
Spermatic cord paratesticular tumor: a rare case report
Introduction
Angiomyofibroblastoma (AMF) is a rare tumor that occurs predominantly in the external female genitalia (vulva, vagina, pelvis and perineum) (1,2). AMF is rarer in men and tends to occur in the inguinal region, scrotum, perineum and spermatic cord (3). There are even rarer reports of growths in other sites, such as the foot (2). From the clinical standpoint, the tumor is well defined, asymptomatic and has slow growth (4). In this paper, we report a case of a paratesticular tumor of the spermatic cord and offer a review comparing it to the main differential diagnosis: angiomyxoma.
Case presentation
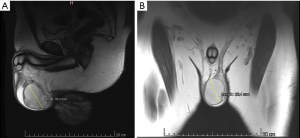
A 34-year-old male with no relevant medical history sought medical care in 2017 after noticing a painless, progressive increase in scrotum volume on the left side over a five-year period. Doppler ultrasound revealed a left parascrotal nodule of unknown etiology. The study of markers was negative for all testicular tumors. Contrast magnetic resonance revealed a heterogeneous tumor in the scrotum, which was defined as a nodule of unknown etiology. Leiomyoma was the hypothetical diagnosis (Figure 1).
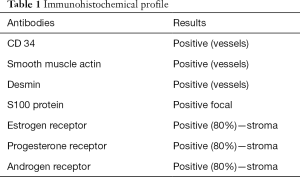
After months of deliberation, the decision was made to perform radical treatment with orchiectomia through the inguinal route. The exploratory procedure was performed in February 2018, which revealed a well-defined tumor adjacent to the testicle with a fibroelastic consistency measuring approximately 6 cm at its largest diameter. Based on this finding, excision of the tumor was performed with the preservation of the testicle. The surgical specimen was sent for anatomopathological analysis. The growth measured 6.5 cm × 5.0 cm × 4.5 cm, weighed 86.0 g, had a cream to brown color and was finely granulous, suggesting AMF, which was confirmed by the immunohistochemical markers (Table 1).
Full table
Discussion
Angiomyofibroblastoma was first described by Fletcher et al. in 1992 as a tumor that occurs rarely in the reproductive system of older women (4), particularly in the vulva, labia majora, vagina and perineum as well as around the clitoris.
Histopathologically, AMF has different regions containing either few or thousands of cells with diverse cellular morphology, low mitotic activity and fusiform cells with limited atypia. The major characteristics are prominent vascularization with perivascular fibrinoid hyalinization. AFM is a well-defined superficial tumor (5,6).
Iwasa and Fletcher examined 51 cases of inguinoscrotal cellular angiofibroma in 25 men and vulvovaginal angiofibroma in 26 women. CD34 was expressed in 60% of cases, smooth muscle actin in 21% and desmin in 8%. S-100 protein was negative in all cases (7). In the immunohistochemical analysis, AMF reacts positively and diffusely with vimentin, with the variable expression of CD34, smooth muscle actin as well as estrogen and progesterone receptors (8). In the present case, all these antibodies were positive, including estrogen, progesterone and androgen receptors.
The main differential diagnosis is angiomyxoma, which also develops in the pelvic and perineal region. This tumor is aggressive, locally infiltrative and invasive. It has no metastatic potential, but recurrences are frequent. In the immunohistochemical analysis, both AMF and aggressive angiomyxoma are positive for desmin and smooth muscle actin. The best criterion for differentiating these tumors is the high cellularity and more pronounced vascularization in AMF, whereas smooth muscle cells are characteristically found around the vessels in angiomyxoma (7). Angiomyxoma is generally located deeper and has an invasive aspect, abundant mucin and frequent extravasation to the blood stream, whereas AMA is located more superficially, with a well-defined appearance and sparse mucin (9). The patient in the present report had a well-defined tumor with free margins and no invasion of the adjacent tissues.
Tumor regression has been seen in AMF (4). There is only one report of recurrence (after 13 years) and no cases of sarcoma or malignant transformation have been described. Recommended treatment is surgical excision with wide margin. Both short-term and long-term postoperative follow up is required (1,5).
Conclusions
Spermatic cord angiomyofibroblastoma can be considered an exception among paratesticular tumors, which are also rare. The literature offers little information on this histopathological type, but it has been demonstrated that simple excision of the tumor is curative in practically all cases. Divergences of opinion are found regarding the need for long-term follow up.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ding G, Yu Y, Jin M, et al. Angiomyofibroblastoma-like tumor of the scrotum: a case report and literature review. Oncol Lett 2014;7:435-8. [Crossref] [PubMed]
- Bouhajja L, Rammeh SA, Sayari S, et al. Angiomiofibroblastoma do cordão espermático: relato de caso. Pathologica 2017;109:368-70. [PubMed]
- Salunke AA, Chen Y, Lee VK, et al. Angiomyofibroblastoma of the foot: a rare soft tissue tumor at unusual site. Indian J Surg Oncol 2017;8:210-3. [Crossref] [PubMed]
- Lee SH, Yang JW, Do JM, et al. Angiomyofibroblastoma-like tumor of the scrotum. Korean J Urol 2010;51:365-7. [Crossref] [PubMed]
- Tzanakis NE, Giannopoulos GA, Efstathiou SP, et al. Angiomyofibroblastoma of the spermatic cord: a case report. J Med Case Rep 2010;4:79. [Crossref] [PubMed]
- Wolfman DJ, Marko I, Gould CF, et al. Tumores extratesticulares mesenquimais e condições semelhantes a tumores: dos arquivos de patologia radiológica. Radiografias 2015;35:1943-54.
- Mediero G, Dorrego A, Mora CN, et al. Angiomiofibroblastoma invasivo escrotal: primer caso descrito. Arch Esp Urol 2000;53:827-9.
- João R, Oliveira e Neta J, Farinha R, et al. Angyomiofibrossarcoma-like tumor of male genital track mimicking a testicular tumor. Acta Urol Port 2015;32:43-6.
- Msakni I, Ghachem D, Bani MA, et al. Paratesticular angiomyofibroblastoma-like tumor: unusual case of a solidocystic form. Case Rep Med 2017;2017:1273531. [Crossref] [PubMed]
Cite this article as: da Silva RF, Pinto Filho IC, Querichelli AF, Ozima BA, Spessoto LC, Fácio Júnior FN. Spermatic cord paratesticular tumor: a rare case report. AME Case Rep 2019;3:8.


