
Classic Hodgkin lymphoma with initial extranodal osseous presentation: a case report and literature review
Introduction
Classic Hodgkin lymphoma (CHL) accounts for 95% of all HL cases with bone marrow involvement occurring in 5% of all CHL cases (1). On the other hand, extranodal forms of HL are rare, accounting for <1% of all HL cases with the most common locations being the digestive tract, lungs, central nervous system and bone (2,3).
The initial presentation of classic Hodgkin lymphoma in a pediatric population typically consists of lymphadenopathy, fever, night sweats and weight loss. Extranodal osseous lesions are rarely seen at the time of diagnosis with only a handful of cases described in the literature.
Case presentation
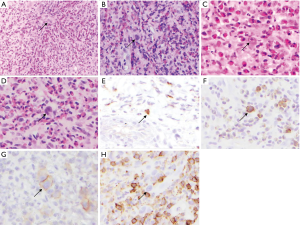
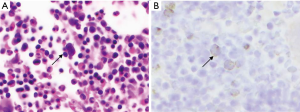
The present study describes a case of HL with initial extranodal osseous presentation in an 11-year-old male. The patient presented with 5 months of severe pain in the lumbar-sacral region with radiation to both lateral areas of the legs, without any substantial neurological deficits, fever or weight loss. Red blood cell count was normal, and further examination revealed cervical lymphadenopathy. Radiological evaluation detected a lytic lesion in L5 vertebral body and right iliac bone, extending to both psoas muscles (Figure 1). Pathological evaluation included biopsy of the L5 lesion (Figure 2) which showed a prominent vascular component, scattered Reed-Sternberger (RS) cells with prominent nucleoli, and a heavy eosinophilic infiltrate. The staging bone marrow biopsy showed involvement by HL (Figure 3).

Discussion
The Lugano staging system is the most current lymphoma staging classification system which was derived in 2011 from the Cotswolds-modified Ann Arbor classification system. Based on this classification, stage IV is defined as: “diffuse or disseminated involvement of at least one extranodal organ with or without associated lymph node involvement” (4).
Extranodal osseous involvement in Hodgkin lymphoma is uncommon. Even in the late stages only 9% to 35% of cases have any bone involvement, and very rarely at the time of presentation (5) as in our case.
Kumar et al. (6) reported a case with a previous diagnosis of Hodgkin lymphoma that was successfully treated, but later presented with a solitary lytic bone lesion in the right upper humerus. Microscopic examination of the biopsy revealed classical binuclear and mononuclear RS cells in a lymphoplasmacytic background with admixed eosinophils, neutrophils and histiocytes. A diagnosis of extranodal osseous Hodgkin lymphoma was made with RS cells staining for CD15 and CD30.
Similar to Kumar et al. (6) Li et al. (7) and Li et al. (8) also reported two cases of extranodal osseous Hodgkin lymphoma who initially presented with a lytic lesion of the rib and sternum respectively.
In contrast to the cases reported of primary bone lymphoma reported by Kumar et al. (6) and Li et al. (7) where no other sites of involvement were found, Dogan et al. (5) described 49 cases of Hodgkin lymphoma with bone involvement reported at the time of initial diagnosis. The majority of these cases also had lymph nodes and other organ involvement with bone lesions at staging workup. With similar gender distribution, and the most common bones involved were from the axial skeleton: in our case, both right ilium and lumbar vertebrae were involved.
Sidharth et al. (9) conducted a study focusing on the pediatric population, whereby they staged 49 first-time-diagnosed patients younger than 18-year-old. Twenty-four percent of these patients presented initially with stage IV (advanced stage) and subsequently showed less satisfactory response to treatment. A much higher percentage was reported in another study by Sherief et al. (10) focusing on patients ranging from 3 to 14 years old whereby they noted that more than half of the patients (55.9%) had advanced disease at the time of diagnosis. On the other hand, Gaudio et al.’s, (11) study on patients with a median age of 41-year-old reported a percentage of only 8% of patients presenting initially with advanced disease. Based on these studies, there exists a significant difference in the proportion of pediatric versus adult patients presenting with advanced disease.
Radiologically, lytic lesions of bone represent a variety of conditions ranging from benign (including infections and bone cysts) to malignant neoplasms such as multiple myeloma and Hodgkin lymphoma. Based on our patient’s young age and radiologic findings the following entities, besides CHL, entered the differential diagnosis: epithelioid hemangioma of bone, Langerhans cell histiocytosis, osteomyelitis, ALCL, mastocytosis, acute myelomonocytic leukemia, and large B cell lymphomas (LBCL) including diffuse LBCL and T-cell/histiocyte-rich LBCL.
Epithelioid hemangioma of bone has been reported most commonly in the tubular bones of the extremities (12). Although recognized as a benign tumor by the WHO, it can display locally aggressive features. It manifests radiologically as an aggressive lytic lesion, usually involving the diaphysis of the long bones, pelvis, and scapula. It also can grow rapidly, with a disproportion between the very large soft tissue mass and the cortical destruction (13). Both Epithelioid hemangioma of bone and extranodal osseous Hodgkin lymphoma may present histologically with a lymphoplasmacytic infiltrate with heavily admixed histiocytic and eosinophilic background, prominent vascular component and reactive fibroblastic proliferation. However, the presence of RS cells determines the diagnosis of CHL. Consequently, a thorough and precise search for RS cells should be performed when encountered with a bone lesion with a richly vascularized mixed inflammatory background.
Langerhans cell histiocytosis also presents as a lytic mass that may possibly extend into soft tissue. Histologically, it shows a background composed of variable admixture of eosinophils, giant cells, neutrophils and Langerhans cells; which are easily distinguished from RS cells by their reniform nuclei, absence of prominent nucleoli and positivity for S100 and CD1a immunostains with absent CD30 staining.
Osteomyelitis may produce focal bone destruction with soft tissue permeation and can present with a heavy eosinophilic and lymphoplasmacytic background inflammation with associated bone destruction and stromal fibrosis; however, it lacks RS cells.
Anaplastic large cell lymphoma (ALCL) is a T cell lymphoma that usually presents in children and young adults, has common extranodal or bone marrow involvement, and is characterized by large hallmark cells with abundant cytoplasm that can have multiple wreath-like nuclei resembling Reed-Sternberg cells. The hallmark cells are usually positive for CD30, but unlike RS cells, they tend to express CD45, CD43, EMA and ALK (in ALK-positive ALCL) (14).
Although mastocytosis rarely presents as a skeletal disorder, in cases associated with bone marrow infiltration it can manifest as diffuse, poorly demarcated, sclerotic, and lucent areas involving the axial skeleton with associated lytic changes, osteopenia, osteonecrosis and bone destruction (15). Microscopically, mastocytosis presents as perivascular and peritrabecular condensation of compact foci of more than 15 mast cells within fibrohistiocytic matrix with absent RS cells.
Acute myelomonocytic leukemia requires the presence of myeloblasts, monoblasts and promonocytes as 20% or more of the nonerythroid cells in the blood or bone marrow (1). In our case, the patient’s CBC was normal and the bone marrow did not show any evidence of blasts.
Diffuse large B cell lymphoma (DLBCL) is more common in adults and is rarely associated with osseous or bone marrow involvement. It usually presents as a diffuse sheet-like proliferation of medium-sized to large lymphoid B-cells (1) some of which may mimic RS cells. Both the anaplastic variant and mediastinal subtype of DLBCL can express CD30; however, unlike RS cells they are usually positive for CD45, CD20, CD79a, CD75, Oct-2 and BOB-1.
T-cell/histiocyte-rich LBCL affects mainly middle-aged men, presents as a nodal disease with common bone marrow involvement, and is characterized by scattered single large B cells mimicking RS cells embedded in a background of small T cells and histiocytes. The large atypical B cells have a different immunophenotype than RS cells and usually express pan-B-cell markers including CD19, CD20, CD79a and Bcl-6 with negative expression for CD15 and CD30 (1).
Given the overlapping morphologic features among the aforementioned entities, the final diagnosis of extranodal osseous Hodgkin lymphoma will depend on the presence of Reed Sternberg cells and their positivity for CD15 and CD30 with negative expression for CD45, CD43, ALK, S100, CD1a and pan-B-cell markers.
In our case, the patient initially presented with a solitary bone lytic lesion of L5 vertebra and sacrum. Microscopic examination of the L5 bone biopsy showed a prominent vascular component, scattered large cells with prominent nucleoli and a heavy eosinophilic infiltrate, which raised the concern of extranodal osseous Hodgkin lymphoma given the patient’s age and the presence of cervical lymphadenopathy. Further immunohistochemical workup revealed that the large cells (Reed Sternberg cells) were positive for CD15, CD30 and Pax-5 supporting the diagnosis of classic Hodgkin lymphoma. Consequently, the patient underwent a bone marrow biopsy which also showed involvement by Hodgkin lymphoma and is currently completing chemotherapy regimen with promising results.
Conclusions
Hodgkin lymphoma presenting initially as a bone lesion is very uncommon and could be misleading, especially in the pediatric population. Clinicians should maintain a high suspicion for hematologic malignancies and pathological examination thorough immunohistochemical workup plays a vital role in establishing this challenging diagnosis.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The authors have obtained a written consent from the mother.
References
- Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues. Revised 4th edition. Lyon: WHO, 2017;2.
- Guermazi A, Brice P, de Kerviler EE, et al. Extranodal Hodgkin disease: spectrum of disease. Radiographics 2001;21:161-79. [Crossref] [PubMed]
- Zucca E. Extranodal lymphoma: a reappraisal. Ann Oncol 2008;19 Suppl 4:iv77-80. [Crossref] [PubMed]
- Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol 2014;32:3059-68. [Crossref] [PubMed]
- Köseoğlu RD, Senayli A, Biçakçi U, et al. Osseous presentation of Hodgkin's disease: a case report and review of the literature. Turk J Pediatr 2007;49:218-22. [PubMed]
- Kumar S, Ferns SJ, Bhat BV, et al. Hodgkins disease in relapse presenting as bone tumor. Indian Pediatr 2003;40:56-9. [PubMed]
- Li Y, Wang XB, Tian XY, et al. Unusual primary osseous Hodgkin lymphoma in rib with associated soft tissue mass: a case report and review of literature. Diagn Pathol 2012;7:64. [Crossref] [PubMed]
- Li Y, Qin Y, Zheng L, et al. Extranodal presentation of Hodgkin's lymphoma of the sternum: A case report and review of the literature. Oncol Lett 2018;15:2079-84. [PubMed]
- Totadri S, Radhakrishnan V, Ganesan TS, et al. Can Radiotherapy Be Omitted in Children With Hodgkin Lymphoma Who Achieve Metabolic Remission on Interim Positron Emission Tomography? Experience of a Tertiary Care Cancer Referral Center. J Glob Oncol 2018;4:1-7. [Crossref] [PubMed]
- Sherief LM, Elsafy UR, Abdelkhalek ER, et al. Hodgkin lymphoma in childhood: clinicopathological features and therapy outcome at 2 centers from a developing country. Medicine (Baltimore) 2015;94:e670. [Crossref] [PubMed]
- Gaudio F, Pedote P, Niccoli Asabella A, et al. Bone Involvement in Hodgkin's Lymphoma: Clinical Features and Outcome. Acta Haematol 2018;140:178-82. [Crossref] [PubMed]
- Boyaci B, Hornicek FJ, Nielsen GP, et al. Epithelioid hemangioma of the spine: a case series of six patients and review of the literature. Spine J 2013;13:e7-13. [Crossref] [PubMed]
- Ignacio EA, Palmer KM, Mathur SC, et al. Epithelioid hemangioendothelioma of the lower extremity. Radiographics 1999;19:531-7. [Crossref] [PubMed]
- Jaffe ES. Anaplastic large cell lymphoma: the shifting sands of diagnostic hematopathology. Mod Pathol 2001;14:219-28. [Crossref] [PubMed]
- Horny HP. Mastocytosis: an unusual clonal disorder of bone marrow-derived hematopoietic progenitor cells. Am J Clin Pathol 2009;132:438-47. [Crossref] [PubMed]
Cite this article as: Gomez M, Bem S, El-Zammar O, Naous R. Classic Hodgkin lymphoma with initial extranodal osseous presentation: a case report and literature review. AME Case Rep 2019;3:22.


