Diagnosis of plexiform schwannoma of the foot in a 66-year-old male: a case report and literature review
Introduction
Plexiform schwannoma is a rare type of benign peripheral nerve sheath tumor, which was first reported by Harkin in 1978 (1). It is a special variant of schwannoma, accounting for about 2–5% of all schwannomas, and the average age of patients is 34 (2). Plexiform schwannomas are more common in the trunk, head, neck, and upper extremity, most of which manifests as superficial nerve nodules less than 2 cm in diameter (3). However, it rarely occurs in the lower extremity. Thus, there are few cases reported in the literature and most of literatures reports the size of the tumor is smaller (<3 cm). Herein, we reported a case of 66-year-old patient with plexiform schwannoma in theof right foot and the tumor size is larger than 7 cm in dimension. We also reviewed literature and made comparison with the case in our study. We present the following article/case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-81).
Material and methods
We reviewed the medical records and obtained the report, diagnosis, treatment, and clinical results. This study was approved by the ethics committee of Centro Hospitalar Conde de São Januário. We also conducted a comprehensive literature search using PubMed. The following search terms were used separately or in combination: plexiform schwannoma of lower extremity, peripheral nerve sheath tumor of lower extremity. In this case who admitted to our hospital, we collected clinical manisfestations, imaging findings, treatment, outcome and clinical follow up.
Case presentation
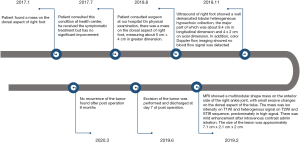
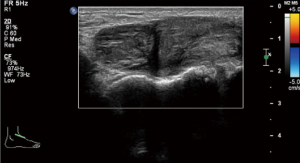
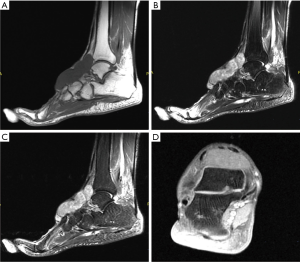
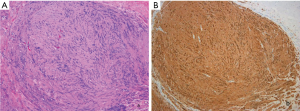
The patient was a 66-year-old male presented with soft tissue mass on his right foot for 3 years. A mass appeared on the dorsal side of his right foot 3 years ago, with no history of trauma. .He had neither medical history, family history, or psycho-social history including relevant genetic problems, nor a family history of neurofibromatosis. He also denied any pain, numbness, and weakness. He stated the lesion had enlarged in the last 6 months and had been consulted in health center, but did not improve after symptomatic treatment. He was referred to surgery department for further management. On physical examination, a mass was found on the dorsal aspect of right foot, measuring about 5cm × 4cm. The patient underwent ultrasound initially and found a well demarcated lobular heterogeneous hypoechoic collection, the major part of which was about 9.4 cm in longitudinal dimension and 4 cm × 2 cm on axial dimension. In addition, color Doppler flow imaging showed no blood flow signal was detected on the right dorsal foot, between the subcutaneous layer and the skeleton (Figure 1). Further examinations were scheduled for differential diagnosis of lipoma and soft tissue mass. A subsequent MRI examination revealed a multinodular shape mass on the anterior side of the right ankle joint, with small erosive changes on the dorsal aspect of the talus. The mass was iso-intensity on T1WI and heterogenous signal on T2WI and STIR sequence, predominately in high signal. There was mild enhancement after intravenous contrast administration. The size of the lesion was approximately 7.1 cm × 2.1 cm × 2 cm (Figure 2). The preferred diagnosis was schwannoma, but differential diagnosis of hemangioma and Morton neuroma was needed for final confirmation. Then, the tumor was excised for pathological examination. Pathological microscopy showed well circumscribed nodular fragments imparted plexiform nodularity, exhibiting alternating hypercellular and hypocellular zones. The lesion was composed of spindle cells with wavy nuclei and fibrillary cytoplasm. Some nuclear palisading and Verocay bodies were noted. Some of the nuclei showed ancient change. Hyaline vessels were seen. Immunohistochemistry showed the lesion was diffusely in positive for S-100 protein (Figure 3). After surgery, patient recovered well and found no complication. There was no recurrence at 9 months after the operation. The medical timeline was shown in Figure 4. All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of Centro Hospitalar Conde de São Januário and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Literature review
Nine cases of plexiform schwannoma of lower extremity were found in the literature. A total of 10 cases were analyzed, including our case (Table 1).
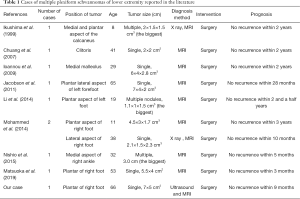
Full table
Discussion
Plexiform schwannoma is a special subtype of schwannoma. Schwannoma, also known as Schwann cell tumor, is a tumor developed from Schwann sheath of peripheral nerve. It was classified into seven subtypes by Erlandson in 1985: traditional, cranial, cellular, plexiform, archaic, melanocytic, and granulocytic (4), and the plexiform type only accounts for about 5% of them. Plexiform schwannoma is a rare skin tumor, but not neurofibromatosis (5). According to the literature, the minimum age of onset of plexiform schwannoma is 8 years, and the maximum is 65 years. The size of the tumor ranged from 1.5 to 7 cm (6-11). All the tumors were located in the plantar and lateral areas. The case in our study was a 66-year-old elderly patient with a large mass on his right foot.
There are two types of schwannomas: Antoni A and B. Antoni A is characterized by: (I) Schwann cells are usually arranged in sinusoidal or gyral bundles with fine connective tissue fibers; (II) the nucleus tends to be arranged in palisade and alternates with non-nuclear regions. While the Antoni B is characterized by loosely and disorderly organized Schwann cells and fine reticular connective tissue. Type B tissue is variable, forming small cysts and fusing into large cysts (12).
Plexiform schwannoma is not combined with neurofibromatosis and has no malignant tendency. The tumor often grows eccentrically. The incidence of necrosis, cystic degeneration and mycosis is higher than that of neurofibroma. It can be seen that, on the MRI, the signal of Antoni-A area and Antoni-B area are more uneven, and the signal is significantly higher on T2WI (13).
Ultrasound is used to distinguish schwannoma from other soft tissue tumors, although it cannot differentiate the schwannoma, neurofibroma and malignant peripheral schwannoma. Most of the peripheral nerve sheath tumors were homogeneous and hypoechoic. Doppler imaging of vascularity can identity peripheral nerve sheath tumor from the ganglion cyst (14,15). When a solid mass is diagnosed by ultrasound, the continuity of the peripheral nerve should be evaluated, because this continuity suggests the diagnosis of a peripheral schwannoma rather than other solid masses (16).
MRI has the characteristics of high-resolution and multi-plane imaging. It can not only accurately display the shape, size, and location of tumor, understanding the relationship between tumor and adjacent blood vessels and nerves, wrapping or invasion, but also indicate the change of tumor signal intensity, judging the histological characteristics of tumor accordingly and inferring its biological behavior. The provided information of growth mode and morphological characteristics is the important basis for the selection and formulation of plexiform schwannoma treatment plan. All the cases were diagnosed via MRI in the literature. and 2 of them were performed the X ray initially but were finally confirmed by MRI (6-11).
At diagnosis by MRI, plexiform schwannoma should be differentiated from plexiform neurofibroma, lipoma, hemangioma and myxoma. Plexiform neurofibroma is located in the important nerve distribution areas. The involved nerves are diffusely twisted and thickened in a plexiform shape and surrounded by cystic nodules of different sizes, which show peanut-like cluster or bead-like changes, equal or slightly low signal on T1WI, slightly high or high signal on T2WI. The tumor has clear boundary with surrounding tissues, showing “target sign” or “separation fat sign”. The “target sign” in MRI shows low signal in the center of lesion and high signal area in the surrounding, because the center of the lesion is fibrous collagen tissue and the surrounding is myxomatous tissue. Although this sign is highly suggestive of neurofibroma, it is occasionally also seen in schwannomas and malignant peripheral nerve sheath tumors. In hemangioma, there are blood vessels in or around the hemangioma, which may have characteristic structures such as fat and phleboliths. The lesions show equal or slightly high signal on T1WI, high signal on T2WI, and “light bulb sign”. Compared with other soft tissue tumors, the signal of the lesions is higher, and the enhancement of the lesions is obvious. The stroma of myxoma contains a lot of mucus, which is usually oval, parallel to the long axis of muscle and with clear boundary. The signal is equal to or lower than muscle on T1WI and is higher than fat signal on T2WI, without obvious enhancement (17). Lipoma showed high signal intensity on T1, saturated fat sequence showed saturation with no or only slight enhancement. Fast spin-echo T2 shows high signal (18).
CT is not as sensitive or specific as MRI in the diagnosis of schwannoma, but it is often used for preliminary detection and obtain the preliminary results. Besides, it is particularly useful when assessing changes in bone adjacent the tumors (Table 2).
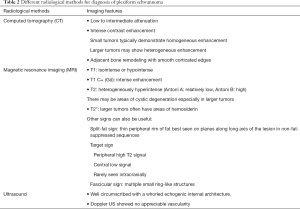
Full table
In this case, the patient was performed the ultrasound at first but the typical characteristics of plexiform schwannoma were not seen. The following MRI showed typical features of schwannoma and the “target sign” noted within the lesion. The final pathological examination confirmed the diagnosis.
Surgical resection is the first choice for plexiform schwannoma treatment, but local recurrence sometimes occurs and is not uncommon. The causes are usually incomplete surgical resection as well as the irregular and finger-like growth of the tumor. The residual tumors after surgical resection can cause more rapid recurrence, but no metastasis, and the prognosis is good (19). The patient was followed up for 9 months without recurrence.
Our study has some limitations. Because this is a single case report, the sample size is too small. In addition, follow-up time is relatively short, compared with other literature. Despite the small sample size in our study, the diagnosis of huge plexiform schwannoma in an elderly patient was rare and can provide more useful clinical information of plexiform schwannoma. Further characterization of radiological features of plexiform schwannoma by more precise clinical studies is required.
In conclusion, the incidence of plexiform schwannoma is relatively low, and its differential diagnosis from plexiform neurofibroma and other tumors is difficult. Imaging examination of CT, ultrasound and MRI can clearly show the location and extent of tumor and its relationship with adjacent structures, thereby guiding the surgery. These radiological modalities can be combined for diagnosis of plexiform schwannoma, but the final diagnosis should be based on pathology. This case report provides a deeper understanding of plexiform schwannoma in order to reduce the chance of misdiagnosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-81
Peer Review File: Available at http://dx.doi.org/10.21037/acr-20-81
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-81). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of Centro Hospitalar Conde de São Januário and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harkin J. Benign plexiform schwannoma, a lesion distinct from plexiform neurofibroma. J Neurolpathol Exp Neurol 1978;37:622. [Crossref]
- Chuang WY, Yeh CJ, Jung SM, et al. Plexiform schwannoma of the clitoris: Case report. Apmis 2007;115:889-90. [Crossref] [PubMed]
- Ioannou M, Papanastassiou I, Iakowidou I, et al. Plexiform schwannoma of the posterior tibial nerve: a case report. Cases J 2009;2:8392. [Crossref] [PubMed]
- Erlandson RA. Peripheral nerve sheath tumors. Ultrastruct Pathol 1985;9:113-22. [Crossref] [PubMed]
- Berg JC, Scheithauer BW, Spinner RJ, et al. Plexiform schwannoma: a clinicopathologic overview with emphasis on the head and neck region. Hum Pathol 2008;39:633-40. [Crossref] [PubMed]
- Nishio J, Mori S, Nabeshima K, et al. Successful enucleation of large multinodular/plexiform schwannoma of the foot and ankle. Springerplus 2015;4:260. [Crossref] [PubMed]
- Ikushima K, Ueda T, Kudawara I, et al. Plexiform schwannoma of the foot. Eur Radiol 1999;9:1653-5. [Crossref] [PubMed]
- Li XN, Cui JL, Christopasak SP, et al. Multiple plexiform schwannomas in the plantar aspect of the foot: case report and literature review. BMC Musculoskelet Disord 2014;15:342. [Crossref] [PubMed]
- Matsuoka Y, Kakudo N, Fukui M, et al. Giant plexiform schwannoma in the plantar aspect of the foot: a case report. J Surg Case Rep 2019;2019:rjz352. [Crossref] [PubMed]
- Mohammed SA, Pressman MM, Schmidt B, et al. Case presentations and review of plexiform schwannoma in the foot. J Foot Ankle Surg 2014;53:179-85. [Crossref] [PubMed]
- Jacobson JM, Felder JM 3rd, Pedroso F, et al. Plexiform schwannoma of the foot: a review of the literature and case report. J Foot Ankle Surg 2011;50:68-73. [Crossref] [PubMed]
- Fletcher CD, Davies S. Benign plexiform (multinodular) schwannoma: a rare tumour unassociated with neurofibromatosis. Histopathology 1986;10:971-80. [Crossref] [PubMed]
- Yamada K, Harada M, Kunitoku N, et al. MR imaging features of a scalp plexiform schwannoma. AJNR Am J Neuroradiol 2004;25:291-4. [PubMed]
- De Flaviis L, Nessi R, Bo PD, et al. High‐resolution ultrasonography of wrist ganglia. J Clin Ultrasound 1987;15:17-22. [Crossref] [PubMed]
- Ortega R, Fessell DP, Jacobson JA, et al. Sonography of ankle ganglia with pathologic correlation in 10 pediatric and adult patients. AJR Am J Roentgenol 2002;178:1445-9. [Crossref] [PubMed]
- Silvestri E, Martinoli C, Derchi LE, et al. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology 1995;197:291-6. [Crossref] [PubMed]
- Nishimoto K, Kusuzaki K, Matsumine A, et al. Surrounding muscle edema detected by MRI is valuable for diagnosis of intramuscular myxoma. Oncol Rep 2004;11:143-8. [Crossref] [PubMed]
- Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol 2004;182:733-9. [Crossref] [PubMed]
- Kron M, Bohnsack BL, Archer SM, et al. Recurrent orbital schwannomas: clinical course and histopathologic correlation. BMC Ophthalmol 2012;12:44. [Crossref] [PubMed]
Cite this article as: Ieong CM, Kong SC. Diagnosis of plexiform schwannoma of the foot in a 66-year-old male: a case report and literature review. AME Case Rep 2020;4:34.