
Secondary atlantoaxial subluxation in isolated cervical dystonia—a case report
Introduction
Dystonia is characterized by sustained (or intermittent) simultaneous contractions of the agonist and antagonist muscles, causing twisting and repetitive movements (dystonic tremor) or abnormal fixed postures (1). Focal dystonia involving the neck muscles is called “cervical dystonia” (CD), also known as spasmodic torticollis. CD is classified as an isolated (primary) dystonia if there is no identifiable underlying cause. CD can occur as a consequence of another disorder or condition and be considered acquired (secondary). Dystonic movements have a typical pattern and are twisting, may be tremulous (2). The essential pathophysiological feature of dystonia is co-contraction of antagonistic muscles. CD can have a profound impact on patients’ quality of life due to painful neck twisting, repetitive head movements, and psycho-social stress (3). The diagnosis is based on clinical observation. Laboratory or imaging test have no validation in confirming the diagnosis of CD (2). Several treatment options are available for patients with CD. In mild cases, physiotherapy and muscles relaxants may be available. In general settings, intramuscular injection of botulinum neurotoxin remains the mainstay of treatment for most focal dystonia syndromes (2,3). This case demonstrates an association between CD and atlantoaxial subluxation, which was previously unreported. We present the following case in accordance with the CARE Guideline.
Case presentation
A 14-year-old girl was referred to our chiropractic clinic with left head tilt and bilateral neck pain. In the beginning, the girl noticed a feeling of tremor and pulling in the right neck which appeared only from time to time. Her family doctor, at first, gave her a tentative diagnosis of CD and prescribed some non-steroidal anti-inflammatory drugs and muscle relaxants without improvements. As the disease progresses in a couple of months, she experienced head tilting to the right side, twisting of the neck and right occipital headache. These symptoms aggravated in both stressful situations and during physical strain. The girl was withdrawn, socially anxious and unhappy about her awkward looks. For nearly a year, she had to seek medical treatment for her painful dystonia, and previously received three botulinum toxin injections at 3-month intervals, along with physiotherapy and acupuncture. These regimens brought slight relief of the CD. The combination of psychotherapy and antidepressant could not help reduce her anxiety and pain.
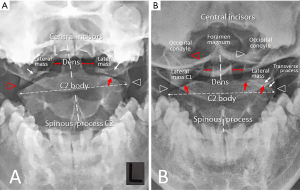
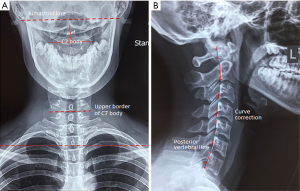
The patient presented to our clinic with guarded neck posture. The head was tilted to the right side and the chin was pulled to the left at rest. There was hypertonicity of the right sternocleidomastoid, right trapezius, and left splenius capitis, which was thought to be voluntary as it subsided when the patient was relaxed. No other areas of dystonic involvement were seen. Neck ROM was noted to be limited by pain to 0° extension (normal >60°), and 10° left rotation and 25° right rotation (normal >80°). The Soto-Hall test (approximating the chin to the chest) reproduced neck pain. Open mouth odontoid view (Figures 1,2A) demonstrated an asymmetry of the lateral atlantodental intervals and an offset of the C1 relative to the C2, which were suggestive of a rotatory instability in this patient. MRI of the brain excluded intracranial causes of the problems. In the absence of significant medical history and red flags, the subjective findings of this case report were consistent with an isolated CD and a probable atlantoaxial subluxation.
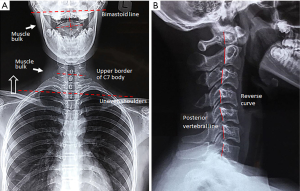
The patient underwent chiropractic treatment consisting of thermal ultrasound therapy, gentle massage and muscle mobilization with a daily frequency for 5 days. Heating pad was also encouraged for home use. She reported a significant relief of the neck pain and spasm after the first week. A light force cervical adjustment was added to restore the neck mobility during the following session 3 times a week for next 3 months. For subsequent 3 months, treatment sessions were reduced to twice a week to further normalize the head position. As a result of this treatment (Figures 2B,3), the postural and rotating symptoms were reduced. Furthermore, muscular hypertrophy, pain, and headache recovered. The girl has now been symptom-free from the dystonia for 9 months after initiation of chiropractic care. She is very happy with her recovery and regained confidence and self-esteem.
Discussion
While the pathogenesis of CD remains unclear, recent studies demonstrated that the afferent (Ia) sensory information from the neck was misinterpreted in patients with CD. Abnormal proprioceptive information with a preserved tonic vibration reflex suggests a central cause rather than a disorder of peripheral origin (4). At muscular level, dystonia is triggered by abnormal firing, with prominent electromyography (EMG) bursts and co-contraction of agonist and antagonist. This abnormal activation is asymmetric side-to-side most of the time, resulting in prominent asymmetric head/neck/shoulder position and muscle hypertrophy (5). A reduction of electrical resistance was observed in dystonic/hypertrophic muscles of CD patients, it is likely due to greater muscle size allowing a lower resistance for current flow on EMG (5). The diagnostic process for CD is guided by clinical examination, a detailed history, and knowledge of the disorder.
CD is a neurological condition. However, as illustrated in our case, some non-neurological conditions are relevant to and mimic CD. These problems often require additional interventions or other treatments. Repetitive contractions result in greater shearing forces and bending movement of the cervical structures. Approximately 60% of the neck rotation is from the atlantoaxial (C1–C2) joint combined with the horizontal C1–C2 facet joint alignment. Repetitive strain injury predisposes the cervical vertebrae to biomechanical changes and contributes to the development of C1–C2 subluxation (6). The horizontal orientation of the facet joints along with the relative ligamentous laxity in growing children also predisposes the cervical joints to hypermobility. An open-mouth odontoid radiograph is useful in evaluating the C1–C2 relationship. A shift of the odontoid to one side relative to the lateral masses of C1 (Figure 2A) is sufficient to make a diagnosis of C1–C2 subluxation (7). Treatment of dystonia through local injections of botulinum toxin clearly reduces pain in most patients with isolated dystonia (8), but it is incapable of treating C1–C2 subluxation. The chiropractic approach includes providing therapeutic effects for the tight musculature, joint mobilization for pain relief, and strengthening exercises for structure stabilization (9). These biomechanical responses are believed to be linked to clinical effects in treating spinal subluxation (10). The strength of this case is that it demonstrated an unexpected complication of CD and the treatment plan was individualized to the needs of the patient. Limitations such as the very small sample size and retrospective reporting require more such cases being reported.
Conclusions
CD can cause shearing forces of the cervical structures and predispose the upper cervical joint to unstable changes. Atlantoaxial subluxation can present with similar symptoms and be ignored. An index of suspicion should be maintained for this debilitating complication.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr.2020.03.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the guardian of the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Albanese A, Bhatia K, Bressman SB, et al. Phenomenology and classification of dystonia: a consensus update. Mov Disord 2013;28:863-73. [Crossref] [PubMed]
- Albanese A, Di Giovanni M, Lalli S. Dystonia: diagnosis and management. Eur J Neurol 2019;26:5-17. [Crossref] [PubMed]
- Mittal SO, Lenka A, Jankovic J. Cervical dystonia: an update on therapeutics. Expert Opin Orphan Drugs 2019;7:199-209. [Crossref]
- Avanzino L, Fiorio M. Proprioceptive dysfunction in focal dystonia: from experimental evidence to rehabilitation strategies. Front Hum Neurosci 2014;8:1000. [Crossref] [PubMed]
- Lungu C, Tarulli AW, Tarsy D, et al. Quantifying muscle asymmetries in cervical dystonia with electrical impedance: a preliminary assessment. Clin Neurophysiol 2011;122:1027-31. [Crossref] [PubMed]
- Ghanem I, El Hage S, Rachkidi R, et al. Pediatric cervical spine instability. J Child Orthop 2008;2:71-84. [Crossref] [PubMed]
- Ciftdemir M, Copuroğlu C, Ozcan M, et al. Non-operative treatment in children and adolescents with atlantoaxial rotatory subluxation. Balkan Med J 2012;29:277-80. [PubMed]
- Novaretti N, Cunha ALN, Bezerra TC, et al. The prevalence and correlation of non-motor symptoms in adult patients with idiopathic focal or segmental dystonia. Tremor Other Hyperkinet Mov (N Y) 2019;9:596. [PubMed]
- Marchand AA, Wong JJ. Conservative management of idiopathic anterior atlantoaxial subluxation without neurological deficits in an 83-year-old female: a case report. J Can Chiropr Assoc 2014;58:76-84. [PubMed]
- Pagé I, Descarreaux M. Effects of spinal manipulative therapy biomechanical parameters on clinical and biomechanical outcomes of participants with chronic thoracic pain: a randomized controlled experimental trial. BMC Musculoskelet Disord 2019;20:29. [Crossref] [PubMed]
Cite this article as: Chu EC, Lo FS, Bhaumik A. Secondary atlantoaxial subluxation in isolated cervical dystonia—a case report. AME Case Rep 2020;4:9.


