
Colon metastasis from recurrent gallbladder cancer: a case report
Introduction
Primary adenocarcinoma of the gallbladder accounts for 5% of malignant tumors and is associated with a poor prognosis. It is diagnosed as an incidental finding while doing abdominal procedures for other diseases or cholecystectomy (1-3). Gallstones are the most prevalent risk factors and are present in 70–90% of patients with gallbladder cancer (GBC) (4). Some correlations between tobacco use, female sex, multiparity, substance abuse, high body mass index (BMI) and incidence of gallbladder carcinoma were found. In the most of cases, patients are asymptomatic (5-7). The majority of symptoms include pain, anorexia, nausea or vomiting, obstructive jaundice, either from direct invasion of the biliary tree or from metastatic liver diseases. The most frequent sites of metastases from this kind of neoplasm are intraabdominal and among them, we list the liver most frequently involved by direct extension, with an incidence ranging from 60% to 90% and intra-abdominal lymph nodes involved in about 60% of cases (8). Extra-abdominal metastatic sites like pleura and lung are rare. Very few cases are reported affecting skin, bone, central nervous system, heart, orbit, scalp, cervix, kidney, thyroid, breast and even the hernia sac (9-18). Approximately 10–30% of patients will be candidates for surgical resection, the only potentially curable treatment of localized gallbladder carcinoma. Adjuvant therapy options are about fluoropyrimidine-based chemoradiation or fluoropyrimidine- or gemcitabine-based chemotherapy alone. Chemotherapy is the mainstay for stage IV/unresectable GBC even if prognosis is poor despite treatment. Targeted biologic therapy, such as inhibitors of VEGF, EGFR, and HER2, have been evaluated in the setting of advanced disease but further studies are still needed in this issue (19). Colonic metastases representing approximately 1% of total colorectal cancers, are very rarely reported; in most cases there are multiple lesions and one third of them may still be asymptomatic or found only at autopsy. Metastatic involvement of colorectum is often diagnosed in patients with a primary cancer deriving from the lung, ovary, breast, prostate, kidney, skin, stomach, or hepatobiliary system (20). Herein, we present a case of recurrent gallbladder cancer with synchronous liver and colonic metastases. To date, based on patient data in the literature, there have been no reports about development of metastases to the colon from primary gallbladder adenocarcinoma.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-167).
Case presentation
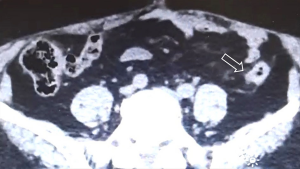
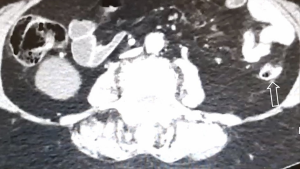
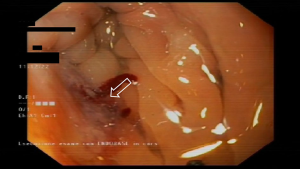
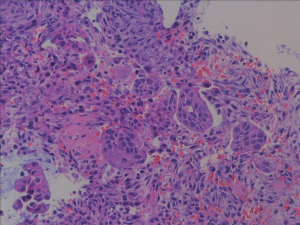
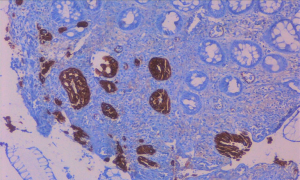
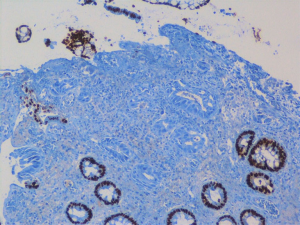
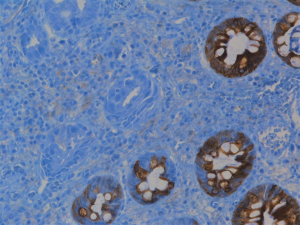
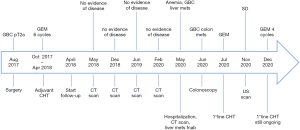
A 78-year-old woman’s past medical history was marked, 3 years ago, by a cholecystectomy for a diffuse carcinoma in situ and an infiltrating adenocarcinoma pT2a G2; she completed six months of adjuvant gemcitabine chemotherapy and started a regular follow up in our institution. According to the guidelines, a clinical-laboratory-instrumental re-evaluation was carried out every 6 months. In May 2020, because a severe anemia [hemoglobin (hb) 6 g/dL] our patient was hospitalized in Medicine Institute of our Hospital. She underwent blood transfusions and other tests. A CT scan showed liver metastases, the two largest of which were in the VIII segment, respectively in the subcapsular region (maximum diameter 20 mm) and in the paracaval region (maximum diameter 16 mm), and two focal parietal doubtful circumscribed parietal thickening of the left colon and sigmoid tract (Figures 1,2). A flexible colonoscopy revealed a 3 cm extending stenosis with a fragile and eroded surrounding mucosa difficult to overcome, 30 cm from the anal verge, another similar lesion with a maximum diameter 7 mm at 34 cm from the anal verge and a third 5 cm lesion with ulcerated mucosa and fragile on contact with the instrument, 49 cm from the anal verge. All three lesions were biopsied but histological examination was not diagnostic. Biopsy of one of the liver lesions was then performed: histological examination was compatible with a metastatic localization of gallbladder adenocarcinoma (CK7+, CK20−, CDX2−). Suddenly a second colonoscopy was indicated by a multidisciplinary oncology group. The examination was interrupted due to the difficulty of progression of the instrument in relation to the visceral rigidity at the sigmoid level where an eroded and easily bleeding nodular mucosal area in sigmoid tract with diverticular disease (DICA-3 according to the Diverticular Inflammation and Complication Assessment, an endoscopic classification for diverticulosis and diverticular disease of the colon) was found (Figure 3). The histological examination of the biopsies performed at this level revealed an infiltration of adenocarcinoma, a finding compatible with a metastasis of gallbladder adenocarcinoma (CK7+, CK20−, CDX2−) (Figures 4-7). The case was collegially re-evaluated by a multidisciplinary team. In consideration of the progressive deterioration of the clinical conditions, the extension of the primary GBC and the patient’s age, it was decided not to carry out with the typing of the 49 cm from the anal verge located and not otherwise accessible colon lesion and to start a first-line mono-chemotherapy treatment with gemcitabine undertaken in July 2020. To date, the well-tolerated chemotherapy is still ongoing at our institute and is getting a good disease control (Figure 8).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Discussion
The occurrence of GBC is rare, since the symptoms are similar to those of benign disease. It is estimated that 86–100% of these cancers are associated with cholelithiasis. It is histologically mainly reported after surgical gallbladder resection for benign diseases such as chronic cholecystitis and gallstones. Some researchers suggest that gallbladder stones may form as a result of carcinoma or may indicate a predisposition for malignancies. It appears to have a triple higher prevalence in women than in men with a peak in the seventh decade of life. In our case herein reported, the gallbladder carcinoma was diagnosed following cholecystectomy that was performed for chronic cholecystitis due to gallbladder stones. The most common histological type of GBC is adenocarcinoma. Unfortunately, GBC is still diagnosed at an advanced stage with an unfavorable prognosis and a one-year survival rate of only 10% and so far no treatment is truly effective. Patients with localized disease are estimated to have a five-year survival rate of approximately 32%. According to more recent data in the literature, cases of colon metastasis from gallbladder carcinoma have not been reported (20). Our case is probably the first report of colon metastasis in a patient with recurrent GBC. Therefore, any endoscopically observed suspected colonic lesion in a patient with a known GBC should always be carefully examined using the clinical, radiological and pathological examination in order to catch early metastasis. The case reported here is very unusual in that the patient during the follow-up developed blood loss anemia which made one suspect the presence of a primary colon cancer and not a colon with secondary involvement from another origin. Our case may help us in daily clinical practice, to promote endoscopic screening for intestinal metastases during follow-up for any primary tumor, in patients who present vague and non-specific abdominal signs and symptoms. Our patient developed severe microcytic anemia with heme positive stools for which she was promptly subjected to blood transfusions and instrumental investigations, including colonoscopy, despite not having obstructive disorders. The best knowledge of intestinal metastases from gallbladder carcinoma and their correct management could lead to a longer survival. Metastatic colon lesions are a rare clinical entity that can present management difficulties. The incidence of this type of metastasis seems to increase, following the increased awareness of doctors during the clinical-instrumental follow-up checks of a primary neoplasm. Furthermore, the presence of an increasing percentage of metastatic lesions in an unusual site at the autopsy table, should be a trigger for further investigations for doctors who deal with colorectal oncology. Their clinical presentation can vary from asymptomatic to signs similar to those of colorectal carcinoma as in our patient who at the same time also developed histologically compatible liver metastases as secondary from gallbladder carcinoma. However, immunohistological analysis is indeed the cornerstone to distinguish colon metastases from other tumors from primary colorectal neoplasms. All of this is extremely important to guide the oncologist and identify the best therapeutic strategy with the best treatment options on which survival ratios depend. So our case for the first time helps us to keep in mind that colon metastases can occur in patients with gallbladder adenocarcinomas and may also be the presenting sign. It could be argued that patients with a history of GBC and showing gastrointestinal symptoms, although not specific, should undergo appropriate diagnostic procedures, such as colonoscopy, computed tomography and or magnetic resonance imaging, to exclude any intestinal metastases.
Conclusions
This is probably the first reported case of colonic metastasis in a patient with a recurrent gallbladder carcinoma with synchronous liver involvement. In our opinion, it is important to have great awareness during follow-up examinations for primary neoplasms, so as to prevent secondary involvement to the colon and rectum too. Keeping this in mind we conclude that though colon is a rare metastatic site of GBC and it may be a difficult issue for oncologists to resolve because of its rarity, one should keep vigilance for colon metastases to prevent and detect their occurrence in symptomatic cases in order to improve the survival period.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-167
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-167). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol 2014;6:99-109. [PubMed]
- Rahman R, Simoes EJ, Schmaltz C, et al. Trend analysis and survival of primary gallbladder cancer in the United States: a 1973-2009 population-based study. Cancer Med 2017;6:874-80. [Crossref] [PubMed]
- Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 2006;118:1591-602. [Crossref] [PubMed]
- Hsing AW, Gao YT, Han TQ, et al. Gallstones and the risk of biliary tract cancer: a population-based study in China. Br J Cancer 2007;97:1577-82. [Crossref] [PubMed]
- Rakić M, Patrlj L, Kopljar M, et al. Gallbladder cancer. Hepatobiliary Surg Nutr 2014;3:221-6. [PubMed]
- Misra S, Chaturvedi A, Misra NC, et al. Carcinoma of the gallbladder. Lancet Oncol 2003;4:167-76. [Crossref] [PubMed]
- Pandey M, Shukla VK. Diet and gallbladder cancer: a case-control study. Eur J Cancer Prev 2002;11:365-8. [Crossref] [PubMed]
- Dwivedi AN, Jain S, Dixit R. Gall bladder carcinoma: Aggressive malignancy with protean loco-regional and distant spread. World J Clin Cases 2015;3:231-44. [Crossref] [PubMed]
- Puglisi F, Capuano P, Gentile A, et al. Retrobulbar metastasis from gallbladder carcinoma after laparoscopic cholecystectomy. A case report. Tumori 2005;91:428-31. [Crossref] [PubMed]
- Amarti LE, Faouzi H, Salmi N, et al. Breast metastasis from recurrent gallbladder adenocarcinoma: a case report with review of the literature. J Gastrointest Oncol 2016;7:E77-80. [Crossref] [PubMed]
- Molina-Barea R, Rios-Peregrina RM, Slim M, et al. Lobular breast cancer metastasis to the colon, the appendix and the gallbladder. Breast Care (Basel) 2014;9:428-30. [Crossref] [PubMed]
- Chaudhari S, Hatwal D, Bhat P. A rare presentation of gallbladder carcinoma metastasis. J Clin Diagn Res 2014;8:FD19-20. [Crossref] [PubMed]
- Tanriverdi O, Meydan N, Barutca S, et al. Cutaneous metastasis of gallbladder adenocarcinoma in a patient with chronic lymphocytic leukemia: a case report and review of the literature. Ann Dermatol 2013;25:99-103. [Crossref] [PubMed]
- Kumar S, Singh D, Goel MM, et al. FNAC site metastasis in gall bladder cancer--a rare presentation. BMJ Case Rep 2012;2012:bcr0220125777 [Crossref] [PubMed]
- Jani C, Baiyee E, Jani R. Intramuscular Metastasis of Gallbladder Carcinoma. Arch Cancer Res 2020;8:6.
- Jeyaraj P, Sio TT, Iott MJ. An unusual case of isolated, serial metastases of gallbladder carcinoma involving the chest wall, axilla, breast and lung parenchyma. Rare Tumors 2013;5:e7 [Crossref] [PubMed]
- Swain JR, Tewari M, Shukla HS. Scalp Metastases as a Rare Primary First Manifestation of Gallbladder Cancer. Indian J Surg 2019;81:184-5. [Crossref]
- Siddiqui M, Hegde S, Nguyen T, et al. Sarcomatoid carcinoma of the gallbladder: A rare form of gallbladder cancer. SAGE Open Med Case Rep 2020;8:2050313X20906739.
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Hepatobiliary Cancers. Version 5.2020 – August 4, 2020. NCCN.org.
- Galanopoulos M, Gkeros F, Liatsos C, et al. Secondary metastatic lesions to colon and rectum. Ann Gastroenterol 2018;31:282-7. [Crossref] [PubMed]
Cite this article as: Signorelli C, Marrucci E, Cristi E, Pastorelli A, Cardello P, Chilelli MG, Zampaletta C, Ruggeri EM. Colon metastasis from recurrent gallbladder cancer: a case report. AME Case Rep 2021;5:21.


