
Osteoma arising from the middle turbinate—a case series
Introduction
Osteomas are benign tumours and the most common fibro-osseous lesions in the sinonasal cavity (1). They are slow growing with no specific growth pattern (2). Among sinonasal osteomas, they are most commonly found in the frontal sinus followed by the ethmoid and maxillary sinuses (3,4). They rarely involve the sphenoid sinuses (5). Headache is a common symptom. We describe 2 cases of large osteomas arising from the middle turbinate.
Case presentation
The first case was a 29-year-old normally fit and well gentleman who presented to the ENT outpatient clinic with a 2-year history of left sided nasal obstruction that was getting gradually worse with pain over his external nose and developing a visible swelling. This was associated with a poor sense of smell and taste, rhinorrhoea and headaches. On examination, he had grade 3 polyps bilaterally worse on the left.
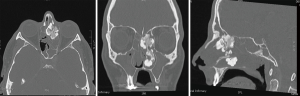
He underwent a CT scan of the paranasal sinuses (Figure 1) which showed a large lobular densely calcified mass centred on the left middle turbinate, with “cauliflower” extension superiorly, laterally, and inferiorly within the nasal airway. There was bulging of the lamina papyracea into the left orbit with some reduction in bone density. There was also a defect in the cribriform plate on the left, almost a centimetre in length. The lesion just bulged into the cribriform plate defect, raising the possibility of intracranial extension. There was extensive soft tissue opacification through the remainder of the left-sided paranasal sinuses, including soft tissue bulging into postnasal space; consistent with retained secretions and mucosal thickening. Further polyps were seen beneath the middle turbinate on the right nasal airway, and near complete opacification was noted in the right maxillary antrum and sphenoid and partial opacification of the frontal and ethmoid loculi.
He was treated with fusion navigation assisted FESS polypectomy and excision of the bony mass tethered to the left middle turbinate. Left polyps were excised and sent for histology. The large bony mass centred on the middle turbinate was drilled through and the extending polyps excised. Delivery of the large mass with attached polyps required septal dislocation and vomerine spur reduction. Remnant of the mass remained on the left middle turbinate. A biopsy was taken from the anterior end. This was attached to the skull base and therefore not removed. Bilateral uncinectomy and middle meatal antrostomies were performed to eradicate the polyps. There was no need to enter the frontal sinus.
Histopathology examination of the specimens showed the polyps to be inflammatory. Within the left bony mass, there were fibrocellular areas comprising of bland mononuclear stromal cells admixed with mixed inflammatory infiltrates including eosinophils. Also identified in the stroma were irregular vital bony trabeculae, comprised of lamellar bone admixed with woven bone. Osteocytes within lacunae and prominent reversal lines were identified in the bony fragments. These bony fragments were lined by osteoblasts in part and devoid of the same elsewhere. No evidence of malignancy was identified. The appearances were in keeping with a benign fibro-osseous lesion.
Three weeks post-surgery, his symptoms had improved. There was some mucopus in the left nasal cavity but with no evidence of polyps. The right nasal cavity had healed well. He was further prescribed Flixonase nasules 3 drops each nostril twice a day with follow up in 6 months.
The second case is of a 65-year-old lady who was admitted to hospital for headaches and low blood pressure under the medical team. She had a background history of systemic lupus erythematous, osteoarthritis, coeliac disease, Barrett’s oesophagus, hiatus hernia, familial hypercholestrolaemia. Her symptoms were initially treated conservatively.
A CT scan of her head was done which showed there to be a 2.8 cm × 4 cm × 4 cm area of high-attenuation present within the left-side of the nasal cavity, with involvement of the medial aspect of the left opacified maxillary antrum. Bone window review revealed heterogenous bone-density, with both sclerotic areas along with patchy 'woolly' regions. Both the ethmoid air cells and frontal sinuses were completely opacified bilaterally, and moderate circumferential mucosal thickening was further noted within the right maxillary and sphenoid sinuses.
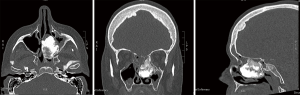
She was eventually discharged and referred to the outpatient ENT clinic. She had bilateral nasal obstruction and on examination had grade 2 polyps bilaterally she was commenced on betnesol nasal drops and underwent a further CT scan specific for the paranasal sinuses (Figure 2) which showed there to be a large osteoma measuring 4.0 cm × 3.3 cm × 3.8 cm within the posterior aspect of the left maxillary antrum, ethmoidal complex and left nasal cavity. It markedly deviated the nasal septum to the right and extended into the post-nasal space. In addition there was evidence of extensive opacification within the maxillary, frontal, ethmoid and sphenoid sinuses bilaterally.
She then was treated with fusion navigation assisted excision of the mass. The bony mass was seen to have replaced and medialised the left middle turbinate. It was dissected free from its position abutting the left lamina and left posterior fontanelle. The mass was freed and drilled into 3 parts. An attempt was made to deliver it through the nasopharynx but failed. Thus bone rongeurs were used to nibble at it extensively. A posterior septotomy was done to facilitate dissection and removal of the tumour. Posterior septum was then deflected to the right. The left lamina papyracea was noted to be dehiscent in a small area superiorly. The frontal sinuses were not opened. Nasal packs were inserted bilaterally at the end of the procedure. These were removed prior to discharge from hospital. She was prescribed saline nasal douching with outpatient follow up in 2 weeks.
Histopathological examination of the mass found it to consist of dense cortical lamellar bone. There were also bone trabeculae with a fibrotic marrow space. These features would be consistent with a benign osteoma. No features to suggest malignancy were identified.
At her follow up, she was found to have made an excellent recovery. She was able to breathe clearly through both nostrils and her sense of smell and taste had returned. She had less headaches. On examination there was some nasal crusting bilaterally. She was commenced on Flixonase nasules, Naseptin cream and oral clarithromycin for 6 weeks.
Follow up 4 weeks later found her asymptomatic. On examination she had a septal defect but with a clear healthy nasal cavity. She was prescribed Avamys nasal spray to be used on a long term basis.
Discussion
Headache is a common symptom in sinonasal osteomas, presenting usually in the second to fifth decades (5). Paranasal sinus lesions are commonly overlooked as a cause of headaches (6). It should be part of the differential diagnosis (6). Many osteomas go undetected (7).
Patients can present in many ways including acute sinusitis, headache, epistaxis, orbital cellulitis and diplopia, asymptomatic (3,5). Some patients are asymptomatic with 1% of osteomas being found incidentally on routine radiological investigations (5).
They are most commonly found in the frontal sinus followed by the ethmoid and maxillary sinuses (3,4). They have also been found arising from the nasal bone, hard palate, nasolacrimal duct, nasal septum (8). Osteomas arising from the nasal turbinates are extremely rare (9). They have been described arising from the inferior turbinates (9).
Pathogenesis remains controversial with three current theories regarding osteoma formation (10). The developmental theory suggests that cells during embryonic development become trapped and undergo unregulated proliferation causing the formation of an osteoma. Whereas both the traumatic and infectious theory hypothesise that inflammation is a key factor in the formation of excessive bony proliferation (10).
Endoscopic resection of frontal osteomas are usually adequate and safe however, occasionally external auxiliary approach may be required when the sinus ostium is narrow or the tumour is attached to vital surrounding structures such as the orbital roof (5). An argument for open surgery is better exposure and less risk of incomplete excision and may be necessary for giant tumours (5). However it does come with increased morbidity. An indication for osteoplastic flap are laterally placed osteomas.
Conclusions
Although extremely rare, osteomas can arise from the middle turbinate causing symptoms such as headache, facial pain, nasal obstruction and visual problems.
As they are slow growing, they can be of large size at presentation. Treatment usually involves surgical excision. Endoscopic excision is usually adequate and safe.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: There is no patient identifiable data within the text.
References
- Eller R, Sillers M. Common fibro-osseous lesions of the paranasal sinuses. Otolaryngol Clin North Am 2006;39:585-600. x. [Crossref] [PubMed]
- Halawi AM, Maley JE, Robinson RA, et al. Craniofacial osteoma: clinical presentation and patterns of growth. Am J Rhinol Allergy 2013;27:128-33. [Crossref] [PubMed]
- McHugh JB, Mukherji SK, Lucas DR. Sino-orbital osteoma: a clinicopathologic study of 45 surgically treated cases with emphasis on tumors with osteoblastoma-like features. Arch Pathol Lab Med 2009;133:1587-93. [PubMed]
- Buyuklu F, Akdogan MV, Ozer C, et al. Growth characteristics and clinical manifestations of the paranasal sinus osteomas. Otolaryngol Head Neck Surg 2011;145:319-23. [Crossref] [PubMed]
- Strek P, Zagolski O, Skladzien J, et al. Osteomas of the paranasal sinuses: Surgical Treatment Options. Med Sci Monit 2007;13:CR244-50. [PubMed]
- Lee JH, Kim HJ, Hong YH, et al. Underestimation of rhinogenic causes in patients presenting to the emergency department with acute headache. Acta Neurol Taiwan 2015;24:37-42. [PubMed]
- Zhuang A, Li Y, Lin M, et al. Ethmoid Osteoma as a Culprit of Orbital Emphysema: A Case Report. Medicine (Baltimore) 2015;94:e724. [Crossref] [PubMed]
- Wang HM, Xue WS, Gang YU. A case report: osteoma of the nasal septum. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2012;47:777-8. [PubMed]
- Grabovac S, Đanić Hadžibegović A, Markešić J. Inferior turbinate osteoma as a cause of unilateral nose obstruction. Coll Antropol 2012;36:189-91. [PubMed]
- Viswanatha B. Maxillary sinus osteoma: two cases and review of the literature. Acta Otorhinolaryngol Ital 2012;32:202-5. [PubMed]
Cite this article as: Gan RW, Gubbi G, Blackabey V, Ward VM. Osteoma arising from the middle turbinate—a case series. AME Case Rep 2019;3:17.


