
The curious case of an atypical headache, a case report and review of literature
Introduction
Patients with headaches are frequent occurrences in primary care practices. The headaches have an estimated lifetime prevalence of 66%—of which, 14% to 16% corresponds to migraine, 46% to 78% to tension-type headache, and 0.1% to 0.3% for cluster headache (1-3). The economic effects of a headache are also substantial. It is estimated that headache accounts for 20% of work absences (4).
Tension-type headaches have an increased incidence in patients observing fasting. The frequency of these headaches also increases with the duration of the fast and may be associated with factors like hypoglycemia, caffeine withdrawal, dehydration, or lack of sleep (5). Management of these headaches is dependent on the physician’s ability to effectively assess and diagnose them. It is important to obtain an extensive history and physical examination in order to identify any possible causes of headaches (6). Acyclovir is frequently started empirically in patients with clinical suspicion of infective encephalopathy, even if the etiology is unknown (7).
Acute viral encephalitis is a neurological emergency which often requires prompt diagnosis and treatment to prevent severe disability or death. Making this diagnosis hinges crucially on a lumbar puncture (LP) that is often delayed in practice (8).
We report the case of a 37-year-old male, who presented to the family medicine practice with persistent headaches which subsided postprandial and was later, was admitted to the hospital for stroke-like symptoms. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-88).
Case presentation
A 37-year-old male with no prior history of headaches presented with a 2-week history of severe right-sided headaches behind the eye. The patient also reported a previous episode of blurry vision in his left eye a week before the onset of right-sided headache. During this time the patient was fasting for religious reasons and stated that the headache was accompanied with vomiting without nausea which subsided after a meal. The patient stated that he had recently traveled to India for a conference a month prior to the onset of his symptoms, but did not visit any rural areas or get ill during his visit. He did not report any previous episodes.
On examination, his vital signs were normal and he appeared mildly anxious. Upon central nervous system (CNS) examination, pupils were equal, round and reactive to light, cranial nerves II–XII were intact, reflexes were symmetric and intact bilaterally, Glasgow Coma Scale of 15, and no meningeal signs or photophobia.
The initial diagnosis of migraines secondary to hypoglycemia while fasting was made. The patient was requested to discontinue fasting until his symptoms resolved along with 50 mg of Cambia. A follow-up appointment was scheduled for 1 week.
The patient’s symptoms worsened and presented to the emergency room (ER) the following day with sudden onset of dysstasia, aphasia, with right-sided hemiparesis and fluctuating loss of consciousness (LOC). He reported intermittent headaches, generally worse in the back of the head and right-sided blurriness. He did not have any neck stiffness or back pain. The patient reported that he was asymptomatic in the morning but noted unsteady gait, and staring spells as the day progressed. He then began to have worsening dysphasia and dysarthria; however, he was able to follow commands and instructions.
Given the severity of his symptoms, the patient was admitted to the hospital for further evaluation. Initially, he was empirically managed with intravenous (IV) ceftriaxone 2 g Q12, vancomycin 1 g Q12, and acyclovir 800 mg Q6 for suspected viral encephalitis. Computed tomography (CT) angiogram of the head and neck showed no acute intracranial abnormality. The patient’s CT was non-diagnostic and magnetic resonance imaging (MRI) confirmed no acute intracranial abnormalities.
Traumatic LP revealed an opening pressure of 35, protein 2.89 g/L, white blood cell (WBC) 133 (106/L) with 53% lymphocytes, red blood cell (RBC) 38,000 (106/L). However, cerebrospinal fluid (CSF) showed no evidence of Japanese encephalitis, HSV (type 1 or 2), varicella-zoster virus, enterovirus, or parechovirus. Serum tests for HIV, West-Nile virus PCR, Ebstein-Barr virus, cytomegalovirus, and viral hepatitis (A, B, and C) also yielded non-diagnostic results.
Electroencephalogram (EEG) was recorded in a confused patient during wakefulness and drowsiness. There was mild to moderate diffuse slowing of the background which appeared nonspecific secondary to a mild encephalopathic process. In addition, there was a continuous delta slowing over the left hemisphere through the recording that could be due to structural lesions or postictal changes. There were no definite epileptiform discharges, electrographic seizures, or evidence of non-convulsive status epilepticus.
The patient received 10 days of IV acyclovir which showed improvement in the repeat LP; protein 0.67 g/L, WBC 28 (106/L) with 94% lymphocytes, RBC 73 (106/L) with negative CSF infectious workup. Antibody screening was conducted and ruled out autoimmune encephalitis.
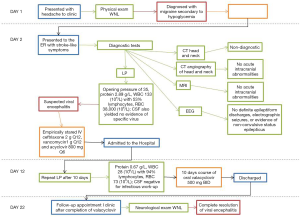
Ten days after admission, he was discharged with 10 days of valacyclovir 500 mg twice a day (BID) for a total of a 20-day course of anti-viral. The patient presented to the outpatient clinic after concluding the valacyclovir. Neurological examination was within normal limits (WNLs) and the patient had complete resolution of viral encephalitis. Figure 1 describes the timeline for the sequence of events in chronological order. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript.
Discussion
Patients with headaches are frequent occurrences in primary care practices. The headaches have an estimated lifetime prevalence of 66%—of which, 14% to 16% corresponds to migraine, 46% to 78% to tension-type headache, and 0.1% to 0.3% for cluster headache (1-3). The economic effects of a headache are also substantial. It is estimated that headache accounts for 20% of work absences (4). Majority of these headaches are managed in an outpatient setting without an immediate referral to the emergency department or non-emergent referral to the neurologist. These headaches can be caused by psychosocial factors, prescription medications, or other neurological conditions like migraines. Effective management of these headaches heavily depends on the physician’s ability to assess and diagnose. A detailed and focused history, along with a complete physical examination is essential to identify any causes of headaches. Early detection and diagnosis from the presenting illness allow creating an effective management plan.
Encephalitis is a pathological term meaning inflammation of the brain. This inflammation can be ascertained clinically by patients presenting with fever, seizures, or functional neurological deficits, CSF parameters, imaging, or EEG. CSF typically exhibits increased pressure with a slightly elevated protein and normal glucose concentration. Glaser et al. reports that even in patients with clear signs of an acute infection, more than 10% did not exhibit an underlying relationship to the illness (9). Acute viral encephalitis is a neurological emergency, which often requires prompt diagnosis and treatment to prevent severe disability or death. Making the diagnosis of viral encephalitis hinges crucially on a LP, which is often delayed in practice (8).
Headaches have an increased incidence in patients observing fasting (5). While following the “Guideline for primary care management of headache in adults”, our patient presented without red-flag symptoms to rule out any secondary causes of headache (10). In a previous study, Awada et al. reports that 41% of patients fasting have a headache predominantly of tension-type. The frequency of these headaches also increases with the duration of the fast and may be associated with factors like hypoglycemia, caffeine withdrawal, dehydration, or lack of sleep (5). The resolution of our patient’s headache, with a meal after a prolonged state of fasting, can certainly mask the underlying symptoms of the patient. Therefore, the threshold for referral of atypical headaches or unusual headache precipitants should be low.
Not every patient will present with classic headache symptoms. These patients should be followed up more frequently to monitor changes in their presentation. More insidious causes for a headache, such as viral infections, should not be ruled out. If the symptoms are acute and severe, an immediate inpatient work-up with empiric treatment for the most probable etiology may be warranted, despite unequivocal exam and laboratory findings. Acyclovir is frequently started empirically in patients with clinical suspicion of infective encephalopathy, even if the etiology is unknown. However, Chaudhuri et al. reports that acyclovir has no therapeutic benefit in patients with non-herpetic encephalitis (7). This leads us to believe that our patient in fact did have herpes simplex virus encephalopathy despite yielding no results in the CSF.
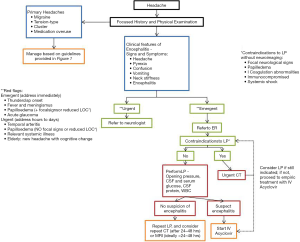
Primary care physicians tend to refer mainly to the pathway presented in the referenced flowchart (Figure 2) (10). However, as per the uncharacteristic presentation of our patient, it is essential to think beyond the four main subgroups of headaches. Educating the patient on potential red flags and creating a safety plan is paramount to the outcome in patients with atypical headaches. Figure 3 illustrates a suggested guideline for primary care physicians in atypical presentation (10,11).
Effective management of headaches in an outpatient setting is heavily dependent on the physician’s ability to assess and diagnose through a focused history and a complete physical examination. Physicians have a referral bias towards diagnostically challenging cases based on the severity of the patient’s presenting illness (9). While making the diagnosis of viral encephalitis hinges crucially on a LP, failure to identify and treat these headaches due to delayed testing may lead to more serious sequelae. Glaser et al. also states the need for new approaches and better tools for identifying the etiology (9).
Conclusions
This case highlights the importance of diagnosing headaches promptly in patients with atypical presentations. In addition, when these findings are identified, a full history including a timeline of the symptoms should be conducted. Given that the prevalence of adult headaches in primary care is fairly frequent, it is not realistic or practical to investigate every patient with an LP or radiological imagining of the brain. However, it is important to have careful consideration of the signs and symptoms presented. A significant portion of the consultation should incorporate patient education regarding red flag symptoms and safety planning. Furthermore, with the possibility of subtle presentation and the nonspecific symptoms of viral encephalopathy, physicians are urged to keep this diagnosis on their differential for headaches.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-88
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-88). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bigal ME, Lipton RB, Stewart WF. The epidemiology and impact of migraine. Curr Neurol Neurosci Rep 2004;4:98-104. [Crossref] [PubMed]
- Robbins MS, Lipton RB. The epidemiology of primary headache disorders. Semin Neurol 2010;30:107-19. [Crossref] [PubMed]
- Stovner Lj, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27:193-210. [Crossref] [PubMed]
- Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. J Neurol Neurosurg Psychiatry 2006;77:385-7. [Crossref] [PubMed]
- Awada A, al Jumah M. The first-of-Ramadan headache. Headache 1999;39:490-3. [Crossref] [PubMed]
- Lee VME, Ang LL, Soon DTL, et al. The adult patient with headache. Singapore Med J 2018;59:399-406. [Crossref] [PubMed]
- Chaudhuri A, Kennedy PG. Diagnosis and treatment of viral encephalitis. Postgrad Med J 2002;78:575-83. [Crossref] [PubMed]
- Ellul M, Solomon T. Acute encephalitis - diagnosis and management. Clin Med (Lond) 2018;18:155-9. [Crossref] [PubMed]
- Glaser CA, Honarmand S, Anderson LJ, et al. Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin Infect Dis 2006;43:1565-77. [Crossref] [PubMed]
- Guideline for primary care management of headache in adults. 2016. Available online: www.topalbertadoctors.org/cpgs/10065
- Solomon T, Michael BD, Smith PE, et al. Management of suspected viral encephalitis in adults--Association of British Neurologists and British Infection Association National Guidelines. J Infect 2012;64:347-73. [Crossref] [PubMed]
Cite this article as: Paracha H, Hussain SA. The curious case of an atypical headache, a case report and review of literature. AME Case Rep 2020;4:28.



