
Rare radiculopathy from an osteochondral loose body: a case report and literature review
Introduction
Lumbar radiculopathy can lead to back and leg pain. Low back pain (LBP) is a common condition and affects up to 90% of the population at some point in their lives (1). The prevalence of lumbosacral radiculopathy is between 3% to 5% of the population (2). The most common aetiology of lumbar radiculopathy is nerve root compression caused by disc herniation. Loose bodies in the spinal canal are extremely rare with only 5 cases reported previously (3-7). Three cases occurred in the lumbar spine and two have been reported in the cervical spine. All previously reported cases were located centrally in the canal causing central canal stenosis. This is the first reported case to occur in the foramen.
Case presentation
A 48-year-old woman presented with a 7-year history of progressive right-sided sciatica. The pain radiated in a right L5 distribution with constant parasthesia described as an “electric” sensation. She also described an intermittent severe “grabbing pain” in the midline of her lower lumbar spine exacerbated by movement. She had presented to the emergency department (ED) on several occasions. Her past medical history was unremarkable apart from a body mass index (BMI) over 30 kg/m2.
On examination the patient had an antalgic gait. Lower limb neurological examination was normal.
She had seen other spine surgeons and had several lumbar spine magnetic resonance imagings (MRIs), outlining a degenerative disc at L5–S1 extending into the right L5–S1 foramen potentially irritating but not compressing the L5 nerve root.
She had undergone extensive investigations trying to ascertain the source of pain. She had been given a diagnosis of piriformis syndrome based on a sciatic nerve ultrasound. Gluteal tendinopathy had been considered and an MRI hip showed trochanteric and subgluteal bursitis.
Lack of improvement following several steroid injections into the hip joint and lumbar spine lead the patient to seek further referral.
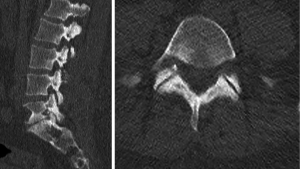
An updated lumbar MRI showed significant disc degeneration at L5–S1 with loss of disc height but no nerve compression. The right L5–S1 foramen was narrowed with indentation of the right L5 nerve root posteriorly in the foramen (Figure 1). This appeared to be due to thickened ligament/joint capsule from a moderate facet joint arthropathy.

A minimally invasive right L5 nerve root decompression was performed through a midline incision. The right L5 nerve root was exposed in the lateral recess and decompression 14 mm along the nerve root was performed. A loose osteochondral fragment was found in the foramen and removed. It measured 5 mm × 4 mm × 3 mm (Figure 2). The fragment caused severe compression of the nerve root and had eroded the perineurium due to chronic compression. Once the fragment was removed the nerve root was freely mobile. She reported immediate resolution of the sciatic pain post operatively.
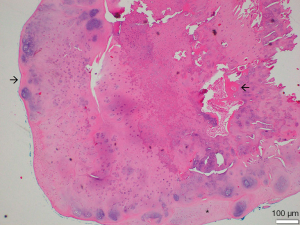
Histopathological examination revealed a benign cartilaginous nodule with central areas of bone formation (Figure 3). The surface of the nodule was smooth. The subsurface stroma included areas of cartilage as well as areas that appeared to be transitional between synovial tissue, with several layers of fibroblast like cells, and cartilage. It was postulated, therefore, that the cartilaginous nodule could have arisen due to metaplastic transition of synovium into cartilaginous and bony tissue.
Discussion
Osseous loose bodies in synovial joints are presumed to arise from trauma, joint degeneration or synovial proliferation (4). They are usually seen in synovial joints such as the knee and hip and most commonly arise from the articular surfaces of the bone (4). Single loose bodies in the spinal canal are extremely rare with only four cases reported to date; two in the lumbar and two in the cervical spine (3,5-7). A fifth case reported of multiple osseous loose bodies in association with an isthmic spondylolisthesis has also been reported (4). In all cases the lesions caused central stenosis. Our case is unique as the osteochondral loose body caused unilateral sciatica due to compression of the L5 nerve root in the foramen.
Histopathological analysis of our case revealed a benign cartilaginous nodule with central areas of bone formation. Subsurface stroma displayed areas of cartilage as well as tissue transitioning between synovium, fibroblastic cells, and cartilage (Figure 3). Therefore, we postulate that the cartilaginous nodule could have arisen due to metaplastic transition of synovium into cartilaginous and bony tissue.
The differential diagnosis for single loose bodies includes osteochondroma, synovial osteochondromatosis and osseous loose body (4).
Osteochondromas are the most common benign tumours of the long bones and the skeleton (8). Most cases occur in young adults (8). Involvement of the spine is rare with isolated cases of cord compression reported. The lesions generally arise from the neural arch not from the facet joint as in our case. The histology of our case with mature bone with a smooth cartilaginous cap could be considered consistent with an Osteochondroma but with the presence of synovial tissue in the lesion imply it has arisen from the joint rather than from mature trabecular bone.
Primary synovial chondromatosis, also called Reichel syndrome is a very rare benign idiopathic disease affecting the lining of articular surfaces of synovial joints (9,10). It is characterized by the presence of multiple cartilaginous or osteocartilaginous nodules in the synovium floating in the joint space (6,10). It usually causes mono-articular pathology. The exact pathogenesis is unknown, but it is suggested that synovium undergoes cartilage metaplasia (6). The synovium grows abnormally and produces small nodules of cartilage which may ossify (6). It usually affects the large joints such as the knee, or less commonly the hip, elbow, wrist, ankle and the shoulder joint (10). The condition is extremely rare with only two cases reported in the literature previously (9,10). As our case only had a single loose body in a joint with established arthritic degeneration primary synovial osteochondromatosis is very unlikely.
Chronic intra-articular loose bodies are generally composed of cartilage alone or cartilage and bone and are usually found in the larger knee or hip joints. They result from any process that causes damage to the articular surface. They are often designated as secondary synovial osteochondromatosis. They have been documented in osteoarthritis, avascular necrosis, osteonecrosis and osteochondritis dissecans (6). They arise from the growth of separated particles from the articular cartilage or osteophytes or osteophytes from the degenerative joint. These bodies show uniform chondrocytes with annular calcification surrounding the core tissue (4). The loose bodies cause locking, damage or irritation to local structures. There is no uniform radiographic or MRI appearance as the loose body may not be detected in up to 30% of cases, just as in our case (11).
Tambe et al. reported the first case of an osteochondral loose body in the lumbar spine in 2002 (3). A 68-year-old man presented with progressive neurogenic claudication (3). MRI revealed severe posterior central stenosis with no evidence of disc protrusion or synovial cysts (3). Similarly, in our case the authors did not appreciate the loose body until surgery when the loose body became evident underneath the ligamentum flavum. The fragment Tambe described was histopathologically similar to our case with trabecular bone centrally covered by surface layers of cartilage (3). The authors termed it a “Spinolith” and were unable to identify a source for the lesion (3). The loose body was 9 mm × 5 mm × 2 mm in size. In our case the loose body was lying in the foramen, not centrally in the canal.
Treon et al. also described a single osteochondral lesion causing lumbar canal stenosis in a 64-year-old female with neurogenic claudication (5). Imaging showed a grade 1 L3–4 degenerative spondylolisthesis with significant central stenosis (5). During surgery she was found to have a freely mobile L3 spinous process and large osteochondral fragment in her spinal canal (5). The authors postulated that facet joint hypertrophy was the locus of the fragment however they felt it may have arisen from the mobile spinous process (5). The lateral location of the lesion in our case in the foramen adjacent to the facet joint makes it almost certain the fragment arose from the anterior aspect of the facet joint. The lesion was wedged in the foramen and could not have arisen from the midline structures as it could not have migrated through the foramen. It was delivered into the central canal only after significant bone had been removed medially.
The exact origin of the loose body in our case remains obscure. In our case the location lying posterior to the nerve in the foramen makes it impossible to represent a simple calcified disc fragment. Degenerated intervertebral discs possess osteogenic potential in direct relation to the severity of degeneration. Takeshima et al. reported a case of isthmic spondylolisthesis with multiple loose bodies causing central canal stenosis in a 74-year-old male (4). The authors hypothesised that long-standing dynamic instability induced by lumbar isthmic spondylolisthesis may facilitate the formation of the multiple loose bodies (4). Ossification of the ligamentum flavum can occur however in our case the lesion revealed trabecular bone surrounded by cartilage without any connection to ligamentum flavum.
These two previous cases highlight the usefulness of computed tomography (CT) scans in cases of lumbar spine pathology. In all three cases of single lose body in the lumbar spine the lesions were not seen on the pre-operative MRI scan. In our case the loose body was best visualized in retrospect from the localising CT scan performed as part of the technetium bone scan but this was not appreciated as it was not a diagnostic quality CT scan and was not assessed as such (Figure 4). If this had been performed the lesion could have been diagnosed at a much earlier stage.
Our case is unique as it is only the third case reported of a single loose body in the lumbar spine. It lay laterally in the foramen not in the centre of the canal as was found in previous cases.
Conclusions
We present the first case of an intra-foraminal osteochondral loose body as a cause of radiculopathy. This is the fourth reported case of loose bodies in the lumbar spine. Spine surgeons should consider diagnostic CT as well as MRI in cases of foraminal stenosis to assess the source of compression.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ 2015;350:h1748. [Crossref] [PubMed]
- Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin 2007;25:387-405. [Crossref] [PubMed]
- Tambe A, Monk J, Calthorpe D. "Spinolith": case report of a loose body in the spinal canal. Spine (Phila Pa 1976) 2002;27:E248-9. [Crossref] [PubMed]
- Takeshima Y, Hanakita J, Takahashi T, et al. Multiple Osseous Loose Bodies Associated with Lumbar Isthmic Spondylolisthesis. World Neurosurg 2016;95:623.e1-623.e4. [Crossref] [PubMed]
- Treon K, Ockendon M. Osteochondral loose body: an unusual cause of lumbar spinal stenosis. Eur Spine J 2017;26:167-9. [Crossref] [PubMed]
- Hongo M, Miyakoshi N, Kasukawa Y, et al. Enlargement of an osseous loose body in the cervical spine with cord compression. Spine J 2009;9:e11-4. [Crossref] [PubMed]
- Shin C, Nourbakhsh A, Ozkan E, et al. Asymptomatic osseous loose body in the cervical spine. A case report. J Bone Joint Surg Am 2007;89:1586-8. [Crossref] [PubMed]
- Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46. [PubMed]
- Wahab H, Hasan O, Habib A, et al. Arthroscopic removal of loose bodies in synovial chondromatosis of shoulder joint, unusual location of rare disease: A case report and literature review. Ann Med Surg (Lond) 2018;37:25-9. [Crossref] [PubMed]
- Tahmasebi MN, Bashti K, Sobhan M, et al. Bilateral Synovial Knee Chondromatosis in a Patient with Rheumatoid Arthritis: Case-report and Literature Review. Arch Bone Jt Surg 2014;2:260-4. [PubMed]
- Fischer M, Mödder G. Radionuclide therapy of inflammatory joint diseases. Nucl Med Commun 2002;23:829-31. [Crossref] [PubMed]
Cite this article as: Whittaker B, Frydenberg E, Earls P, Wang D, Steel T. Rare radiculopathy from an osteochondral loose body: a case report and literature review. AME Case Rep 2019;3:38.



