
CT-guided percutaneous aspiration of Tarlov cyst: a case report of 2-year follow up
Introduction
In 1938, Tarlov (1) described Tarlov cysts for the first time. Tarlov cysts are characterized by sacs that contain cerebrospinal fluid (CSF), which are a rare entity, with an incidence varying from 1.5% to 9% of the adult population (2). Clinical symptoms are evident in approximately 20–30% of patients with Tarlov cysts (2). When clinical symptoms, such as low back pain, and sexual, bladder and bowel dysfunction, are present, it is suspected that arachnoid cysts arise from the sacral spinal canal, which can compress nerve roots or the sacral nerve plexus. Sitting, standing, walking, and coughing are actions that increase CSF pressure and induce symptoms. Although there are many treatment options, consensus regarding the optimal treatment strategy has not been reached. Options include CSF drainage, shunts, and microsurgical excision, each of which has advantages and disadvantages. For example, surgical decompression provides relief but also involves a risk for infection, CSF leakage, and neurological deficits (3). Although percutaneous drainage provides temporary relief, symptoms may recur within months (4). In the present report, we present a case of Tarlov cyst treated with CT-guided percutaneous aspiration. Two-year follow-up MRI confirmed a decrease in the size of the cyst. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr.2020.04.01).
Case report
A 43-year-old woman presented with pain radiating to both lower extremities. She also complained of buttock pain and anal discomfort for 4 years. The pain was aggravated by coughing. The neurological examination was normal. The patient underwent lumbosacral MRI, and the cysts demonstrated low signal on T1-weighted images and high signal, similar to CSF, on T2-weighted images. MRI revealed cystic masses involving both S2-nerve roots, 58 mm× 21 mm in diameter, on both sides (Figure 1). Bone erosion was observed on CT imaging. A caudal block was performed first. However, the patient’s symptoms were not relieved; as such, CT-guided aspiration was performed.
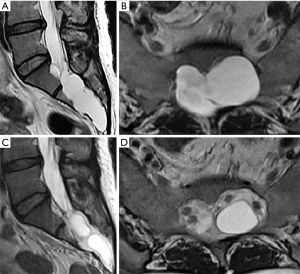
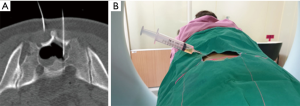
During the procedure, the patient was placed prone, and the location of the Tarlov cyst was confirmed under CT with trajectory planning. Lidocaine (1%) was injected to the entry point of the needle. An 18-gauge spinal needle was then used to perforate the S2 lamina, which is approximately 2 mm thick and easily penetrated by a spinal needle (Figure 2). Ten milliliters of CSF was aspirated. During the aspiration process, negative pressure in the cyst induced pain. After the needle was withdrawn, the entry site was cleaned with betadine and a sterile dressing was placed. The patient was followed for 2 h without complications and was then discharged with antibiotics. A 2-year follow-up MRI revealed a decrease in the size of the Tarlov cyst with two encapsulated cysts, which had less compressive effect on neural structures, resulting in no contact with bones (Figure 1).
Discussion
Simple aspiration of a symptomatic Tarlov cyst can result in frequent recurrence or even no improvement of symptoms (4). Invasiveness and possible complications of surgical excision, however, justify attempts at simple aspiration. We report a case of successful CT-guided aspiration for the treatment of a symptomatic Tarlov cyst, which decreased the size of the cyst, with improved symptoms that were maintained for 2 years.
The etiology, mechanism, and risk factors for Tarlov cysts remain unclear, although several hypotheses have been proposed. Tarlov suggested that these cysts are the result of blockage of venous drainage, arachnoidal proliferation, or an increase in CSF hydrostatic pressure (1).
For asymptomatic patients, the common approach is observation, while intervention is recommended only for symptomatic patients. Our protocol for symptomatic Tarlov cysts is to first perform a caudal block. If symptoms do not improve, aspiration is performed. When the patient does not benefit from these procedures, surgery is the next alternative.
Surgery for Tarlov cysts, however, is associated with possible complications, including CSF leak, infection, headache, dizziness, and recurrence (3). We also had a similar experience with surgery. One of our patients complained of continued headache with dizziness for 6 months after surgery, even though the wound was intact, and another experienced cyst recurrence 3 months after surgical excision.
CT-guided aspiration could be a viable, minimally invasive alternative to surgery to treat symptomatic Tarlov cysts. However, Lee et al. (4) reported no improvement in pain.
Compression of the sacral nerves can result in symptoms including pain radiating from the lumbar spine to both legs, hypoesthesia in the perineal region, bowel or urinary functional disturbance, and sexual disturbance. Cysts may increase in size and induce symptoms. In this case, comparison of preoperative and postoperative magnetic resonance images is valuable. Symptoms are mostly related to increased cyst size that compress neural structures.
Despite the small sample size, our results demonstrate that CT-guided aspiration of a Tarlov cyst can decrease the size of the cyst, which can be maintained for up to 2 years. Considering the possible complications of surgical excision of Tarlov cysts, CT-guided aspiration can be a safe and easy treatment option.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr.2020.04.01
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr.2020.04.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the noncommercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tarlov IM. Sacral nerve-root cysts: another cause of the sciatic or cauda equina syndrome. J Neuropathol Exp Neurol 1953;11:22-7.
- Langdown AJ, Grundy JR, Birch NC. The clinical relevance of tarlov cysts. J Spinal Disord Tech 2005;18:29-33. [Crossref] [PubMed]
- Mummaneni PV, Pitts LH, McCormack BM, et al. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery 2000;47:74-8; discussion 78-9. [PubMed]
- Lee JY, Impekoven P, Stenzel W, et al. CT-guided percutaneous aspiration of Tarlov cyst as a useful diagnostic procedure prior to operative intervention. Acta Neurochir (Wien) 2004;146:667-70. [Crossref] [PubMed]
Cite this article as: Sahin E, Lee SH, Eun SS. CT-guided percutaneous aspiration of Tarlov cyst: a case report of 2-year follow up. AME Case Rep 2020;4:11.


