
Al Wakra type II myocardial infarction—a case report in our emergency department
Introduction
Myocardial infarction (MI) is one of the serious diseases presented in the emergency department (ED). Hence, all the staff in the ED, doctors, and nurses should be trained in MI diagnosis and treatment. MI has varied presentations including chest pain, chest discomfort, pain in left shoulder, neck pain or silent symptoms as observed in some diabetic patients. In addition, it can be induced by multiple factors such as diabetes mellitus (DM), smoking, hypertension, stress, etc. The fourth universal definition of MI 2018, defined MI as the presence of acute myocardial injury detected by abnormal cardiac biomarkers in the setting evidence of myocardial ischemia. They classified MI into 5 types: (I) ischemic myocardial necrosis because of coronary artery block by thrombus or plaque rupture, (II) ischemic myocardial necrosis resulting due to decreased the blood, oxygen supply and demand mismatch, (III) sudden cardiac death without troponin value, (IV) procedural-related MI, including post percutaneous coronary intervention and stent thrombosis, (V) post coronary artery bypass grafting (1).
Sepsis is the condition can be induce septic shock that the cause of multi-organ dysfunction. Septic shock is the one of causes of demand mismatch in cardiac cell so it’s lead to type II MI (2). There is no direct relation between Fever and MI but some of reviews discussed fever as of sign of endocarditis in MI patient. Also, some of cardiac patient after cardiac procedures had fever (3). Here we discussed triad of fever as sign of sepsis or pre-sepsis condition in case of severe infection, Type II MI and overcrowded problems in ED.
Overcrowded ED is a famous problem in big hospitals with high flow rate. This is causes for delay or negligence in critical cases with poor prognoses due to delayed examination and management. Clinical history may be incomplete in an overcrowded hospital because of time stress. Under such circumstances, triage would be useful in the waiting area as it is a dynamic process for detecting deterioration of any waiting case and accordingly re-prioritizing the case. Moreover, different research and quality improvement projects (QIPs) should be implemented to avoid missing of cases and prevent overcrowding complications (4).
In general, Emergency physician should be aware of fever may be early sign of severe infection and may be deteriorate to Sepsis and septic shock if not get the early and proper management. Type II MI could be happening in overcrowded ED due to delay of proper management. The QIPs with dynamic triage are Keyes to give proper management in overcrowded ED.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-106).
Case presentation
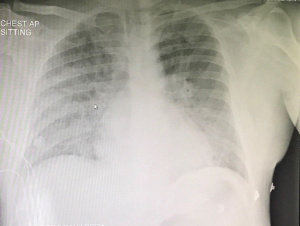
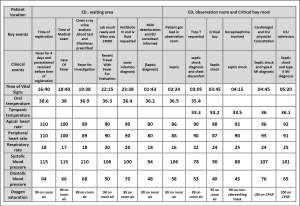
A 45-years-old, male patient with known DM type II and on regular medications, presented in our ED at the end of 2018 with fever persisting on Paracetamol for the last 4 days. He had paracetamol one gram before the time of registration. He had no significant family history and he looked like good social and behavior gentleman. He arrived from Sri Lanka a week back. On examination, he showed stable vital signs but had a body temperature of 38.6 °C and glucose of 6.6 mmol. He had no cough, sore throat, dysuria, abdominal pain, loose motion or constipation. The patient’s chest X-ray was normal (Figure 1) and urine analysis was negative. Blood culture and malaria screen were performed to determine the cause of fever. He stayed in the waiting area due to the lack of availability of bed in the observation room. However, supportive treatment was provided during the waiting period. He received 1L normal saline IV and diclofenac sodium 75 mg intramuscular IM after 30 minutes of his examination, and his body temperature dropped to 36.6 °C.
The blood test results showed leukocytosis (24,000/mm3), and accordingly, the doctor prescribed 1L normal saline and ceftriaxone 2gm IV. He had mild dropped in blood pressure about 94/48 and ED consultant was informed. After 6 hours in the waiting area, he got a bed in the observation room. Again, the blood pressure was measured to be 106/60, which dropped further (as septic shock) to be 78/53. Then, the patient complained of chest discomfort and blood troponin level requested. When blood pressure dropped to 78/53, he shifted to critical bay room. Intravenous fluid had no effect, so norepinephrine was started. His body temperature dropped to 35.5 °C and it considered as sign of sepsis. Electrocardiogram ECG was non-significant (Figure 2). Transthoracic Echo showed regional wall motion abnormality with low ejection fraction of 37% and reduced left ventricular systolic function. He had high troponin level (4,423 ng/mL). The patient was admitted to the intensive care unit (ICU). The chest X-ray was repeated, and it showed bilateral infiltration with ground glass appearance on sides (not COVID19, the case presented at the end of 2018), suggesting bronchopneumonia and pulmonary edema (Figure 3). The second X-ray was totally different than the first one that done in ED (Figures 1,3). The cardiologist diagnosed the case as Type II MI. The patient’s condition improved after proper management in ICU. The patient discharged from our hospital and he still visit our outpatient clinic for follow up.
Regarding to the timeline, the patient had 2 hours as waiting time between the registration time and the time of medical examination. He got one hour more during the medical examination. He had 6 hours more in waiting area because no bed available in observation room at that time. He had 90 minutes for supportive treatment in observation room, and then he got 90 minutes more in resuscitation room for advanced management. Finally, he admitted to the ICU. For more details about the timeline figure, vital signs and clinical events (Figure 4).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee. The authors got the permission for publication of this case report from medical research center, Hamad Medical Corporation, Qatar. It was under Ref. No.: MRC-04-19-476. Written informed consent was obtained from the patient.
Discussion and review
MI is death in cardiac Myocyte as a result of Ischemia which leads to myocardial necrosis (5). Hypoperfusion leads to ischemia and then myocardial necrosis that result in the death of myocytes. Myocardial necrosis may also lead to degradation of the cell membrane and increased level of troponin blood (6).
Ischemic heart disease involves an atheromatous plaque that leads to occlusion in the coronary artery and decreases blood supply and perfusion. It also involves other mechanisms such as myocyte death and myocardial necrosis. Demand ischemia demands increased oxygen supply, but a decrease in the oxygen supply leads to myocyte death and increased cardiac troponin level. Demand ischemia may occur in cases such as tachyarrhythmia, severe hypotension, shock, sepsis, left ventricular failure, congestive heart failure, severe acute cardiomyopathy, and Kawasaki disease (7,8).
For the fourth universal definition of MI, the 2018 joint task force of the European Society of Cardiology, American College of Cardiology, American Heart Association, and the World Health Federation defined MI as the presence of acute myocardial injury detected by abnormal cardiac biomarkers in the setting evidence of myocardial ischemia. They classified MI into 5 types: (I) ischemic myocardial necrosis because of plaque rupture, (II) ischemic myocardial necrosis resulting due to supply and demand mismatch, (III) sudden cardiac death without troponin value, (IV) procedural-related MI, including post percutaneous coronary intervention and stent thrombosis, and (V) post coronary artery bypass grafting (1,9,10).
The acute coronary syndrome includes ST elevation MI (STEMI), NSTEMI and unstable angina (UA). The first two are characterized by increased cardiac troponin level while the UA involves clinical diagnosis with ECG ischemic changes like inverted or flat T wave (11).
Cardiac troponin is a regulatory protein that controls the calcium interacting with actin and myosin. The troponin complex has three subunits: trop T, trop I and trop C (12).
The cellular mechanisms of troponin elevation are: (I) ischemia that causes hypoperfusion, leading to myocyte death and necrosis; (II) increased myocyte membrane permeability that leads to degradation of the cell membrane and increases blood troponin level as in sepsis and severe inflammatory; (III) normal turnover of myocardial cell and cell apoptosis leading to cell damage as preload ischemia; (V) demand ischemia as a result of a mismatch between oxygen demand and supply as in congenital heart disease, and sepsis (13).
Certain non-cardiac diseases can also increase cardiac troponin level, but it is considered as poor prognosis, especially in critical illness because it means some of the cardiac myocyte death and insufficient heart work. Increased cardiac troponin without coronary occlusion needs to be researched as the cause of myocardial necrosis (14,15). In chronic kidney disease, troponin may increase because of myocardial abnormalities, especially in end-stage chronic kidney disease (16). Severe burn of more than 25% may be associated with high troponin due to cardiac contractile dysfunction (16). Kawasaki disease is associated with elevation in troponin due to myocarditis and in heart failure (17). Cardioversion and defibrillation-induced myocardial injury can also increase troponin level (18). Acute stroke may also elevate cardiac troponin, especially in subarachnoid hemorrhage (19).
Sepsis is clinical syndrome resulting from severe inflammatory response due to severe infection, and it leads to multiple organ dysfunction syndromes, shock, and death. Sepsis sign may include: sign of specific infectious source such as cough, dyspnea, dysuria or wound purulent discharge, etc. Also, arterial hypotension, high temperature more than 38.3 or low temperature less than 36, Heart rate more than 90 also tachypnea and respiratory rate more than 20 breathe per minute. High white blood cells and lactic acid is considered as laboratory sign of sepsis. Disturbed conscious level (DCL) may sign of peripheral hypo perfusion in septic shock. Some of wearing score system included the body temperature to determine the risk of case deterioration. The National Early Warning Score 2 (NEWS2) is score system developed by royal college of physicians to determine the risk of sepsis in hospital case (ED, ICU, and ward). It based on the six of physiological parameters: respiratory rate, oxygen saturation, Systolic blood pressure, and pulse rate, level of consciousness or new confusion and body temperature. The score from 0 to 4 means low risk and may patient need observation every 4 to 6 hours, also the score from 5 to 6 means medium risk and indicates to observation every one hour, finally score 7 and more means high risk with continuous observation. The sequential organ failure assessment score (SOFA score) is score system to assess the critical ill patient and it based on Partial pressure of oxygen PO2, Fraction inspired Oxygen, platelet count, Glasgow coma Scale, bilirubin, renal function, hypotension and vasopressor. Other Score is quick SOFA (QSOFA) to assess the sepsis case. QSOFA based on blood pressure, respiratory rate and mental status (20-22).
Sepsis should get early recognition in the ED by nurses and doctors (News2, SOFA and Q-SOFA may help). In addition, early and aggressive treatment such as sepsis six resuscitation bundles may help to improve the prognosis (23).
Overcrowding ED is a universal problem in big hospitals that have a high flow rate. It is sometimes the cause of delay or negligence in the critical case and poor prognoses for some curable cases due to the delay in examination and management. Clinical history may remain incomplete in overcrowding hospital because of the time stress. Rectal exam and pelvis exam are sometimes missed. Triage should be useful in the waiting area as a dynamic process. Also, many researches and QIPs should be implemented to prevent the missed case and to avoid overcrowding complications (24).
In our case, the patient presented with fever with suspicion of malaria due to the lack of specific causes for fever such as cough or sore throat, or even gastrointestinal GIT symptoms also it was in 2018 before COVID 19 pandemic attack. During the patient’s waiting time, phlebotomy and medication were given. The lab result showed high leukocytes, so antibiotics with more fluid were also given to the patient, but the patient’s prognosis got worse prognosis resulting in sepsis. The patient was hypotensive with no effect of IV fluid, so norepinephrine was administered. Chest discomfort was observed with non-significant ECG (Figure 2), but much high trop T was observed. Surprisingly, the second chest X-ray findings were different from the first one (Figures 1,3). The patient was admitted to ICU, and his condition improved with good management of sepsis and MI. This indicates the requirement of a specific program or staff to re triage the patient regularly in the waiting area with early treatment after observation. Overcrowded ED can exhaust both man power and facilities.
In this case we have sequence of complications started by high fever 38.6 then sepsis following by septic shock and ended by type II MI, the prolonged waiting time in overcrowded ED is the factor that leads to the case deterioration. We recommend further research about dynamic triage (triage and re-triage) system to help overcrowded ED. QIPs are needed in general but may be each hospital needs specific QIP according to the hospital structure; also, we recommend that for further research. One of strength points in this case, it was in good medical center like Al Wakra hospital, HMC that one of high medical centers with good medical records and documentations that help us to evaluate our case study. However, the one of limitation points is the predisposing factors may have role in this case like the racial factor or the patient has type II DM but it was controlled (6.6 mmol). Any how our point in this case to avoid the serious complications from prolonged waiting time and to report one of less frequency case of type II MI that developed in our ED.
In our adult ED, Al Wakra Hospital, we had many of modifications after that case. We have now more man power: specialists, consultants and staff nurses. Every one of physicians and staff nurses should obtain sepsis course certificate and early warning system course certificate for sepsis case. We have now more observation unites with more beds. We have proper triage systems that give priorities to our patient according to the history and patient Condition. The patients with low priority get early transfer with free transportation by bus to the nearest health center to deal such that case also they triage the patient again as dynamic process, then, they send back to us the patient who need further investigations and consultations. We keep all high priority case in our department for supportive treatment and investigations. We avoid any effort to unnecessary case by triage out with free transportation to the nearest primary health center, to keep more effort for the high priority and sick case, to avoid any wasting time. We have regular rounds by consultant, senior specialist and charge nurse in waiting and observation areas to pick up any critical or sick case, also to discharge any unnecessary or stable case. The staff nurses have direct axis to the supervisor to report any prolongation in waiting time for any case. All medications and supportive treatment are giving in the proper time without any delayed. The supervisor and consultant rounds are regular and circular for dynamic triage (triage and re-triage).
Conclusions
ALWAKRA TYPE II MI: A simple case of fever deteriorated to sepsis and then type II MI after prolonged waiting time in the waiting area of ED to get a bed in the observation room. ED physician should be aware about this complication to give proper and timely management. Overcrowded ED needs more facilities, man power, and quality improvement to avoid any complication from the waiting time or missed case. The triage is a dynamic process, and all ED areas need regular re triage. Further research for dynamic triage is required to prevent such this case.
Acknowledgments
It was an E poster for the international congress only and we did not publish it in any journal before as a full article of case report. We E posted of the same case in the European Society of Emergency Medicine Congress 2019 (EUSEM 2019) that held in Prague Czech October 2019 and we posted the same case in Qatar Health 2020 that held in Doha, Qatar January 2020.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-106
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-106). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee. The authors got the permission for publication of this case report from medical research center, Hamad Medical Corporation, Qatar. It was under Ref. No.: MRC-04-19-476. Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction. J Am Coll Cardiol 2018;72:2231-64. [Crossref] [PubMed]
- Furie N, Israel A, Gilad L, et al. Type 2 myocardial infarction in general medical wards: Clinical features, treatment, and prognosis in comparison with type 1 myocardial infarction. Medicine (Baltimore) 2019;98:e17404 [Crossref] [PubMed]
- Smid J, Scherner M, Wolfram O, et al. Cardiogenic Causes of Fever. Dtsch Arztebl Int 2018;115:193-9. [PubMed]
- Salway RJ, Valenzuela R, Shoenberger JM, et al. Emergency department (ED) overcrowding: evidence-based answers to frequently asked questions. Revista Médica Clínica Las Condes 2017;28:213-9. [Crossref]
- Anderson JL, Morrow DA. Acute Myocardial Infarction. N Engl J Med 2017;376:2053. [Crossref] [PubMed]
- Reichlin T, Twerenbold R, Reiter M, et al. Introduction of high-sensitivity troponin assays: impact on myocardial infarction incidence and prognosis. Am J Med 2012;125:1205. [Crossref] [PubMed]
- Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation 2013;127:2452. [Crossref] [PubMed]
- Zeymer U, Schröder R, Tebbe U, et al. Non-invasive detection of early infarct vessel patency by resolution of ST-segment elevation in patients with thrombolysis for acute myocardial infarction; results of the angiographic substudy of the Hirudin for Improvement of Thrombolysis (HIT)-4 trial. Eur Heart J 2001;22:769. [Crossref] [PubMed]
- Mirvis D, Goldberger AL. Electrocardiography. In: Zipes DP, Bonow RO, Libby P, et al. editors. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia: Elsevier, 2018.
- Schuster EH, Bulkley BH. Early post-infarction angina. Ischemia at a distance and ischemia in the infarct zone. N Engl J Med 1981;305:1101. [Crossref] [PubMed]
- Pope JH, Ruthazer R, Beshansky JR, et al. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis 1998;6:63. [Crossref] [PubMed]
- Higgins JP, Higgins JA. Elevation of cardiac troponin I indicates more than myocardial ischemia. Clin Invest Med 2003;26:133. [PubMed]
- Thygesen K, Mair J, Katus H, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010;31:2197. [Crossref] [PubMed]
- Lim W, Qushmaq I, Devereaux PJ, et al. Elevated cardiac troponin measurements in critically ill patients. Arch Intern Med 2006;166:2446. [Crossref] [PubMed]
- Fridén V, Starnberg K, Muslimovic A, et al. Clearance of cardiac troponin T with and without kidney function. Clin Biochem 2017;50:468-74. [Crossref] [PubMed]
- Murphy JT, Horton JW, Purdue GF, et al. Evaluation of troponin-I as an indicator of cardiac dysfunction after thermal injury. J Trauma 1998;45:700. [Crossref] [PubMed]
- Checchia PA, Borensztajn J, Shulman ST. Circulating cardiac troponin I levels in Kawasaki disease. Pediatr Cardiol 2001;22:102. [Crossref] [PubMed]
- Piechota W, Gielerak G, Ryczek R, et al. Cardiac troponin I after external electrical cardioversion for atrial fibrillation as a marker of myocardial injury--a preliminary report. Kardiol Pol 2007;65:664. [PubMed]
- Naidech AM, Kreiter KT, Janjua N, et al. Cardiac troponin elevation, cardiovascular morbidity, and outcome after subarachnoid hemorrhage. Circulation 2005;112:2851. [Crossref] [PubMed]
- Smith GB, Redfern OC, Pimentel MA, et al. The National Early Warning Score 2 (NEWS2). Clin Med (Lond) 2019;19:260. [Crossref] [PubMed]
- Lambden S, Laterre PF, Levy MM, et al. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care 2019;23:374. [Crossref] [PubMed]
- Marik PE, Taeb AM. SIRS, qSOFA and new sepsis definition. J Thorac Dis 2017;9:943-5. [Crossref] [PubMed]
- Daniels R, Nutbeam T, McNamara G, et al. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J 2011;28:507-12. [Crossref] [PubMed]
- Morley C, Unwin M, Peterson GM, et al. Emergency department crowding: A systematic review of causes, consequences and solutions. PLoS One 2018;13:e0203316 [Crossref] [PubMed]
Cite this article as: Elrobaa IH, Dafalla EH, Khalid MK, Kutty MF. Al Wakra type II myocardial infarction—a case report in our emergency department. AME Case Rep 2021;5:19.




