
Combined single-port transmediastinal and laparoscopic access with CO2 insufflation for esophageal resection: a case report on a canine model
Introduction
Esophageal cancer surgery, open or video-assisted, requires access to the chest, and thus may result in postoperative complications such as pain, atelectasis, pulmonary infection, pleural effusion and even respiratory dysfunction (1). Transmediastinal esophagectomy can effectively reduce these respiratory complications (2,3). Single-port mediastinoscopy with the use of CO2, combined with laparoscopy has been used in recent years (4-7). However, while thoracic surgeons are familiar with the dissection of the esophagus through a transthoracic approach, they could face difficulties through a single transmediastinal access (8). As part of our familiarization with the technique, we performed single-port transmediastinal esophagectomy in canines. Herein we report our experience with this technique.
Experimental process
Time: 2017.08.11.
Location: Covidien Animal Laboratory, Department of Surgery, Shanghai.
Experimental animal and batch number: male labrador, 28 kg, batch number: SYXK(Shanghai)2015-0009.
- Position: supine, shoulders up, head back. Anesthesia: single -lumen endotracheal intubation;
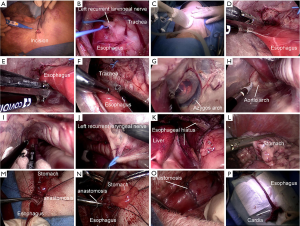
- Incision: a 4-cm incision along the anterior border of the sternocleidomastoid muscle was made (Figure 1A). Standard dissection of the cervical esophagus was conducted. The longitudinal muscle down the left side of the posterior esophagus, marks the left recurrent laryngeal nerve (RLN) (Figure 1B);
- A wound protector was placed and covered with a glove in order to seal the incision. Three fingers of the glove were incised, and a trocar was inserted into each one of them (one for a 10-mm Storz camera, and the rest for instruments such as ordinary forceps for cavity lens, Maryland knife of Covidien) and airtightly secured with a suture (Figure 1C);
- CO2 was insufflated into the mediastinum up to a pressure of 10 mmHg. The esophagus was dissected up to the level of the lower pulmonary vein. The left laryngeal nerve and subcarinal lymph nodes (LNs) were also dissected. We separate the esophagus in the following order:
- Dissection of the left side of the esophagus (Figure 1D);
- Dissection of the posterior side of the esophagus (Figure 1E);
- Dissection of the anterior side of the esophagus (Figure 1F);
- Dissection of the right side of the esophagus and the right side of the pleura and the azygos arch (Figure 1G);
- Exposure of the aortic arch and right brachiocephalic artery (Figure 1H);
- Exposure of the lower trachea and carina, and place the esophageal band as the mark in order to meet the lower esophagus with laparoscopic dissociation (Figure 1I);
- Dissection of the left RLN (Figure 1J).
- Abdominal part: standard laparoscopy was used to dissect the stomach up to the distal mediastinal part of the esophagus through the diaphragmatic crura (Figure 1K). And connect the interspace of upper and distal parts of mediastinum;
- Dissection of the stomach and construction of the gastric (tube) in the peritoneal cavity (Figure 1L);
- The gastric tube was pulled to the neck, through the posterior mediastinum. A hand-sewn end-to-end anastomosis between the proximal cervical esophagus and the gastric tube was constructed (Figure 1M,N,O);
- The specimen removed (most of the esophagus and cardia and lesser curvature of the stomach) were cut (Figure 1P).
Discussion
Single-hole transmediastinal laparoscopic combined approach has gradually become a research hot spot in esophageal surgery since 2015 by Fujiwara et al. (7) reported. At first, this method had strict indications for tumor size, and generally required patients with T1 or T2 tumor, no obvious lesion invasion, and no obvious mediastinal LN enlargement. However, with the development of technology and the popularization of clinical practice, the indications gradually expand. Fujiwara et al. (6) reported pretreatment diagnoses of patients were stage I, 19; II, 13; III, 24; IV, 4. Jin et al. (5) has reported the application of mediastinoscopy combined with laparoscopy treatment of two cases of IIIb and seven patients with IIIa, but he was also put forward a not have apparent LN enlargement. Tokairin et al. (4) also reported using this method in patients with stage IIIb esophageal cancer.
Compared with thoracoscopic combined laparoscopic esophageal cancer surgery, the biggest advantage of this operation method is that no incision is made in the chest and no interference to the chest. Besides, the azygos arch, bronchial artery, and heart plexus and lung plexus of vagus nerve are preserved, so the incidence of postoperative cardiopulmonary complications in transmediastinal esophagectomy is minimized, thus expanding the indications for surgery, especially for elderly patients and patients with cardiopulmonary comorbidities. Jin et al. (5) put forward it was beneficial to patients with poor pulmonary function. In transthoracic esophagectomy, pleural adhesion can make the operation difficult. However, via the transmediastinal approach pleural adhesions can prevent a pneumothorax in case the parietal pleura is accidentally incised. Therefore, instead of making mediastinoscopy difficult, pleural adhesion may make surgery easier to some extent.
The injection of CO2 into the mediastinum makes the surgical field clearer, thus making the separation of esophagus easier and safer. Important structures such as left RLN, thoracic duct and azygos vein should be avoided during operation. Azygos and bronchial arteries in particular, once damaged, can cause bleeding that is difficult to stop. In order to avoid intraoperative bleeding, the following should be followed. First, esophageal dissociation follows this sequence: this sequence makes it easier to identify these important tissues and avoid damaging them. Second, the Maryland energy devices are required to separate the tissues. Compared with other energy devices, Maryland’s thermal insulation device can avoid damaging blood vessels and other important tissues. Thirdly, once intraoperative bleeding occurs, small gauze strips can be used to compress and stop the bleeding, and the bleeding can be performed in lateral position after thoracotomy. Finally, the anesthesiologist had better ventilate with double-cavity endotracheal intubation to facilitate thoracotomy for hemostasis after bleeding.
The insufflation of CO2 in to the mediastinum enlarged the surgical space, which was helpful to fully expose the left RLN, para-esophageal, subcarinal and mediastinal LNs, making it easier to remove them. Compared with thoracoscopic combined laparoscopic esophagectomy, this procedure can fully expose the left RLN. It is difficult to expose the left RLN in the cervicothoracic junction by thoracoscopic combined with laparoscopic esophagectomy. However, inflatable mediastinoscopy combined with laparoscopic esophagectomy cannot remove the right recurrent laryngeal paraspinal LN in the mediastinum, which often requires an additional incision on the right side of the neck to remove the right recurrent laryngeal paraspinal LN. Tokairin et al. (4) reported the bilateral cervical nodes were additionally dissected by the open method. Wang et al. (9) reported less dissected LNs were detected in the inflatable mediastinoscopy group (12.2±5.4 vs. 16.8±5.8, P=0.044) than in the Ivor Lewis group. Jin et al. (5) reported that during mediastinal LN dissection, the number of right RLN LNs under mediastinoscopy was significantly less than that under thoracoscopy (P<0.05). However, Li et al. (10) reported that the transcervical inflatable mediastinoscopy esophagectomy had more LN dissection than the right thoracic esophagectomy.
There is no doubt that the operation of the transcervical inflatable mediastinoscopy esophagectomy is significantly more difficult than that of thoracoscopic esophagectomy. First of all, the thoracic inlet through the upper margin of the manubrium sternum is very narrow, which results in all instruments entering the mediastinum being crowded and interfering with each other. Second, despite the carbon dioxide filling, the space of the mediastinum is much smaller than the thoracic cavity, and the separation of the esophagus is more difficult, especially the right side of the esophagus and the adhesion with the left main bronchus. Thirdly, once there is a small hemorrhage in the operation, the anatomical space will be unclear, resulting in increased operational difficulties behind, and once there is a large hemorrhage, it is very difficult to deal with, often to change the lateral position through thoracic surgery to stop the bleeding.
Anatomical differences between dogs and humans may lead to some surgical differences. First of all, the mediastinal pleura of the dog is not complete, left and right thoracic coherence. These can lead to intraoperative pneumothorax, which can lead to airway hypertension during mechanical ventilation. In addition, the large circular ligaments of the liver in the experimental animals may hinder the dissection of the hiatus. To facilitate surgery, the circular ligament of the liver must be removed before dissecting the hiatus. Carefully retract the left lobe of the liver with a fan liver retractor under laparoscope. Thirdly, when dissecting the lower mediastinal esophagus through the hiatus, it is easy to open the left and right mediastinal pleura and enter the left and right thoracic cavity.
Conclusions
Combined single-port transmediastinal and laparoscopic access with the CO2 insufflation is an alternative approach for esophagectomy with certain advantages compared to transthoracic approach. Animal models can help the surgeon get familiar with a certain procedure before operating on a human.
Acknowledgments
Funding: This study was supported by the Nature and Science Fund of Key Cultivate Program from Wannan Medical College, CN (grant No. WK2018ZF06); the Science Research Fund for Talent Introduction of Yijishan Hospital, CN (grant No. YR201806); the Science Fund for Key Program of Three Creative Research of Yijishan Hospital, CN (grant No. Z1810).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by Minutes of meeting of the animal welfare and ethics committee at Medtronic clinical training centre (MIC) (Protocol Date: 20170705). All surgery was performed under sodium pentobarbital anesthesia, and all efforts were made to minimize suffering. The experimental dog was euthanized and buried after the experiment.
References
- Oshikiri T, Takiguchi G, Miura S, et al. Current status of minimally invasive esophagectomy for esophageal cancer: Is it truly less invasive? Ann Gastroenterol Surg 2018;3:138-45. [Crossref] [PubMed]
- Nakauchi M, Uyama I, Suda K, et al. Robot-assisted mediastinoscopic esophagectomy for esophageal cancer: the first clinical series. Esophagus 2019;16:85-92. [Crossref] [PubMed]
- Mori K, Aikou S, Yagi K, et al. Technical details of video-assisted transcervical mediastinal dissection for esophageal cancer and its perioperative outcome. Ann Gastroenterol Surg 2017;1:232-7. [Crossref] [PubMed]
- Tokairin Y, Nakajima Y, Kawada K, et al. A feasibility study of mediastinoscopic radical esophagectomy for thoracic esophageal cancer from the viewpoint of the dissected mediastinal lymph nodes validated with thoracoscopic procedure: a prospective clinical trial. Esophagus 2019;16:214-9. [Crossref] [PubMed]
- Jin Y, Lu X, Xue L, et al. Retrospective Comparison of Two Minimally Invasive Esophagectomy in the Treatment of Esophageal Cancer: Pneumatic Mediastinoscopy Versus Thoracoscopy. J Laparoendosc Adv Surg Tech A 2018. [Epub ahead of print]. [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Perioperative outcomes of single-port mediastinoscope-assisted transhiatal esophagectomy for thoracic esophageal cancer. Dis Esophagus 2017;30:1-8. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Single-Port Mediastinoscopic Lymphadenectomy Along the Left Recurrent Laryngeal Nerve. Ann Thorac Surg 2015;100:1115-7. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Mediastinoscope and laparoscope-assisted esophagectomy. J Vis Surg 2016;2:125. [Crossref] [PubMed]
- Wang J, Wei N, Lu Y, et al. Mediastinoscopy-assisted esophagectomy for T2 middle and lower thoracic esophageal squamous cell carcinoma patients. World J Surg Oncol 2018;16:58. [Crossref] [PubMed]
- Li X, Wang W, Zhou Y, et al. Efficacy comparison of transcervical video-assisted mediastinoscopic lymphadenectomy combined with left transthoracic esophagectomy versus right transthoracic esophagectomy for esophageal cancer treatment. World J Surg Oncol 2018;16:25. [Crossref] [PubMed]
Cite this article as: Zhu S, Yu S, Liu F. Combined single-port transmediastinal and laparoscopic access with CO2 insufflation for esophageal resection: a case report on a canine model. AME Case Rep 2020;4:6.


