Surgical reduction technique (transpedicle) for unstable thoracolumbar burst fractures with retropulsion resulting in severe spinal canal stenosis: a preliminary case report
Introduction
Thoracolumbar burst fractures are common entity in polytraumatized patients. The common mechanism is axial compression force to spine which led to failure of anterior and middle column (1). Some of this vertebral collapse may result in spinal canal invasion with or without neurological deficit. In this situation, early surgical stabilization with decompression is vital to restore neurological function (2). Various surgical methods had been described to decompress spinal canal though direct anterior approach or indirect posterior decompression and instrumentation (3). Although anterior fixation had been recommended for retropulsed vertebra fracture for direct decompression but studies had shown posterior approach is equally effective (4). Thus, we employed a posterior approach with a unique transpedicle reduction technique at the level of fracture for decompression. These case reports described the surgical technique and outcomes for patients with traumatic thoracolumbar retropulsed burst fractures treated with posterior decompression transpedicle reduction and posterior spinal instrumentation.
Case presentation
Case 1
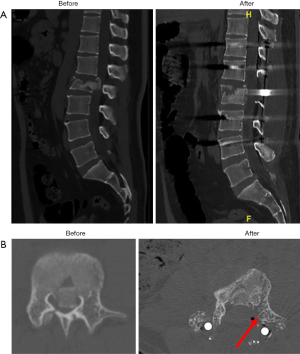
A 16-year-old teenage, was a passenger when his car collided with a tree after avoiding a dog on the road. He sustained multiple injuries to both of his legs and lower back. He complained of severe instability back pain after the accident. However, his sensation, bowel and urine function were spared. Upon examination, his vital were stable. He was alert, conscious and communicative. Both of his legs and ankles were deformed and swollen. The neurological findings were stated below (Table 1).
Full table
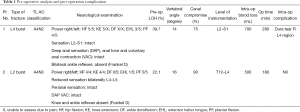
He suffered from an unstable burst fracture L4, L5 and L3 spinous process fracture with neurological deficit, closed fracture right mid-shaft tibia, bimalleolar fractures of both ankles, left tibia plafond fracture. Interlocking nail right tibia, screw fixation of both medial malleoli, plating of left fibula, screw fixation, plating and bone grafting of left tibia plafond, posterior decompression and posterior instrumentation of L2–S1 with dura repair were performed for this patient. CT scan showed the severity of the spinal canal compression and the result after vertebral fracture reduction (Figure 1A,B). CT spine axial view showed pre and post reduced retropulsed fragment and widen spinal canal at L4 level. Red arrow represented remnant of transpedicle approach (Figure 1B).
Case 2
A 38-year-old university lecturer had a fall from height of 12 feet ladder and landed on his back. He immediately developed severe back pain and bilateral lower limb weakness and numbness thereafter. Urinary and bowel functions were normal. Upon examination, he was unable to sit up or walk. There is pinpoint tenderness over thoracolumbar region. The neurological deficits were noted as below (Table 1).
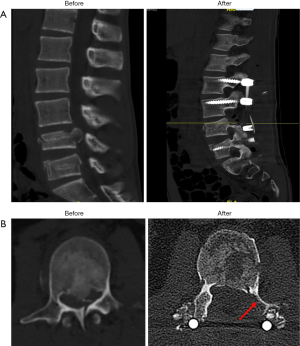
He sustained L2 unstable burst fracture with neurological deficit (Frankel D). Posterior decompression reduction and instrumentation of T12–L4 was performed. The CT scans showed widen of spinal canal space, reduction of vertebral height and kyphotic angle in comparison (Figure 2A,B).
Surgical technique
All patients were placed in prone position on a Jackson frame with posts to support chest wall and pelvis, under general anaesthesia. Traumatic kyphotic segmental fracture of vertebra repositioned after lying on the Jackson frame and reduction controlled on lateral image intensifier view. A midline posterior approach was employed and paraspinal musculature was dissected. Screws were fixed two levels above and below the fracture. Next, laminectomy was performed at the level of fracture. Inferomedial segment of the pedicle was undercut using Kerrison laminectomy punch as evident by the CT scans (Figures 1B,2B). Nerve root was protected with nerve root retractor and a Caperner’s gauge was passed in front of anterior thecal sac through the opening. Placement of Caperner’s gauge on top of the retropulsed fragment was confirmed on image intensifier. Gentle tapping was performed to reduce the retropulsed fragments under image intensifier. Rods length was measured and contoured at a straight or slight lordotic angle to aid further reduction. Rods were fixed to the pedicle screws and further attempt of controlled reduction made with interbody distractor or compressor under image intensifier.
Results
All patients were followed up for at least 3 months. The average operation time for both patients was 230 minutes. Blood loss on average was 600 mL (Table 1).
Neurological recovery
All patients recovered at least by one grade in power (MRC score). No patients suffered from deterioration of neurology post operatively (Table 2).

Full table
Radiographic results
Based on CT scan, all patients had severe canal compromise of average 77.5% (range 75–90%) with vertebral height loss of 30.9% comparing vertebral above and below the fracture. The segmental kyphotic angle on average was 15 degrees (Table 1).
Immediate post operation showed complete release of spinal canal stenosis with reduction of segmental kyphotic angle to average of 5 degrees. Vertebral height was restored (Table 2).
During the latest radiographic follow up, reduction of vertebral height and kyphotic angle were maintained. The canal space remained free (Table 2).
Complications
First patient had a dura tear posteriorly at L4 level. Dura repair was performed uneventfully and no significant post operation complication such as cerebral spinal fluid leakage, infection, wound breakdown or bleeding (Table 1).
Discussion
Management of thoracolumbar burst fractures is still an entity for debate. The stability of the fracture, degree of canal stenosis, present of neurological deficit, injury of posterior ligamentous complex and patient’s co-morbidity formed the basis guide for surgical intervention (2-4). Anterior vertebral body reconstruction with short-segment posterior instrumentation exhibit the most stability, lower risk of re-kyphosis, shorter motion segment involvement and fewer risk of implant failure (5). In addition to reducing the risk of residual kyphosis, it lowered the risk of implant failure when it decreased anterior vertebral stress on pedicle screws where it could loosen, break, dislodge or disconnect from the rod (3). However, Reinhold et al. reported that after operation of 733 patients, posterior approach only instrumentation result in better functional and subjective outcome compared to patients who undergone combined anterior-posterior surgery (5).
In attempt to improve functional outcome for patients in the study, we chose posterior approach fixation. Most studies advocated anterior approach for retropulsed fragment decompression because direct access to the fracture fragment is easier through anterior approach. However, anterior approach had a higher morbidity risk, higher bleeding rate and healing time (2-5). Hence, we advocated posterior decompression with direct fracture reduction for patients with spinal canal stenosis of more 50% (2). Standard laminectomy at the fracture level posed a challenge for surgeons to decompression the retropulsed fracture fragment due to limited field for visualization and instrumentation. Therefore, it is logical to enlarge the operative field without compromising the stability of the spine or collateral damage to the surrounding nerves or spinal cord. We undercut the inferomedial part by a quarter of one pedicle after laminectomy under direct visual to create an opening for a Carpenter’s gauge to pass anterior to thecal sac. It is a safe option as spinal cord and nerve root is protected intentionally with the passing of instrument postero-laterally to the spinal cord. Furthermore, tapping of retropulsed vertebra were done under radiograph guidance. Stability of spine is preserve by limiting pedicle dissection. Another advantage of reducing the retropulsed fragment is to restore vertebra body mass in aid to prevent re-kyphosis. The dura tear in the first patient which was located posteriorly was most likely due to the sharp impingement of spinal cord against the spinous process.
The limitation of this case series was small sample size. Only with larger randomized controlled studies, should we draw a conclusion of this surgical technique.
In retrospect, posterior decompression through transpedicular approach and posterior short-segment stabilization resulted in excellent immediate restoration of segmental kyphosis, significant spinal canal decompression, normalised vertebral body height in patients with a thoracolumbar retropulsed burst fracture with severe spinal canal stenosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976) 1992;17:528-40. [Crossref] [PubMed]
- Anderson KK, Tetreault L, Shamji MF, et al. Optimal Timing of Surgical Decompression for Acute Traumatic Central Cord Syndrome: A Systematic Review of the Literature. Neurosurgery 2015;77 Suppl 4:S15-32. [Crossref] [PubMed]
- Sasso RC, Renkens K, Hanson D, et al. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 2006;19:242-8. [Crossref] [PubMed]
- Ge CM, Wang YR, Jiang SD, et al. Thoracolumbar burst fractures with a neurological deficit treated with posterior decompression and interlaminar fusion. Eur Spine J 2011;20:2195-201. [Crossref] [PubMed]
- Reinhold M, Knop C, Beisse R, et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J 2010;19:1657-76. [Crossref] [PubMed]
Cite this article as: Choo CH, Kwan MK, Chris Chan YW. Surgical reduction technique (transpedicle) for unstable thoracolumbar burst fractures with retropulsion resulting in severe spinal canal stenosis: a preliminary case report. AME Case Rep 2018;2:38.


