
Minimally invasive robotic cervicothoracic fusion: a case report and review of literature
Introduction
Minimally invasive surgery (MIS) of the posterior cervicothoracic spine has recently emerged to treat cervical myelopathy and radiculopathy through spinal fusion. Implementation of 3D neuronavigation and robotic assistance have made smaller incisions possible while also reducing muscular injury, which has decreased postoperative pain and recovery time compared to traditional open techniques (1-4). MIS techniques also significantly reduce intraoperative blood loss while open techniques result in significant blood loss and lengthy recovery times (2,3,5-9).
Robotic-assisted fixation techniques further reduce blood loss and increase pedicle screw insertion accuracy compared to MIS techniques alone (10,11). The first reported case of posterior upper cervical spine surgery using robotic assistance was performed by Tian, where a C1–2 transarticular screw fixation was safely performed under guidance of the TiRobot with accuracy and without complications (10). Another study by Fan et al. further demonstrated accurate cervical screw placement and reduced blood loss using robotic assistance (11).
We report a case of a male patient who presented with progressive right hand and forearm weakness with corresponding atrophy. Spinal canal stenosis, cord compression, foraminal stenosis, and a right paracentral disc herniation was discovered upon magnetic resonance imaging (MRI). A MIS percutaneous robotic cervicothoracic fusion was performed, and it successfully recovered right hand and forearm strength without residual sensory loss. We discuss the findings of our novel technical description and also provide a narrative review of the current literature to identify previous cases which successfully used a MIS cervicothoracic technique.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-149).
Case presentation
History and presentation
A 68-year-old male presented with 6 months of progressive right hand and forearm weakness. His hand was caught in a claw-like position with atrophy of the thenar eminence and forearm. A neurological examination demonstrated decreased strength in the right upper extremity graded as 2/5 for the interossei, opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis. The patient had no clinical signs of myelopathy. A cervical MRI at presentation showed foraminal stenosis at C7–T1 and a right-sided disc herniation with foraminal impingement at T1–T2 (Figure 1).The risks of the procedure and alternatives were discussed, and surgery was determined to be the best course of treatment to minimize further functional loss and maximize his chances of recovering strength.

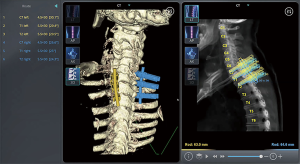
Robotic software planning
Preoperative planning software was utilized to pre-plan trajectories for all screws to allow for directed intraoperative rod placement and to ensure anatomical placement of all instrumentation (Figure 2).
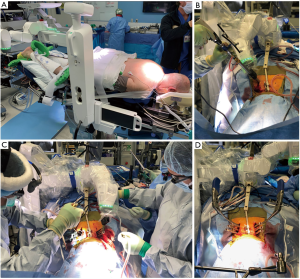
Intraoperative positioning and robotic platform attachment
The patient was positioned prone. Two small stab incisions were made over the C7 and T1 spinous processes and two spinous process pins were placed under fluoroscopic guidance. This was then attached to the navigated spinal robotics platform. Once this was completed, the navigated spinal robotic platform was then registered to the patient with a series of X-rays and an optical survey scan.
Intraoperative robotic technique
A right-sided paraspinal incision was made with the guidance of the robotics platform and the right then left-sided C7, T1 and T2 pedicle tracts were then drilled and tapped. A minimal access retractor was then placed for exposure of the right sided C7–T2 facets. A full C7–T1 and T1–2 facetectomy was performed with full visualization of the exiting C8 and T1 nerve root from its origin at the level of the dura out to the foramen, followed by a T1–T2 discectomy. Bone graft was laid, and rods were then secured bilaterally (Figure 3).
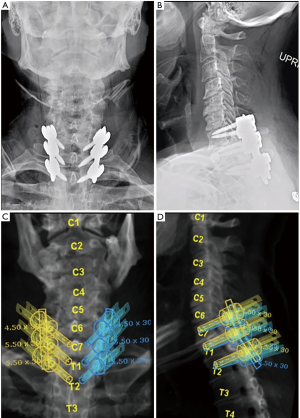
Outcome
There was immediate postoperative improvement in the patient’s upper extremity strength and postoperative imaging confirmed accurate hardware placement. The patient was discharged without complications. At 6 months follow-up there was improvement in hand grip strength to a 4–/5 with sensation intact throughout (Figure 4). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Discussion
A review of the English-language literature using the PubMed database for published case reports and case series from earliest date until present demonstrated 18 reports ranging in publication year between 2005 to 2019, that described patients who underwent percutaneous or MIS posterior cervicothoracic fixation between C1–T4 (Table 1). There was a total of 217 patients (range 16–89 years old, 119 men and 98 women) in reports where this information was available who underwent MIS surgery to correct the conditions including but not limited to cervical fractures, tumors, and discopathy (Table 1) (1-9,12-19). Surgical techniques included pedicle screw or lateral mass fixation (17-19), stand-alone screw fixation (2), transpedicular osteosynthesis (6), gallie fusion (8), and DTRAX facet implant (5). Average operation times were reduced compared to open techniques and ranged from 90 to 298 minutes when reported (2,20). A majority of cases reported pain reduction compared to open techniques. Complications included postoperative quadriplegia from epidural hematoma (20), clinically significant pedicle screw deviation/backout (5,13), conversion to open surgery (18), and postoperative infection (15,18).
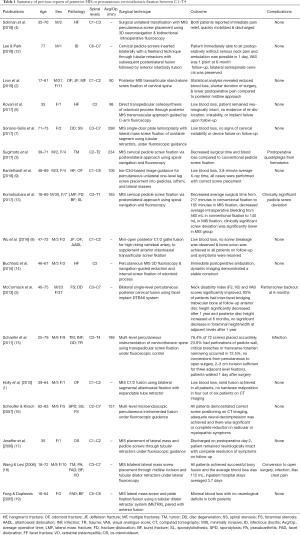
Full table
Shift towards MIS cervical spine surgery
Cervical MIS techniques reduce tissue trauma, blood loss, infection rate, and operative time without compromising accuracy or stability of fixation compared to traditional techniques (2,6,20). Decreased postoperative pain following MIS surgery in comparison to traditional open techniques can be attributed to the reduced surgical stress of muscle stripping and retraction accomplished through use of small MIS exposures and access through tubular retractors (1,13,20). Minimally invasive approaches also allow earlier ambulation and discharge (4,14), which may ultimately lead to decreased cost and complications.
Robotic MIS
Recent advances in technology and technique strive to improve stability, accuracy, and consistency during pedicle screw placement. These can be accomplished during MIS approaches with use of surgical planning, preoperative imaging, and real-time neuronavigation techniques to avoid screw malposition and potential injury to vertebral arteries or nerve roots (13,20). Robotic assistance further increases the capabilities of MIS by using computer-assisted navigation that incorporates cameras, imaging, robotic arms, and tracking of patients/robotic arms (10,11). Although open exposures have the advantage of a larger visual field and ease of rod placement, the need for direct visualization is reduced as the navigated robotic arm allows screw trajectory to be confirmed with overlayed preoperative imaging that contains pre-planned targets, and the arm maintains a stable and rigid tubular retractor position as to avoid deviation during screw placement. As demonstrated in the preoperative plan, spinal robotics allows for planning of the entirety of a construct with insertion points and trajectories, rather than individual screws that are then rodded together. This makes rod passage more feasible through a smaller incision in comparison to traditional MIS techniques, which speeds up workflow resulting in reduced overall operative time.
Robotic assistance for spinal fixation has already been established as a safe technique in lower spine surgeries (10,11). A recent prospective randomized control study comparing fluoroscopy-assisted versus robot-assisted cervical screw fixation was performed by Fan et al. (11). They found that patients with robot-assisted fixation had significantly better screw placement accuracy, and the robot-assisted group experienced significantly less blood loss and shorter post-operative lengths of stay (11). Despite the benefits of robotic assistance, difficulties with registration/trajectory and anatomical variations that are undetected through preoperative imaging could lead to complications (10,11). We used a Maxor X system and did not encounter any issues with registration which allowed successful completion of this minimally invasive fusion without any technical shortcomings or complications. Adoption of robotic assistance in posterior cervicothoracic fusion is still in its early stages so further studies are required to determine its efficacy.
Conclusions
MIS robotic posterior cervicothoracic fusion can effectively be used to achieve surgical decompression and instrumentation resulting in reduced blood loss and shorter post-operative length of stay. We report here an operative technical description and review of the literature which demonstrates these characteristics while also highlighting areas for future improvement. Further implementation of robotic assistance in larger studies is needed to further evaluate its effectiveness.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-149
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-149). Dr. MHP reports personal fees from Medtronic as a consultant, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holly LT, Isaacs RE, Frempong-Boadu AK. Minimally invasive atlantoaxial fusion. Neurosurgery 2010;66:193-7. [Crossref] [PubMed]
- Lvov I, Grin A, Kordonskiy A, et al. Minimally invasive posterior transarticular stand-alone screw instrumentation of C1-C2 using a transmuscular approach: description of technique, results and comparison with posterior midline exposure. World Neurosurg 2019;128:e796-805. [Crossref] [PubMed]
- Sugimoto Y, Hayashi T, Tokioka T. Minimally invasive cervical pedicle screw fixation via the posterolateral approach for metastatic cervical spinal tumors. Spine Surg Relat Res 2017;1:218-21. [Crossref] [PubMed]
- Soliman MAR, Kwan BYM, Jhawar BS. Minimally invasive unilateral percutaneous transfracture fixation of a hangman's fracture using neuronavigation and intraoperative fluoroscopy. World Neurosurg 2019;122:90-5. [Crossref] [PubMed]
- McCormack BM, Bundoc RC, Ver MR, et al. Percutaneous posterior cervical fusion with the DTRAX Facet System for single-level radiculopathy: results in 60 patients. J Neurosurg Spine 2013;18:245-54. [Crossref] [PubMed]
- Kovari VZ, Josvai A, Csokay A. Transpedicular direct osteosynthesis of hangman's fracture from a mini-open exposure as a less invasive procedure: a technical note. Trauma Case Rep 2017;12:66-71. [Crossref] [PubMed]
- Soriano-Solís S, Quillo-Olvera J, Rodríguez-García M, et al. Minimally invasive single-door plate laminoplasty with lateral mass screw fixation for the unstable segment. report of two cases with long follow-up. Coluna/Columna 2017;16:236-9. [Crossref]
- Wu AM, Wang XY, Zhou F, et al. Percutaneous atlantoaxial anterior transarticular screw fixation combined with mini-open posterior C1/2 wire fusion for patients with a high-riding vertebral artery. J Spinal Cord Med 2016;39:234-9. [Crossref] [PubMed]
- Kantelhardt SR, Keric N, Conrad J, et al. Minimally invasive instrumentation of uncomplicated cervical fractures. Eur Spine J 2016;25:127-33. [Crossref] [PubMed]
- Tian W. Robot-assisted posterior C1-2 transarticular screw fixation for atlantoaxial instability: a case report. Spine (Phila Pa 1976) 2016;41:B2-5. [Crossref] [PubMed]
- Fan M, Liu Y, He D, et al. Improved accuracy of cervical spinal surgery with robot-assisted screw insertion: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2020;45:285-91. [Crossref] [PubMed]
- Lee S, Park JH. Minimally invasive cervical pedicle screw placement with a freehand technique through the posterolateral approach using a tubular retractor: a technical note. Oper Neurosurg (Hagerstown) 2019;17:E166-72. [Crossref] [PubMed]
- Komatsubara T, Tokioka T, Sugimoto Y, et al. Minimally invasive cervical pedicle screw fixation by a posterolateral approach for acute cervical injury. Clin Spine Surg 2017;30:466-9. [Crossref] [PubMed]
- Buchholz AL, Morgan SL, Robinson LC, et al. Minimally invasive percutaneous screw fixation of traumatic spondylolisthesis of the axis. J Neurosurg Spine 2015;22:459-65. [Crossref] [PubMed]
- Schaefer C, Begemann P, Fuhrhop I, et al. Percutaneous instrumentation of the cervical and cervico-thoracic spine using pedicle screws: preliminary clinical results and analysis of accuracy. Eur Spine J 2011;20:977-85. [Crossref] [PubMed]
- Scheufler KM, Kirsch E. Percutaneous multilevel decompressive laminectomy, foraminotomy, and instrumented fusion for cervical spondylotic radiculopathy and myelopathy: assessment of feasibility and surgical technique. J Neurosurg Spine 2007;7:514-20. [Crossref] [PubMed]
- Joseffer SS, Post N, Cooper PR, et al. Minimally invasive atlantoaxial fixation with a polyaxial screw-rod construct: technical case report. Neurosurgery 2006;58:ONS-E375; discussion ONS-E375.
- Wang MY, Levi AD. Minimally invasive lateral mass screw fixation in the cervical spine: initial clinical experience with long-term follow-up. Neurosurgery 2006;58:907-12; discussion 907-12. [Crossref] [PubMed]
- Fong S, Duplessis S. Minimally invasive lateral mass plating in the treatment of posterior cervical trauma: surgical technique. J Spinal Disord Tech 2005;18:224-8. [Crossref] [PubMed]
- Mikhael MM, Wolf CF, Shamie AN, et al. Minimally invasive techniques for the posterior cervical spine: foraminal decompression and instrumented fusion. Oper Tech Orthop 2011;21:240-4. [Crossref]
Cite this article as: Diaz-Aguilar LD, Hassan O, Pham MH. Minimally invasive robotic cervicothoracic fusion: a case report and review of literature. AME Case Rep 2021;5:24.


