Successful management requiring multidisciplinary cooperation between seven departments for a large right-sided incarcerated traumatic diaphragmatic hernia: a case report and review of literature
Introduction
Patients with delayed traumatic diaphragmatic hernia (TDH) often experienced a history of penetrating or blunt trauma. TDH from blunt thoracoabdominal trauma occurs in approximately 0.5% and 20% (1), located more frequently in right-sided thorax (13%) in contrast to the common left-sided (75%) (2). This entity is sometimes difficult to ascertain after acute trauma and then consequently give rise to diagnostic delays with life-threatening outcomes. Herein, we present a rare case of incarcerated TDH at the right-side presenting as dramatic dyspnea and acute gastrointestinal obstruction, which required urgent operative repair. We present the following case in accordance with the CARE Guideline (3).
Case presentation
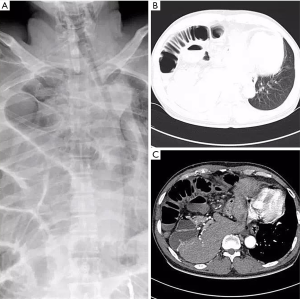
We encountered with a 52-year-old male patient complaining of progressive shortness of breath and vomiting of 2 days’ duration. Following admission to the hospital, breathlessness on this patient gone to no significant improvement after mask oxygen inhalation. The pain on chest, shoulder and abdomen also occurred in this patient as well as tachycardia. His symptoms of dyspnea on exertion and dysuresia became more severe gradually during the past 3 years and affected his quality of life in the last few months. There was a history of fall injury from 5 m at work 10 years ago during which, he suffered from a fourth lumbar vertebral burst fracture, pelvic fracture and posterior urethral injury. Reconstruction of ruptured urethra was performed for him then. Physical examination revealed absent breath sounds on the right-side and deviation of the trachea to the left-side. Otherwise, there was abdominal sound disappearance and tachycardia at heart rate of 121 bpm. Emergent chest X-ray shown the amazing presence of swelling bowel loops stuffed the whole right thoracic cavity and remarkable displace of the mediastinum to the left-side (Figure 1A). CT scan demonstrated herniation of liver, cholecyst, sectional stomach and bowel loops into the right thorax (Figure 1B,C). Arterial blood gas analysis indicated hypoxemia: pH 7.33, PCO2 48 mmHg, PO2 71 mmHg, SO2 92%.
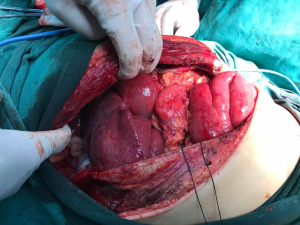
This patient underwent an urgent operation when the diagnosis of an incarcerated TDH was erected. After general anesthesia induction which, needed an experienced anesthetist timely deal with the location of double-lumen tube and high airway pressure with low ventilation, he received a cystostomy after ultrasonic guidance as the incapability of urethral catheterization due to posterior urethral stricture. We found a 19 cm diaphragmatic laceration though centrum tendineum from the posterior sternal hiatus to the 12th thoracic vertebra. The two edges of the 12 cm anterior part of diaphragmatic laceration were smooth scar tissues, and the end was fresh ruptures. Liver, cholecyst, stomach and jejunum loops were discovered to herniate into the right thorax (Figure 2). Meanwhile, transthoracic incision was extended to the right upper abdomen to reduce the liver and cholecyst to peritoneal cavity and jejunum sectional resection and anastomosis was performed during the exploratory operation. A piece of prosthetic material was required to cover the large diaphragmatic rupture (Figure 3). He was then sent to ICU for further life support and considered surgical cured when discharge. A X-ray confirmed complete reduction of herniated organs and full reexpansion of the right lung. Dilatation of urethral stricture was done during his postoperative follow-up.
Comment
TDH acquired after a blunt or penetrating trauma with a 3:1 ratio (4). The most predominant cause of TDH is blunt thoracoabdominal trauma, such as traffic accident and fall from height (5). The left TDH is more commonly seen and the right is relatively rare. Diaphragmatic rupture 76% appear in the left, 22% in the right and 2% with bilateral lesions in TDH (6). An acute TDH is often difficult to determine in patients following severe thoracic or thoracoabdominal injuries. CT scan usually shows low sensitivity in diagnosing TDH with a rate of missed diagnosis in 17% to 63% (7,8). The misdiagnosis may lead to strangulation of the incarcerated abdominal viscera, with a mortality rate between 30% and 60% (9), especially for right TDH, usually incompatible with life and predictive of mortality (10). In this report, this patient was referred to our institute with a suspected diagnosis of right hydropneumothorax, namely dramatic respiratory distress, absent breath sounds on the right thorax and displace of the trachea to the left, hypoxemia. Diaphragmatic rupture should be likely to be neglected after his accident fall from height 10 years ago and developed larger with abdominal pressure improved after dysuresia due to posterior urethral stricture. The smooth scar tissues of the anterior part of diaphragmatic laceration appears to indicate the diaphragmatic rupture caused by his previous accident fall. However, what should be kept in our mind is that the rate of initially missed diaphragmatic injuries can be as high as 66% (11). When tracing the patient’s image data 10 years ago, we found no sign of diaphragmatic injury, meanwhile, Miller et al. once reported that 40 patient’s normal radiographs were found in a series of 93 patients with penetrating injuries of the diaphragm (12). Delayed diagnosis of TDHs resulted in this life-threatening outcome.
Obviously, the immediate surgical approach must be mandatory and a delay in the intervention can lead to death in this patient. TDH is traditionally treated trough a transthoracic or transabdominal approach, meanwhile, a thoracoscopic or laparoscopic pathway has also been proposed more commonly (13-15). Silva et al. pointed out abdominal approach is three times more common than the thoracic, regardless of acute and chronic phase in TDH (6). Furthermore, abdominal pathway is the primary surgical approach in unstable patients with abdominal visceral injuries according to Sukul (16). However, abdominal pathway was not suitable for this patient due to lager diaphragmatic rupture and visceral contents stuffed the whole right thorax. Therefore, hepatobiliary and gastrointestinal surgeons were introduced in advance and got ready for abdominal operation preoperatively. After liver and cholecyst’s restoration after dividing the diaphragmatic adhesion by the former as well as jejunum sectional resection and anastomosis by the later, the giant diaphragmatic rupture was then amenable to be closed with a piece of prosthetic material. ICU’s postoperative management is also indispensable in this case. Successful management required a coordinated effort between anesthetist, sonographer, intensive care specialist, thoracic, urological, hepatobiliary and gastrointestinal surgeons. Tight and active multidisciplinary cooperation in this case manifested the positive energy in emergent resuscitation.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr.2020.03.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Filosso PL, Guerrera F, Sandri A, et al. Surgical management of chronic diaphragmatic hernias. J Thorac Dis 2019;11:S177-85. [Crossref] [PubMed]
- Asensio JA, Petrone P. Diaphragmatic injury. In: Cameron JL. Current surgical therapy. 8th ed. Philadelphia: Elsevier Mosby Co., 2004:946-55.
- Riley DS, Barber MS, Kienle GS, et al. CARE 2013 explanations and elaborations: reporting guidelines for case reports. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Shah R, Sabanathan S, Mearns AJ, et al. Traumatic rupture of diaphragm. Ann Thorac Surg 1995;60:1444-9. [Crossref] [PubMed]
- Marchard P. A study of the forces productive of gastroesophageal regurgitation and herniation through the diaphragmatic hiatus. Thorax 1974;12:105-12.
- Silva GP, Cataneo DC, Cataneo AJM. Thoracotomy compared to laparotomy in the traumatic diaphragmatic hernia. Systematic review and proportional methanalysis. Acta Cir Bras 2018;33:49-66. [Crossref] [PubMed]
- Hofmann S, Kornmann M, Henne-Bruns D, et al. Traumatic diaphragmatic ruptures: clinical presentation, diagnosis and surgical approach in adults. GMS Interdiscip Plast Reconstr Surg DGPW 2012;1:Doc02. [PubMed]
- Panda A, Kumar A, Gamanagatti S, et al. Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagn Interv Radiol 2014;20:121-8. [PubMed]
- Nchimi A, Szapiro D, Ghaye B, et al. Helical CT of blunt diaphragmatic rupture. AJR Am J Roentgenol 2005;184:24-30. [Crossref] [PubMed]
- Lim KH, Park J. Blunt traumatic diaphragmatic rupture: Single-center experience with 38 patients. Medicine (Baltimore) 2018;97:e12849. [Crossref] [PubMed]
- Reber PU, Schmied B, Seiler CA, et al. Missed diaphragmatic injuries and their long-term sequelae. J Trauma 1998;44:183-8. [Crossref] [PubMed]
- Miller L, Bennett EV Jr, Root HD, et al. Management of penetrating and blunt diaphragmatic injury. J Trauma 1984;24:403-9. [Crossref] [PubMed]
- Porojan VA, David OI, Coman IS, et al. Traumatic diaphragmatic lesions - considerations over a series of 15 consecutive cases. Chirurgia (Bucur) 2019;114:73-82. [Crossref] [PubMed]
- Takaichi S, Takahashi T, Funaki S, et al. Laparoscopic repair of an incarcerated diaphragmatic hernia after right hepatectomy for hepatic injury: a case report. Surg Case Rep 2018;4:135. [Crossref] [PubMed]
- Furák J, Athanassiadi K. Diaphragm and transdiaphragmatic injuries. J Thorac Dis 2019;11:S152-7. [Crossref] [PubMed]
- Sukul DM, Kats E, Johannes EJ. Sixty-three cases of traumatic injury of the diaphragm. Injury 1991;22:303-6. [Crossref] [PubMed]
Cite this article as: Wei F, Li Y. Successful management requiring multidisciplinary cooperation between seven departments for a large right-sided incarcerated traumatic diaphragmatic hernia: a case report and review of literature. AME Case Rep 2020;4:10.