The surgical management of recurrent tracheal schwannoma
Introduction
Primary tracheal neoplasms (tumours) are very rare, accounting for just 1% of all tumours (1). The majority of these tumours are malignant, two histologic types make up the large majority of reported cases: squamous cell carcinoma and adenoid cystic carcinoma (2). Benign tumours of the tracheobronchial tree occur less frequently and account for about 25% of primary tracheal tumours and include tumours of neurogenic origin, specifically, schwannoma and neurofibroma (1,3). Described is a case of a successful resection of a tracheal schwannoma refractory to endoscopic treatment.
Case presentation
A 54-year-old Caucasian male, with a past medical history of well controlled asthma only, was referred to our tertiary airway reconstruction centre for evaluation of his primary tracheal schwannoma.
His initial presentation to his local hospital was symptoms of dyspnea on exertion, resulting in his evaluation and treatment included two endoscopic biopsies and laser debulking procedures 5 months apart.
Investigations
A computed tomography (CT) scan performed at his local hospital two months following his last laser procedure had demonstrated recurrent tumour involving the anterior tracheal wall with intraluminal tracheal extension.
On presentation to our institution, the patient had on laryngoscopy normal bilateral mobile and functioning vocal cords. Subsequently, under general anaesthesia a formal airway assessment was undertaken.
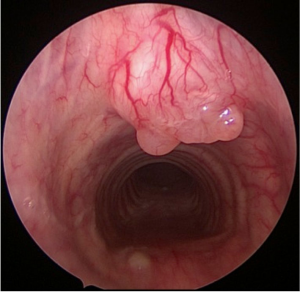
This revealed a well demarcated, exophytic tumour arising from the anterior tracheal wall. It extended from the first tracheal ring to the anterior arch of the cricoid (Figure 1). Following this evaluation the patient was offered a cricotracheal resection to excise the tumour, which was performed seven days following presentation to our institution. The potential risks were explained to the patient, which included temporary tracheostomy, change to his voice and problems with his swallow.
Treatment
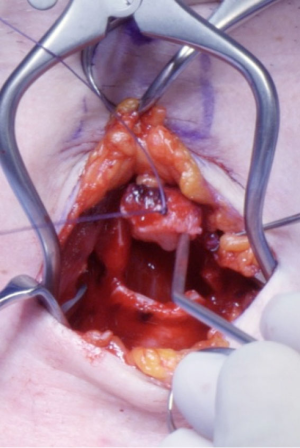
Following informed consent, the patient underwent surgery. The procedure was undertaken with the patient in supine position, neck extended with a shoulder roll. The neck was prepped and draped and a location needle was inserted through the neck under endoscopic guidance to mark the inferior margin of the tumour (Figure 2). A horizontal neck crease incision was performed. The strap muscles were dissected and the cricotracheal cartilage skeletonised (Figure 3). Using the location needle as a guide a small anterior window of cricotracheal cartilage was excised and sent for histopathology (Figure 4). Approximate macroscopic margins of 5 mm were taken. Further mobilization of the trachea was required to enable a tension free anastomosis. Primary anastomosis was performed of the trachea using interrupted polydioxanone suture (PDS) 4-0 (Figure 5). The neck was closed in layers and a small corrugated drain to prevent subcutaneous emphysema inserted. A single chin to chest suture was used to prevent hyperextension of the neck and was removed when the patient returned to the ENT ward. No covering tracheostomy was performed.
Outcome and follow up
The post-operative period was uneventful. He passed a bedside safe swallow test the following day and was discharged day 7 post operatively.
Histopathological analysis revealed a well circumscribed spindle cell tumour in the mucosa with characteristic features of schwannoma. There was no atypia or invasion. All margins were reported clear on final histopathology. Clear margins had been achieved.
Post-operatively the patient had no swallowing or voice concerns. He is currently free from recurrence as evidenced by a check bronchoscopy and CT scan one year post operatively. Results of his spirometry were also normal. He was followed up back at his referring hospital for one year post operatively and has since been discharged.
Discussion
Tracheal schwannomas are extremely rare benign tumours (4) with 52 cases reported in the literature (5). Their origin is from the peripheral nervous system and are derived from well differentiated Schwann cells. Typically, the lesions are solitary, encapsulated and attached to a nerve but have no neurites. Schwannomas are seldom associated with neurofibromatosis 1 (NF1) and rarely undergo malignant transformation (6). Tracheal schwannoma has a predilection for females and affects adults of all ages. Only a fifth of the reported cases are in paediatric patients. A recent review established that more than half the cases in the literature are reported in Asian populations followed by North American and European populations (7,8).
Tracheal schwannomas clinically are slow growing and symptoms are dependent upon their anatomical location, size and degree of airway obstruction caused by the lesion (8). Non-specific symptoms of cough and dyspnea are common and frequently attributed to respiratory disease such as asthma. Thus, patients refractory to medical therapy or those with suspect flow volume loops or those whose symptoms progress to that of stridor should be investigated promptly for an endotracheal lesion (3). Indeed, it has been reported that on average there is a 17-month delay in diagnosis following symptom onset (5). Other symptoms include haemoptysis and dysphonia.
The diagnosis of tracheal schwannoma is based on tracheobronchoscopic biopsy. Microscopically, schwannomas consist of hypercellular (Antoni A) and hypocellular (Antoni B) regions. Nuclear palisade (Verocay body) may be seen in Antoni A tissue (9). Bronchoscopy further facilitates locating the tumour and is instructive for intubation and surgery (7). CT and magnetic resonance imaging (MRI) are employed to further delineate size, site and extension. Pulmonary function tests aid early diagnosis especially flow-volume curves which demonstrate upper airway obstruction (9).
Tracheal schwannoma can be treated conservatively with endoscopic or radiological monitoring or endoscopic debulking as there may be a risk of malignant transformation (10). Small intraluminal tumours can be treated with endoscopic resection. However, the majority require an open resection for curative intent (7). A recent literature review found no recurrence in patients with clear margins following open resection. However there is a risk of recurrence with endolaryngeal procedures and annual post-operative bronchoscopic surveillance is recommended long term, as recurrence up to 12 years post resection has been reported (5). Different imaging modalities have been used for assessment of the tumour and recurrence including CT, MRI and positron emission tomography-CT (PET-CT) (8). Alternatively, serial bronchoscopies and fiberoptic tracheoscopies can be performed.
Presented is a case of a rare tracheal tumour successfully treated by open excision of a tracheal schwannoma leading to tumour free resection margins resulting in no impact on the patient’s swallowing or voice function.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Righini CA, Lequeux T, Laverierre MH, et al. Primary tracheal schwannoma: one case report and a literature review. Eur Arch Otorhinolaryngol 2005;262:157-60. [Crossref] [PubMed]
- Weber AL, Grillo HC. Tracheal tumors. A radiological, clinical, and pathological evaluation of 84 cases. Radiol Clin North Am 1978;16:227-46. [PubMed]
- Isaac BT, Christopher DJ, Thangakunam B, et al. Tracheal schwannoma: Completely resected with therapeutic bronchoscopic techniques. Lung India 2015;32:271-3. [Crossref] [PubMed]
- Girard C, Chambonnière ML, Vergnon JM. Diagnosis and treatment of a benign tracheal tumour: a schwannoma. Rev Mal Respir 2004;21:983-8. [Crossref] [PubMed]
- Hamouri S, Novotny NM. Primary tracheal schwannoma a review of a rare entity: current understanding of management and followup. J Cardiothorac Surg 2017;12:105. [Crossref] [PubMed]
- Hsu HS, Wang CY, Li WY, et al. Endotracheobronchial neurofibromas. Ann Thorac Surg 2002;74:1704-6. [Crossref] [PubMed]
- Han DP, Xiang J, Ye ZQ, et al. Primary tracheal schwannoma treated by surgical resection: a case report. J Thorac Dis 2017;9:E249-52. [Crossref] [PubMed]
- Ge X, Han F, Guan W, et al. Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature. Oncol Lett 2015;10:2273-6. [Crossref] [PubMed]
- Dorfman J, Jamison BM, Morin JE. Primary tracheal schwannoma. Ann Thorac Surg 2000;69:280-1. [Crossref] [PubMed]
- Biswas D, Marnane CN, Mal R, et al. Extracranial head and neck schwannomas--a 10-year review. Auris Nasus Larynx 2007;34:353-9. [Crossref] [PubMed]
Cite this article as: Ally M, Kinshuck AJ, Rouhani M, Sandison A, Sandhu GS. The surgical management of recurrent tracheal schwannoma. AME Case Rep 2018;2:16.