Laparoscopic right varicocelectomy for chronic scrotal pain
Introduction
Varicocele represents a common abnormality between adult males and has a causative association with infertility, subfertility or hypogonadism in approximately 25% of the cases (1). Spermatic vein dilatation and reflux is usually located at the left side due to the anatomical relation of the left spermatic vein and the left renal vein. Varicoceles are often palpable and/or visible, depending on their grade, and create scrotal discomfort or chronic pain. Bilateral varicocele is seldom demonstrated, while isolated right varicocele is extremely rare. Right varicocele, due to its rarity, stimulates the suspicion of an underlying pathology such as, retroperitoneal tumors, vena cava thrombus or kidney tumors, and further investigation is usually carried out (2). We present a case of a 61-year-old man presented to our department with chronic right scrotal pain and isolated right varicocele which treated laparoscopically.
Case presentation
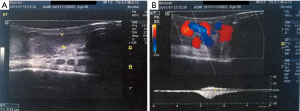
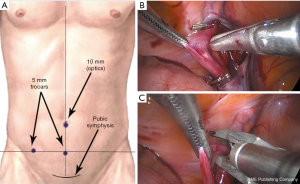
A 61-year-old male presented in the outpatients’ clinic complaining for chronic pain in the right scrotal area for the last 5 years. The Visual Analog Scale (VAS) for pain (0–10 scale) was 6. The patient was otherwise healthy with no medical history or other comorbidities. Clinical examination revealed a grade I right varicocele (palpable during Valsalva straining maneuver), normal testicles and normal contralateral scrotum. No inguinal hernias or other masses were diagnosed. The patient underwent a full laboratory and imaging evaluation. Blood examinations were normal including beta-human chorionic gonadotropin, alpha-fetoprotein and lactate dehydrogenase tests, urine analysis had no pathology, and sperm culture revealed a multi-sensitive Staphylococcus epidermidis infection. Semen analysis was not curried out due to patient’s preference and disinterest for fertility. Moreover, the patient reported previous successful conception. The presence of the right varicocele was also demonstrated by a scrotal color-doppler ultrasound examination that measured the diameter of the vein up to 0.54 cm and showed a high grade reflux during Valsalva maneuver (Figure 1). The patient was initially treated with antibiotic therapy and anti-inflammatory drugs, and further investigation with urinary ultrasound imaging and pelvic-abdomen Computed Tomography was carried out, which were negative for any additional pathology. Nevertheless, 3 months later, there was no improvement in the patient’s symptoms and surgical treatment of the varicocele was decided. Laparoscopic approach was selected for the advantage of diagnostic laparoscopy, effective spermatic vein ligation and fine cosmetic result. For laparoscopic access, after the pneumoperitoneum creation, a 10 mm umbilical port was used for the high definition camera (HD Karl Storz laparoscopic system, Tuttlingen, Germany) and two 5 mm ports at the middle-line and right lateral area (Figure 2A). Diagnostic laparoscopy was negative for any concomitant intra-abdominal pathology. Three veins were recognized and ligated using metallic clips below the level of the right inguinal ring, while left side was normal (Figure 2B,C). No intraoperative or postoperative complications were observed and the patient was discharged after 24 hours. One month after the operation, complete clinical response was observed with the patient reporting a zero in VAS for pain and resolution of the varicocele.
Discussion
The prevalence of varicocele is reaching 15% in the general male population and it is typically found in young adolescents who seek infertility treatment, but recent epidemiological data suggest that the prevalence is increasing with age (3). Varicocele is an acquired cause of testicular deficiency in approximately 25% of men with abnormal sperm diagram. Current, high quality evidence supports that, surgical correction of varicoceles can result in the improvement of semen parameters even for non-obstructive azoospermic patients (1). In general, only patients with clinical (grade > I) varicocele may benefit from surgery and achieve pregnancy.
The pathophysiologic mechanism of chronic scrotal pain (orchialgia) is not fully understood yet, still, varicocele is considered the responsible cause in up to 8.8% of the cases. Therefore, chronic discomfort in clinical varicocele requires surgical intervention especially when no other pathology can be demonstrated and pain resolves in approximately half of the patients (4). Other series have reported pain resolution in 87% of the patients after laparoscopic varicocelectomy (5).
Regarding the site, varicoceles are located in the left side in the vast majority of the cases, while bilaterality is reported in 15% to 50% (6). Pathophysiologically, left vein dilatation is a result of increased venous pressure or valvular incompetence in the left renal vein where the left internal spermatic vein expands, collateral venous anastomoses or the “nutcracker” phenomenon (compression of the left renal vein between the aorta and superior mesenteric artery) (7). On the contrary, isolated right side varicocele should prompt further imaging evaluation for the exclusion of malignancies, especially renal cell carcinoma with renal vein thrombus (2).
Several surgical and radiological techniques have been suggested for the treatment of the varicocele. Amongst them classic open retroperitoneal (Palomo), inguinal and sub-inguinal (microsurgical) approach, sclerotherapy and embolization and finally laparoscopic and robot-assisted procedures. Recurrence rates have been reported from 0.8% (for the microsurgical surgery) to 29% (for the open Palomo technique). Complications include scrotal hematomas, hydrocele, testicular atrophy, thrombophlebitis, and epididymitis. Microsurgical repair seems to have an advantage in semen parameters improvement compared to open or laparoscopic surgery but longer operating time. Laparoscopic surgery has the advantage of visual magnification and high-quality visualization of the operative field and high efficacy in bilateral varicoceles. Additionally, cosmetic results are usually excellent; post-operative pain low and hospital stay minimal. However, the need for general anesthesia and the relatively higher rate of complications is a drawback (8).
Acknowledgements
The authors would like to thank the Operating Theater Head Nurse, Mr. Dimitris Athanasiadis for his contribution to the treatment of the patient.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Agarwal A, Deepinder F, Cocuzza M, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology 2007;70:532-8. [Crossref] [PubMed]
- Masson P, Brannigan RE. The varicocele. Urol Clin North Am 2014;41:129-44. [Crossref] [PubMed]
- Alsaikhan B, Alrabeeah K, Delouya G, et al. Epidemiology of varicocele. Asian J Androl 2016;18:179-81. [Crossref] [PubMed]
- Sigalos JT, Pastuszak AW. Chronic orchialgia: epidemiology, diagnosis and evaluation. Transl Androl Urol 2017;6:37-43. [Crossref] [PubMed]
- Kachrilas S, Popov E, Bourdoumis A, et al. Laparoscopic Varicocelectomy in the Management of Chronic Scrotal Pain. JSLS 2014;18:e2014.00302.
- Zini A, Boman J. Varicocele: red flag or red herring? Semin Reprod Med 2009;27:171-8. [Crossref] [PubMed]
- Clavijo RI, Carrasquillo R, Ramasamy R. Varicoceles: prevalence and pathogenesis in adult men. Fertil Steril 2017;108:364-9. [Crossref] [PubMed]
- Yuan R, Zhuo H, Cao D, et al. Efficacy and safety of varicocelectomies: A meta-analysis. Syst Biol Reprod Med 2017;63:120-9. [Crossref] [PubMed]
Cite this article as: Chondros K, Kountourakis E, Kalogridaki M, Grekos K. Laparoscopic right varicocelectomy for chronic scrotal pain. AME Case Rep 2018;2:37.


