Splenic abscess following laparoscopic cholecystectomy: a case report of a rare disease and a review of its management
Introduction
Splenic abscess is a rare, potentially lethal condition, with autopsy studies showing incidence rates between 0.14–0.7%. Mortality rates ranging from 47–100% make early diagnosis and prompt intervention vital. Predisposing factors which have been identified with increased risk for splenic abscess include: metastatic hematogenous infection, hemoglobinopathies, trauma, immunodeficiency, and neighboring spleen infections (1-3).
Several case reports have documented post-surgical splenic abscess, most notably after laparoscopic sleeve gastrectomy (4,5). To the best of our knowledge, there has not been any reported cases of splenic abscess arising after laparoscopic cholecystectomy. It is important to remember this disease process for expeditious targeted treatment in future cases.
When examining the treatment options for splenic abscess, there is an increasing interest in image guided percutaneous intervention. The minimally invasive option has been shown to be a safe and efficacious alternative to surgery (6-8).
Case presentation
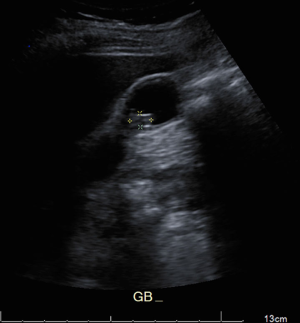
A 69-year-old female with a past medical history significant for cholelithiasis, hypertension, and hyperlipidemia presented to the Emergency Department with a chief complaint of right upper quadrant abdominal pain for two days. Upon arrival, the patient was febrile to 39.4 °C and tachycardic. Significant laboratory values included a leukocytosis, elevated liver function tests and pancreatic enzymes. Imaging was obtained demonstrating a mobile gallstone (Figure 1), choledocholithiasis and pancreatic inflammation (Figure 2). The patient was taken for urgent endoscopic retrograde cholangiopancreatography (ERCP), extraction of stones and sphincterotomy. Post procedurally, the patient underwent an uncomplicated laparoscopic cholecystectomy.

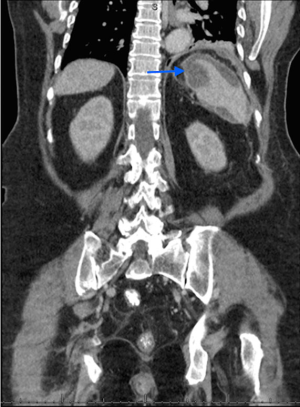
Post operatively, the patient had a persistent leukocytosis. The white blood cell count peaked at 16,800 on postoperative day 6. During this period the patient remained afebrile, hemodynamically stable, with minimal abdominal pain, and well appearing incisional wounds. She was not experiencing any upper respiratory, gastrointestinal, or genitourinary symptoms. No other lab abnormalities were noted—AST, ALT, Alk Phos, bilirubin, and lipase were all within normal limits. A CT scan was performed which showed a rim-enhancing splenic collection measuring 6.6 cm × 2.2 cm suggestive of an abscess (Figure 3).
Interventional radiology was consulted for evaluation of the abscess. A 10-french pigtail catheter was placed into the abscess with aspiration of 50 mL of purulent fluid. The fluid was sent for culture which eventually grew out Klebsiella pneumoniae and Enterobacter cloacae complex. Drain outputs were monitored over the next several days. The patient remained afebrile and hemodynamically stable, and the remainder of the hospital stay was uncomplicated.
The patient continued her course of parenteral antibiotics as an outpatient. She received imaging which confirmed resolution of the abscess (Figure 4), and the drain was removed.

Discussion
Laparoscopic cholecystectomy has become the cornerstone in treatment of symptomatic biliary colic and acute cholecystitis. The operation carries significantly lower rates of morbidity and mortality when compared to open cholecystectomy. As such, over the past several decades we have seen an increase in rates of laparoscopic cholecystectomy. However, the laparoscopic approach is not completely risk free. The most common complications seen with the procedure include bile duct injuries, hemorrhage and sub-hepatic abscess (9).
Of the many recognized complications of laparoscopic cholecystectomy, splenic abscess has not yet been reported in current literature. There have been several established risk factors for the development of splenic abscess (1-3). Of note, there has been one single case report documenting nonoperative treatment of acute cholecystitis with antibiotics with the subsequent development of splenic abscess (10).
Splenic abscess is a relatively uncommon disease with autopsy studies reporting incidence rates ranging from 0.14–0.7%. However, the disease has been growing in frequency which is likely attributed to several factors (6).
The nonspecific signs and symptoms of splenic abscess make clinical diagnosis difficult. The classic triad of fever, palpable spleen and left upper quadrant pain are only seen in about two-thirds of patients. Fever is seen in 90% of patients and leukocytosis in 88% of patients (3,10). Therefore, clinical alertness and early use of modern imaging modalities is essential for diagnosis.
CT scan has been shown to be the most sensitive test for the diagnosis of splenic abscess. It is particularly useful when the clinical picture is unclear because it carries the capability to demonstrate a variety of intra-abdominal disease processes (6,8).
Our clinical experience with the development of splenic abscess after routine laparoscopic cholecystectomy mimics cases seen in previous literature. Post operatively after uncomplicated cholecystectomy, the patient had persistent leukocytosis with uncertain etiology. The patient was not experiencing any abdominal pain and was not having fevers. Since the clinical picture was unclear, A CT scan was obtained which was able to diagnose splenic abscess (Figure 3).
Current treatment options for splenic abscess are broken down into two subsets: percutaneous and surgical intervention. Percutaneous treatment includes image guided aspiration with or without placement of drainage catheter. Surgical intervention can be either laparoscopic or open, and includes drainage of abscess with splenectomy or splenic conservation. The best treatment option remains unclear, and there is lacking prospective data demonstrating which modality is superior (1,2,5,6,8).
Recent literature review documents a 3.2% incidence of infection after splenectomy with a mortality rate of 1.4% (5). As such, there has been a drive toward spleen conserving treatment as it carries the added benefit of avoiding immunological dysfunction (6,10).
With our patient, immediate CT guided percutaneous aspiration and placement of drainage catheter was performed. Percutaneous intervention has been proven to be successful when the abscess is unilocular/bilocular, has a discrete wall, has no internal septations, or has thin liquid content (2,5,6). There has become an increasing interest in percutaneous image guided intervention as it carries several advantages. It is less invasive, has shorter procedure times, avoids general anesthesia, and is associated with earlier rehabilitation (10).
In conclusion, splenic abscess is a rare entity which is important to remember as it is associated with significant mortality. Predisposing factors have been identified, however the clinical manifestations of the disease are relatively vague. Early diagnosis and prompt treatment are essential for patient survival. Image guided percutaneous interventions have been increasingly used and carry numerous benefits compared to a more invasive surgical approach. However, there is a paucity of data comparing these therapies. As such, more prospective, randomized clinical trials are needed to analyze the efficacy of treatment options.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
References
- Chang KC, Chuah SK, Changchien CS, et al. Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan. World J Gastroenterol 2006;12:460-4. [Crossref] [PubMed]
- Kang M, Kalra N, Gulati M, et al. Image guided percutaneous splenic interventions. Eur J Radiol 2007;64:140-6. [Crossref] [PubMed]
- Singh Y, Cawich S, Aziz I, et al. Delayed splenic abscess after laparoscopic sleeve gastrectomy. BMJ Case Rep 2015. [Crossref] [PubMed]
- Sakran N, Ilivitzki A, Zeina AR, et al. Splenic abscess after sleeve gastrectomy: a report of two cases. Obes Facts 2012;5:635-9. [Crossref] [PubMed]
- Ferraioli G, Brunetti E, Gulizia R, et al. Management of splenic abscess: report on 16 cases from a single center. Int J Infect Dis 2009;13:524-30. [Crossref] [PubMed]
- Llenas-García J, Fernández-Ruiz M, Caurcel L, et al. Splenic abscess: a review of 22 cases in a single institution. Eur J Intern Med 2009;20:537-9. [Crossref] [PubMed]
- Chiang IS, Lin TJ, Chiang IC, et al. Splenic abscesses: review of 29 cases. Kaohsiung J Med Sci 2003;19:510-5. [Crossref] [PubMed]
- Smyrniotis V, Kehagias D, Voros D, et al. Splenic abscess. An old disease with new interest. Dig Surg 2000;17:354-7. [Crossref] [PubMed]
- Duca S, Bãlã O, Al-Hajjar N, et al. Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford) 2003;5:152-8. [Crossref] [PubMed]
- Harnarayan P, Naraynsingh V, Hariharan S. Splenic abscess arising from acute cholecystitis. J Coll Physicians Surg Pak 2012;22:252-4. [PubMed]
Cite this article as: Bain K, Lelchuk A, Parizh D, Meytes V, Kumar S. Splenic abscess following laparoscopic cholecystectomy: a case report of a rare disease and a review of its management. AME Case Rep 2018;2:15.


