Hemorrhagic transformation of posterior fossa ischemia after antithrombotic therapy for a blunt vertebral artery injury: a case report
Introduction
Blunt cerebrovascular injury (BCVI) constitutes a relatively rare but important clinical entity, whose diagnosis, treatment, and follow-up have remained controversial (1,2). The incidence of vertebral artery injuries after blunt trauma (BVAI) has been reported to be as high as 73% in selected populations, while its associated mortality and its permanent morbidity may be as high as 8% and 24%, respectively (1,2). Symptomatic patients experience ischemic events involving the posterior fossa neural structures after a variable latent period (1-3). Antithrombotic therapy remains the treatment of choice, as it decreases the incidence of a post-traumatic stroke and improves the neurological outcome (1-4). Herewith, we present a rare case with a hemorrhagic transformation of an ischemic stroke of the cerebellum due to a BVAI, its diagnostic approach, its associated treatment challenges, and its overall outcome. Written informed consent was obtained from the patient for publication of this case report and any accompanying data.
Case presentation
A 69-year-old man was admitted to the emergency department of a regional hospital after being involved in a motor vehicle collision. His previous medical history was unremarkable. He reported no complaints upon his admission, and his clinical examination revealed no abnormalities. A head CT scan revealed no abnormalities, while the cervical spine CT scan demonstrated fractures of the C4 and C5 transverse process on the right side (Figure 1A,B). No other injuries were identified.
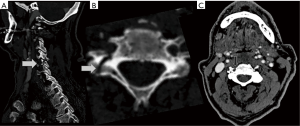
On the second day, the patient was transferred to the Department of Neurosurgery at our University Hospital. Both his clinical and his neurological status had remained unchanged. A CT angiography (CTA) of the neck vessels could not depict the right vertebral artery, from the level of C5 and above (Figure 1C). Based on his CTA findings we initiated a prophylactic treatment with a low dose of aspirin (80 mg orally, once daily).
Two days later, the patient developed symptoms and signs of posterior fossa ischemia, including persistent dizziness, dysarthria, ataxia, and difficulty in walking. An urgent head CT scan showed a region of lower density in the right cerebellar hemisphere, and the diagnosis of cerebellar edema/ischemia/infarction was set (Figure 2A). In the following hours, the patient rapidly became obtunded, could not protect his respiratory airway, and was intubated. Consequently, we inserted an intracranial pressure-monitoring catheter (ICP), escalated the dose of his antiplatelet regiment to a therapeutic dose (325 mg orally, once daily), and we transferred him to the intensive care unit (ICU).
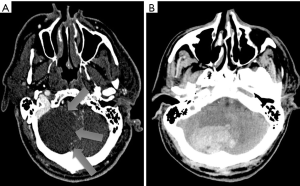
During the following two days, the ICP remained within a normal range. However, on a scheduled control head CT scan obtained at the sixth day, the dark ischemic area gave its place to an area of high density, compatible with an intracerebellar hemorrhage. The latter exerted a significant mass effect on the adjacent neural structures, obstructed the fourth ventricle, and caused acute hydrocephalus. The antiplatelet medication was withdrawn, and the patient was transferred to the operating room for an emergent decompression (Figure 2B). An external ventricular drain was placed and the posterior fossa hematoma was evacuated through a midline (asymmetric to the right side) suboccipital craniectomy.
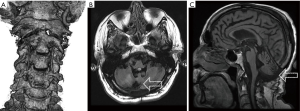
After four days of ICU hospitalization, the patient was weaned off the ventilator, and he was gradually returned to the neurosurgical ward. His cerebellar signs and symptoms remained for approximately two months after his hospital discharge to a rehabilitation center. The patient was followed-up in our outpatient clinic, initially on a monthly basis for six months, and then every six months for two years. The obtained CTA of the neck vessels showed recanalization of his right vertebral artery, while his brain MRI demonstrated right-sided cerebellar atrophy, two years after surgery (Figure 3A,B,C).
Discussion
The medical literature of the previous decades raised the global awareness for BVAIs. Our patient is among the 0.63% of all blunt trauma patients who suffer from a BVAI (1,2). In addition, he is among the 70–78% of the latter, in whom his BVAI occurs in association with a cervical spine fracture (1,2). As far as we know, he is the first reported case with a hemorrhagic transformation of a posterior fossa ischemic stroke after anti-platelet therapy for the management of a BVAI-associated ischemic stroke.
A screening for BVAI after blunt trauma should take place if there are: (I) unexplained neurological abnormalities; (II) Horner’s syndrome; (III) neck soft tissue injury; (IV) epistaxis from a suspected arterial source; (V) petrous bone fractures; (VI) brain diffuse axonal injury; (VII) cervical spine fracture through the transverse foramen; and (VIII) Le-Fort II or III facial fractures (1,2). Our patient suffered a fracture of the transverse process of two consecutive vertebrae; therefore, further angiographic evaluation of his neck vessels was mandatory. It has been postulated that CTA is the imaging modality of choice for screening patients with suspected BVAIs (4). Having said that, conventional digital subtractive angiography remains the golden standard for the diagnosis of BVAI, particularly if concurrent endovascular therapy is a potential consideration (4). Magnetic resonance imaging is reserved for those patients with a concomitant spinal cord injury (4). In the present case, we preferred a CTA study due to its non-invasive nature and its availability.
BVAIs are classified according to a five-level grading scale into grade I lesions, with luminal narrowing less than 25%, while grade II lesions are characterized by more than 25% luminal narrowing (2). Pseudo-aneurysms and total vascular occlusions are classified as grade III and grade IV lesions, respectively; grade V lesions are characterized by vessel transection with extravasation (2). The CTA of the present patient revealed the absence of visualization (total obliteration) of the right vertebral artery from the level of osseous injury. Thus, we faced a grade IV lesion.
A BVAI may cause distal posterior circulation ischemia or stroke, and anticoagulation or anti-platelet therapy is recommended (1,2,4). However, the pertinent literature has failed to demonstrate a difference in outcome between the two regiments (1,2). The majority of high-grade BVAI remains stable, while the recanalization rate of grade IV injuries has been reported as high as 35% during the initial two months after injury (3). In order to minimize the incidence of angiography-related complications, angiographic follow-up is recommended after the 7th post-injury day (1). With these in mind, we initiated a low-dose prophylactic anti-platelet therapy and we arranged for a CTA control a week later.
During the fourth day, the patient developed symptoms and signs of posterior circulation ischemia, which was verified by a head CT scan. It has been reported that BVAIs are associated with a reported stroke rate as high as 7%, which is confined to the immediate post-injury period (3). The relevant mortality is as high as 100% (3). The recommended daily doses of aspirin for the treatment of acute ischemic stroke are 160–325 mg (5). Serious bleeding complications can accompany aggressive anticoagulation regimens, either as worsening of a preexisting intra-cerebral hemorrhage or in the form of an extra-cranial hemorrhage, especially in patients with multiple injuries (1). Given the absence of a co-existing hemorrhage and the presence of a posterior fossa ischemia in our case, we administered aspirin in therapeutic doses.
In this patient, we witnessed a hemorrhagic transformation of a posterior fossa ischemic stroke secondary to a grade IV BVAI after aggressive anti-platelet therapy. It is worth noting that the hemorrhage occurred in a sedated patient without any major alterations of his vital signs or his ICP. Despite the administered anti-platelet therapy, we proceeded with suboccipital craniectomy and hematoma evacuation. The final outcome was very satisfactory, as the patient survived the acute phase, and his affected vertebral artery was gradually re-canalized during his long-term follow-up.
Conclusions
Hemorrhagic transformation after aggressive anti-platelet therapy for the treatment of BVAI is a rare but serious complication. It is difficult to suspect it in sedated or comatose patients hospitalized in ICU. It is even more difficult to surgically treat these patients, due to the administered anti-platelet therapy. Nevertheless, their timely aggressive management may well be a life-saving procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Bromberg WJ, Collier BC, Diebel LN, et al. Blunt cerebrovascular injury practice management guidelines: the Eastern Association for the Surgery of Trauma. J Trauma 2010;68:471-7. [PubMed]
- Biffl WL, Cothren CC, Moore EE, et al. Western Trauma Association Critical Decisions in Trauma: Screening for and Treatment of Blunt Cerebrovascular Injuries. J Trauma Inj Infect Crit Care 2009;67:1150-3. [Crossref] [PubMed]
- Scott WW, Sharp S, Figueroa SA, et al. Clinical and radiological outcomes following traumatic Grade 3 and 4 vertebral artery injuries: a 10-year retrospective analysis from a Level 1 trauma center. J Neurosurg 2015;122:610-5. [Crossref] [PubMed]
- Harrigan MR, Hadley MN, Dhall SS, et al. Management of vertebral artery injuries following non-penetrating cervical trauma. Neurosurgery 2013;72:234-43. [Crossref] [PubMed]
- Ansara AJ, Nisly SA, Arif SA, et al. Aspirin dosing for the prevention and treatment of ischemic stroke: An indication-specific review of the literature. Ann Pharmacother 2010;44:851-62. [Crossref] [PubMed]
Cite this article as: Brotis AG, Karagiorgas G, Tasiou A, Gatos C, Kapsalaki E, Fountas KN. Hemorrhagic transformation of posterior fossa ischemia after antithrombotic therapy for a blunt vertebral artery injury: a case report. AME Case Rep 2018;2:30.


