
Interspinous endoscopic lumbar decompression: technical note
The lumbar laminectomy procedure is performed world-wide as an effective technique for decompressing the central spinal canal and bilateral foramina. In the minimally invasive tubular approach, a paramedian incision is made and sequential dilators are used until a typically 18–21 mm tubular retractor is inserted (1). The approach is typically a sub-spinous process approach to decompress the central canal, and the contralateral foramina is typically more easily decompressed than the ipsilateral foramina. Other versions of the minimally invasive tubular approach include a midline approach where the spinous process is first removed or split (2). One significant challenge of inserting a tubular retractor through the midline approach is the limited space between the spinous processes. Here, the authors describe a step-by-step approach on how to insert an 11.5 mm tubular retractor in the midline and perform a central and bilateral foraminal decompression with a working channel endoscope. The midline approach and midline anatomical point-of-view potentially make this minimally invasive approach more accessible to surgeons less comfortable with the anatomic visualization seen with the paramedian subspinous approach. The authors stress here the importance of reducing the tubular retractor size down from 18 to 11.5 mm: a critical diameter that allows it to be inserted between the spinous process without disrupting the interspinous ligament, facet capsule or multifidus attachments. These structures are often at risk during a tubular retractor decompression surgery.
Case presentation
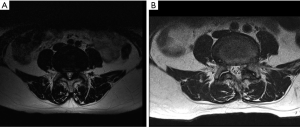
A 69-year-old male patient who presented with classic claudication symptoms and bilateral hip pain with walking, relieved with sitting, is presented. He had exhausted non-operative treatment that included physical therapy and epidural steroid injections. He requested awake endoscopic treatment for his lumbar 4–5 moderate central stenosis and severe lateral recess stenosis. Figure 1 demonstrates his pre-operative and post-operative MRI.
Operative technique
For the endoscopic laminectomy and bilateral foraminotomy procedure, the patient was positioned in the prone position on a Kambin frame with flexed hips and knees to produce kyphosis. The procedure was done with the patient awake with local anesthesia and intravenous sedation. The Joimax iLESSYS® Delta endoscope was used for the procedure. Anterior-posterior (AP) and lateral fluoroscopy were used intermittently throughout the case. The operative level was identified under AP and lateral fluoroscopy. A radio-opaque instrument was used to mark the skin in the midline under AP fluoroscopy. The target of the incision is the caudal 1/3 of the rostral spinous process of the operative level, in this case the L4 spinous process. This target is marked with the tip of the 11-gauge Jamshidi needle. A 10 mm vertical incision is made with a #15 blade. Under AP fluoroscopic guidance, the Jamshidi needle is inserted into the spinous process with the aid of a mallet until it is firmly seated. The direction of the needle is checked under AP fluoroscopy to maintain its position within the midline so that it remains within the confines of the spinous process. The needle is advanced slowly under lateral fluoroscopy with the mallet taking care to maintain its trajectory in the midline. Multiple fluoroscopic images are required to advance the needle to the level of the inferior articular facet. An imaginary line along the inferior articular facet marks the inferior boundary for advancing the Jamshidi needle. Once at the level of the inferior articular facet, a blunt tipped guidewire was introduced, taking care that the guidewire did not advance into the canal. The Jamshidi needle was removed and a 3 mm guide tube (Figure 2A) then 4 mm crown reamer was used under fluoroscopic guidance to create a small channel through the caudal aspect of the rostral spinous process. Care was taken to respect the border of the inferior articular line so as not to enter the canal.
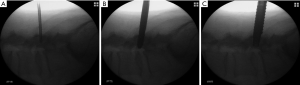
The reamer was removed, and the channel serially widened with the use of progressively larger side cutting manual drills that increase in size up to a final diameter of 9.5 mm (Figure 2B). These manual drills have a blunt tip which protects the dura.
The final diameter of the channel created by the drill is just large enough for the 11.5 mm tubular retractor to be inserted to the inferior articular line under fluoroscopic guidance (Figure 2C). The 1 cm diameter working channel endoscope with a 6 mm working channel was then inserted. The ligamentum flavum was then visible. The endoscopic drill was then used to complete the inferior laminectomy at L4 while the ligamentum flavum was intact.
The endoscopic grasper was used to remove a portion of the midline ligamentum flavum (Figure 3A) exposing the dura. Continuous irrigation and a ball probe were helpful in creating a safe plane between the dura and ligamentum flavum. The Kerrison punch was then used to open and remove the ligamentum flavum and perform bilateral lateral recess decompressions and remove the superior portion of the L5 lamina (Figure 3B,C,D).
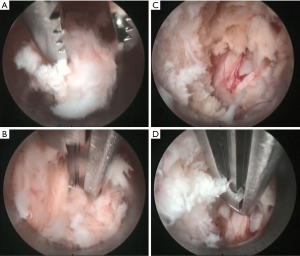
Since the incision and placement of the endoscope and tubular retractor are in the midline, one must simply rotate the retractor and tube to the face the desired lateral recess. The cranial to caudal decompression was achieved by “wanding” the retractor tube. Since the spinous processes are held together by the interspinous ligament, there was some flexibility that allowed the surgeon to angle the tubular retractor as necessary.
The surgical goal of lateral recess decompression is the same as that with open surgery and the endpoint of surgery is to visually inspect the exiting and traversing roots and verify that there is no further compression. Epidural venous bleeding was controlled with bipolar electro-cautery. Once the decompression was completed, the cannulated tubular retractor and endoscope were removed, pressure was held on the incision for 5 min, and the wound was closed with a subcutaneous suture and glue.
Postoperative course
The postoperative course for the patient was uneventful; he had immediate resolution of his claudication and radicular symptoms. Six months, 1- and 2-year after his endoscopic procedure, the patient had no clinical symptoms related to the L4-5 compression.
Discussion
The hallmark of degenerative lumbar spine disease is a loss of disc height and bulging of the lumbar disc and overgrowth of the ligamentum flavum and facet tissue that leads to central and lateral recess stenosis. Treatment paradigms include direct decompressions and indirect decompressions (expanding the disc space with fusion devices or expanding the interspinous distance with interspinous distractors). A direct decompression of the central canal and lateral recess can be performed through a midline approach using standard or tubular retractors or through a paramedian approach through a tubular retractor through a subspinous process trajectory that spares the midline tension band (1). A midline spinous process splitting approach has also been proposed that restores the midline tension band by re-approximating the split spinous processes after the central and lateral recess decompression (2). Multiple authors have described endoscopic approaches to treating lumbar stenosis but these have not been widely adopted by most spine surgeons probably because of unfamiliarity most surgeon have to endoscopic approaches, targeting and visualization (3-7).
The procedure demonstrated here allows the spine surgeon with traditional laminectomy experience to transition immediately to a minimally invasive endoscopic laminectomy procedure that is simple and presents the surgeon with the same anatomy that would be seen during a standard midline approach seen through loupes or a microscope. The advantages, moreover, are, (I) that the incision is so small, the procedure can be performed awake, and (II) the tubular retractor placement is directly midline but does not require taking down the ligaments or muscle attachments to the spinous process thereby preserving the midline tension band. A midline interspinous endoscopic treatment approach is possible today due to advances in endoscopic spine surgery technology that include high-definition endoscopic cameras, endoscopic drills and reamers, and endoscopic graspers and Kerrison rongeurs.
The proposed interspinous endoscopic laminectomy does come with several disadvantages. One, the working channel endoscopic approach is a “one-instrument-at-a-time” approach, meaning, the surgeon doesn’t have an assistant with a second instrument to create a plan between the ligamentum flavum and the dura while the surgeon removes ligamentum with a Kerrison. The continuous irrigation is often considered, however, to act as the second instrument because it pushes the dura away while the surgeon removes ligamentum. Second, a dural tear during endoscopic decompression cannot be easily repaired. The surgeon must consider patching the tear or converting to a more open approach to directly close the tear, which is not simple given that the patient is awake.
Minimally invasive endoscopic spine surgery offers many benefits that are attractive to patients: shorter recovery times, small incisions, and less pain. The authors present this technical note for others to consider as a possible minimally invasive solution for the treatment lumbar stenosis.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patient for publication of this Case report and accompanying images
References
- Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 1999;7:e5. [Crossref] [PubMed]
- Watanabe K, Hosoya T, Shiraishi T, et al. Lumbar spinous process-splitting laminectomy for lumbar canal stenosis. Technical note. J Neurosurg Spine 2005;3:405-8. [Crossref] [PubMed]
- Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 2015;18:61-70. [PubMed]
- Ruetten S, Komp M, Merk H, et al. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 2009;10:476-85. [Crossref] [PubMed]
- Soliman HM. Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J 2015;15:2282-9. [Crossref] [PubMed]
- Torudom Y, Dilokhuttakarn T. Two Portal Percutaneous Endoscopic Decompression for Lumbar Spinal Stenosis: Preliminary Study. Asian Spine J 2016;10:335-42. [Crossref] [PubMed]
- Wagner R, Telfeian AE, Krzok G, et al. Fully-endoscopic lumbar laminectomy for central and lateral recess stenosis: Technical note. Interdiscip Neurosurg 2018;13:6-9. [Crossref]
Cite this article as: Houle P, Telfeian AE, Wagner R, Bae J. Interspinous endoscopic lumbar decompression: technical note. AME Case Rep 2019;3:40.


