Juvenile ossifying fibroma in a Nigerian boy: a rare case report
Introduction
Juvenile ossifying fibroma (JOF) is defined as a fibro-osseous lesion that is characterized by cell rich fibrous tissues, bands of cellular osteoid trabeculae and giant cells (1-3). It presents in children younger than 15 years of age, behaves aggressively, and tends to recur (2,3). It is a variant of ossifying fibroma and also known as “aggressive”, “active” or “psammomatoid” ossifying fibroma (4). It is a benign condition that however invades into the local surrounding structures.
Unlike classical ossifying fibroma which is commoner in the third and fourth decade of life, JOF is very rare and only few cases have been reported (5-10). It commonly involves the paranasal sinuses, the orbit, the fronto-ethmoid bones and the maxilla, although affectation of the mandibular bone has also been documented (5,7,9). It has been reported to occasionally occur in areas of missing teeth (5). There is a slight male predominance and age ranges between 2 to 15 years (3,6). Recurrence which ranges from 30% to 58% has been suggested to be due to the presence of residuals after surgery in the maxillary sinus and orbital region.
JOF presents in similar fashion and often offers diagnostic dilemma with other clinical entities such as Burkitt lymphoma, fibrous dysplasia, aneurysmal bone cyst, osteoblastoma and osteosarcoma. Therefore a high index of suspicion is needed when reviewing a case of jaw mass so as to prevent misdiagnosis and therefore mismanagement of JOF as seen in this 7-year-old boy whose case report is outlined below.
Case presentation
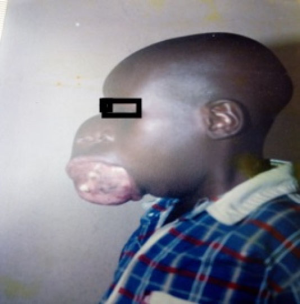
The patient is a 7-year-old boy, whose caregiver belongs to a low socioeconomic class, presented to our oncology unit with a rapidly enlarging right jaw mass. The mass progressively increased in size distorting the adjacent structures such as the nose, ear and eyes. There was also exposure of the buccal mucosa and teeth loss. There was associated noisy breathing. There was no swelling in other parts of the body and vision was still preserved in the affected part.
Clinical examination
Examination findings showed an underweight boy with a huge facial mass extending from the right infraorbital region superiorly to the jaw with exposure of the buccal mucosa and gum with just few teeth. There was upward and lateral displacement of the right eye, proptosis and hypertelorism. The mass also extended laterally distorting the right ear, and in the midline, there was displacement of the right nose, almost obliterating the right nares. The lesion measured about 16 cm by 20 cm in its widest diameter as shown in Figures 1 and 2 below.
Investigation
Incisional biopsy was done and the histologic analysis confirmed the diagnosis of juvenile psammomatoid ossifying fibroma.
Treatment
A right sided hemi-maxillectomy and reconstruction was done. The lesion was sent for histology and the diagnosis was confirmed. The patient recovered uneventfully after surgery without any sequel. Picture of the patient at about two weeks post surgery is shown below in Figure 3.
Discussion
JOF is a rare type of fibro-osseus lesion affecting children usually less than 15 years. It is a benign odontogenic lesion. Pathogenesis is unknown but it appears to be a spontaneously occurring neoplasm (11). Aside age, other distinctive characteristics of JOF includes high recurrence potentials, site of tumor and radiologic appearance (12). There are basically two histological variants of JOF; the psammomoid and the trabecular types. The former which was confirmed in our patient is usually commoner, more aggressive and has a high recurrence rate as compared to the latter (3). Histologic appearance comprises of trabeculae of woven bone, without osteoblastic rimming and bands of cellular osteoid, within a cell-rich fibrous tissue (13). About 85% of JOF originate in the facial bones, with the maxilla being more common than the mandible, among which 90% arises within the paranasal sinuses (ethmoid > frontal > maxillary > sphenoid sinus). 12% occurs in the calvarial bones and 4% are extracranial (14). Clinical features of JOF include facial deformities, proptosis, exophthalmos, nasal symptoms and sinusitis.
The differential diagnosis of JOF includes fibrous dysplasia, aneurysmal bone cystosteosarcoma, osteoblastoma and cement-osseous dysplasia. Burkitt lymphoma is a near differential diagnosis in our environment being a tropical one. This patient was initially misdiagnosed as a case of Burkitt lymphoma and even had some chemotherapy sessions before JOF was confirmed. This is a common finding in our environment as reported by Osunde et al. (10).
Surgery is the mainstay of managing JOF and this can be achieved by enucleation or curettage for smaller lesions and radical excision for larger ones (15). Kaban et al. (16) suggested thorough curettage or enucleation in combination with adjuvant interferon therapy for one year. Follow up is necessary as recurrence rate vary from 30% to 58% and usually occurs between 6 months and 7 years. Metastasis has not been documented in JOF despite its aggressive local behavior. The current patient was followed up for 5 years post surgery with no recurrence.
Conclusions
Being a relatively rare disease with a myriad of closely related clinical entities and high local aggressive nature, an extremely high index of suspicion is needed for early and appropriate management of JOF, to prevent complications and recurrence.
Acknowledgments
We gratefully acknowledge Mr. Malcolm Bailey and all the healthcare practitioners who took part in his care.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Maria A, Sharma Y, Malik M. Juvenile ossifying fibroma of mandible: a case report. J Maxillofac Oral Surg 2013;12:447-50. [Crossref] [PubMed]
- Zama M, Gallo S, Santecchia L, et al. Juvenile active ossifying fibroma with massive involvement of the mandible. Plast Reconstr Surg 2004;113:970-4. [Crossref] [PubMed]
- El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:296-304. [Crossref] [PubMed]
- Brannon RB, Fowler CB. Benign fibro-osseous lesions: a review of current concepts. Adv Anat Pathol 2001;8:126-43. [Crossref] [PubMed]
- Rinaggio J, Land M, Cleveland DB. Juvenile ossifying fibroma of the mandible. J Pediatr Surg 2003;38:648-50. [Crossref] [PubMed]
- Fakadej A, Boynton JR. Juvenile ossifying fibroma of the orbit. Ophthalmic Plast Reconstr Surg 1996;12:174-7. [Crossref] [PubMed]
- Reaume CE, Schmid RW, Wesley RK. Aggressive ossifying fibroma of the mandible. J Oral Maxillofac Surg 1985;43:631-5. [Crossref] [PubMed]
- Slootweg PJ, Müller H. Juvenile ossifying fibroma. Report of four cases. J Craniomaxillofac Surg 1990;18:125-9. [Crossref] [PubMed]
- Leimola-Virtanen R, Vähätalo K, Syrjänen S. Juvenile active ossifying fibroma of the mandible: a report of 2 cases. J Oral Maxillofac Surg 2001;59:439-44. [Crossref] [PubMed]
- Osunde O, Iyogun C, Adebola R. Juvenile aggressive ossifying fibroma of the maxilla: a case report and review of the literature. Ann Med Health Sci Res 2013;3:288-90. [Crossref] [PubMed]
- Shields JA, Peyster RG, Handler SD, et al. Massive juvenile ossifying fibroma of maxillary sinus with orbital involvement. Br J Ophthalmol 1985;69:392-5. [Crossref] [PubMed]
- Knox GW, Roth M, Saleh H, et al. A unique temporal bone lesion resembling juvenile active ossifying myxoma. Am J Otol 1996;17:297-300. [PubMed]
- Slootweg PJ, Panders AK, Koopmans R, et al. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med 1994;23:385-8. [Crossref] [PubMed]
- Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007;11:R31. [Crossref] [PubMed]
- Shekhar MG, Bokhari K. Juvenile aggressive ossifying fibroma of the maxilla. J Indian Soc Pedod Prev Dent 2009;27:170-4. [Crossref] [PubMed]
- Troulis MJ, Williams WB, Kaban LB. Staged protocol for resection, skeletal reconstruction, and oral rehabilitation of children with jaw tumors. J Oral Maxillofac Surg 2004;62:335-43. [Crossref] [PubMed]
Cite this article as: Animasahun BA, Kayode-Awe G, Kusimo OY. Juvenile ossifying fibroma in a Nigerian boy: a rare case report. AME Case Rep 2019;3:20.