-Up. Glob Spine J 2016;6:s-0036-1582911-s-0036-1582911.
- Wagner R, Telfeian AE, Krzok G, et al. Endoscopic Surgical Technique for Treating Sacral Radiculopathy Secondary to S1 Nerve Compression After Minimally Invasive Sacroiliac Joint Fusion: Technical Note. World Neurosurg 2018;119:349-352. [Crossref] [PubMed]
- Wagner R, Telfeian AE, Iprenburg M, et al. Transforaminal Endoscopic Solution to a Kyphoplasty Complication: Technical Note. World Neurosurg 2016;91:195-8. [Crossref] [PubMed]
- McGrath LB Jr, Madhavan K, Chieng LO, et al. Early experience with endoscopic revision of lumbar spinal fusions. Neurosurg Focus 2016;40:E10. [Crossref] [PubMed]
Cite this article as: Bae J, Sathe AH, Lee SH. Endoscopic decompression of L3 nerve root in a case of adult spinal deformity correction with post-operative neurological deficit: a case report. AME Case Rep 2022;6:1.


