
Xanthogranulomatous orchitis: case report of a rare condition
Introduction
Xanthogranulomatous orchitis is a non-neoplastic inflammatory condition characterized by the destruction of testicular tissue with macrophage infiltrate (1). Xanthogranulomatous masses is often found in the kidneys and gallbladder, with few cases of occurrence in the testicle and spermatic cord (2,3). We report a case of xanthogranulomatous orchitis in an adult.
Case presentation
JMS, 55 years of age, diabetic and hypertensive, visited emergency care for testicular pain and swelling with an eight-day history, but a one-year evolution. The patient also reported having chills in the previous days and visited the emergency services on the seventh day of empirical treatment with ciprofloxacin for orchiepididymitis prescribed at another healthcare service.
The examination revealed testicular edema, hyperemia, increased volume with a hard consistency and pain to the touch of the right testicle as well as atrophy of the left testicle due to a past history of trauma.
The complete blood count revealed leukocytosis, increased segmented neutrophils and C-reactive protein of 13.28 mg/dL (value of reference: 0.00 to 0.50 mg/dL). Ultrasound of the scrotum revealed the right testicle with increase dimensions, absent vascular flow (Doppler ultrasound) and an adjacent pseudomass, with a thick epididymis, suggesting testicular torsion. The ultrasound exam revealed a hardened right testicle with no vascular flow, areas of necrosis and purulent secretion as well as thickening of the inguinal cord. Orchiectomy was performed with a margin up to the cord.
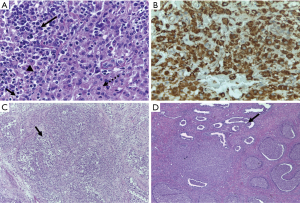
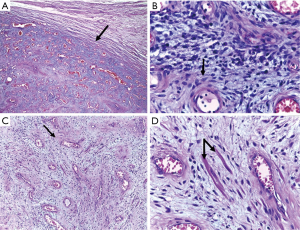
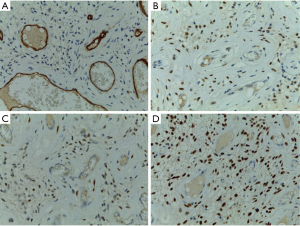
The patient received discharge from hospital on the second postoperative day. The biopsy revealed extensive testicular ischemic necrosis with areas of exudation, a chronic peri-testicular xanthogranulomatous inflammatory process, recent thrombosis, fibrous capsular thickening and acute epididymitis, with the formation of luminal abscesses confirmed by the immunohistochemical analysis (CD34-positive) (Figures 1-3).
The patient is currently in outpatient follow up, with occasional pain on the right side of the scrotum and undergoing hormonal replacement due to the atrophic post-trauma lest testicle.
Discussion
Xanthogranulomatous inflammation is rare with an unclear etiology. One explanation for this condition is a chronic inflammatory process due to duct obstruction. This process is influenced by changes in the immune system and both lipid and macrophage metabolism, lymphatic dysfunction, a foreign body with calculus and surgical thread (4). Commonly found in the liver and gallbladder, xanthogranulomatous inflammation can also be seen in other organs, such as the appendix, ovaries and bladder (5), but can also affect the prostate, epididymis and testicle.
Diabetes, as in the present case, is directly linked to the etiology of xanthogranulomatous inflammation, since diabetic patients are often immunocompromised and the entire process of adherence, chemotaxis and phagocytosis is compromised (6).
Microscopic findings include yellowish nodules with “lipid-laden” macrophages associated to lymphocytes, giant cells and necrosis. However, such findings are not specific to the xanthogranulomatous process and could be concomitant to a tumor (7). The diagnosis is challenging, as the condition can resemble bacterial orchitis, which improves with antibiotic therapy, malakoplakia with typical Michaelis-Gutmann bodies (3) and neoplasm with differences in tumor and immunohistochemical markers (8).
Due to the destructive effects of xanthogranulomatous orchitis, treatment should be aggressive, with radical orchiectomy (as performed in the present case), which could be partial in some cases. Antibiotic therapy for anaerobic bacteria is also important (8-10).
As the patient became symptomatic due to the orchitis and atrophy, hormonal replacement therapy with testosterone was indicated to avoid hypogonadism (11).
Conclusions
Xanthogranulomatous orchitis is a rare condition with an unclear etiology. The present report serves as a reminder of the importance of this condition and can facilitate its understanding, differential diagnosis and the establishment of adequate treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Yamashita , et al. Xanthogranulomatous orchitis after blunt testicular trauma mimicking a testicular tumor: a case report and comparison with published cases. Urol J 2017;14:3094. [PubMed]
- Wen YK, Chen ML. Xanthogranulomatous pyelonephritis complicated by emphysematous pyelonephritis in a hemodialysis patient. Clin Nephrol 2007;68:422-7. [Crossref] [PubMed]
- Nistal M, Gonzalez-Peramato P, Serrano A, et al. Xanthogranulomatous funiculitis and orchiepididymitis: report of 2 cases with immunohistochemical study and literature review. Arch Pathol Lab Med 2004;128:911-4. [PubMed]
- Demirci D, Ekmekcioglu O, Soyuer I, et al. Xanthogranulomatous orchitis with scrotal fistulas. Int J Urol 2004;11:686-8. [Crossref] [PubMed]
- Chlif M, Chakroun M, Ben Rhouma S, et al. Xanthogranulomatous pyelonephritis presenting as a pseudotumour. Can Urol Assoc J 2016;10:E36-40. [Crossref] [PubMed]
- Delamaire M, Maugendre D, Moreno M, et al. Impaired leukocyte functions in diabetic patients. Diabet Med 1997;14:29-34. [Crossref] [PubMed]
- Val-Bernal JF. Concurrent xanthogranulomatous orchiepididymitis and seminoma in the same testis. Pathol Int 2010;60:55-8. [Crossref] [PubMed]
- Alazab RS, Ghawanmeh HM. Xanthogranulomatous orchitis: rare case with brief literature review. Urol Case Rep 2017;13:92-3. [Crossref] [PubMed]
- Al-Said S, Ali A, Aloibaidy AK, et al. Xanthogranulomatous orchitis: review of the published work and report of the case. Int J Urol 2007;14:452-4. [Crossref] [PubMed]
- Rifat Mannan AA, Kahvic M, Sara YA, et al. An unusual case of extensive xanthogranulomatous Orchitis in a diabetic patient. Med Princ Pract 2009;18:418-21. [Crossref] [PubMed]
- Martits AM, Costa EMF, Nardi AC, et al. Late-onset hypogonadism or ADAM: treatment. Rev Assoc Med Bras 2014;60:404-14. [Crossref]
Cite this article as: Gongora e Silva RF, Pinto IC, Constantino EC, Querichelli AF, Spessoto LC, Fácio FN Jr. Xanthogranulomatous orchitis: case report of a rare condition. AME Case Rep 2019;3:4.


