Loculated transudative pleural effusion masquerading as right upper lobe consolidation in a haemodialysis patient
Introduction
Pleural effusion is a common encounter in renal failure patients and frequently possess a diagnostic challenge to clinician especially when it was exudative. Fortunately, transudative pleural effusion secondary to fluid overload remains the commonest cause of pleural effusion in haemodialysis patients (1). Proper clinical assessment together with chest roentograph showing bilateral pleural effusion is often capable of identifying transudative effusion in this group of patients and thoracocentesis is usually not warranted unless there are atypical features or they failed to respond to therapy (2). Moreover, frequent thoracocentesis enhance pleural inflammation and potentially complicate this challenging clinical presentation. We report an atypical presentation of a transudative pleural effusion in a case of haemodialysis patient who had a history of multiple pleural procedures.
Case presentation
A 57-year-old gentlemen with advanced diabetic nephropathy presented with recurrent bilateral pleural effusion for past two years secondary to fluid overload. This led to multiple attempts of therapeutic thoracocentesis. Haemodialysis was eventually started five months prior to current presentation but was inadequate due to poorly developed arterio-venous fistula. Dry weight was not achieved and patient remained in overloaded state most of the time. He was subsequently referred to respiratory team for opinion of bilateral pleural effusion, which was more on the right with pleural fluid analysis showing protein-discordant exudates. Medical thoracoscope subsequently revealed mildly inflamed and thickened parietal pleural. Right middle lobe was adhered to the chest wall and access to apical region was thus restricted. Parietal pleural biopsy yielded chronic inflammation. Workup for tuberculosis was negative. Patient was treated with two months of oral antimicrobial with the impression of secondarily infected pleural cavity from repeated thoracocentesis.
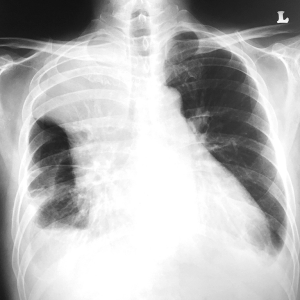
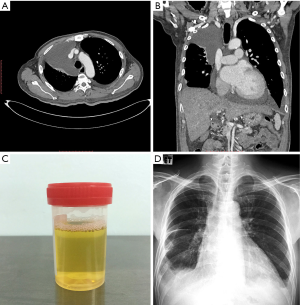
Three months later, he presented with worsening dyspnea and a new right upper lobe consolidation on chest X-ray (Figure 1). He denied fever or cough, but was still overloaded clinically. Flexible bronchoscopy demonstrated normal airway and microbiological studies were all negative. An urgent contrast enhanced computed tomography (CT) thorax was arranged and noted a loculated right apical homogeneous hypodense pleural effusion (10 Hounsfield Unit) measuring 9.4×11.3×19.4 cm (Figure 2A,B), associated with adjacent collapsed-consolidation of the apical segment of the right upper lobe. There were no calcification or mass within the effusion and no abnormal enhancement of the pleural lining. Ultrasound of the right hemithorax anterior-superiorly revealed a hypoechoeic, loculated pleural effusion with scattered fibrin strands, consistent with CT finding. Diagnostic and therapeutic thoracocentesis was performed at the second right intercoastal space, mid clavicular line under direct ultrasound guidance. 400 ml of translucent straw-colored fluid was drained (Figure 2C). Pleural fluid was transudative with pleural fluid to serum (PF/S) protein ratio of 0.42 and PF/S lactate dehydrogenase (LDH) ratio of 0.26. Patient reported immediate relieved of breathlessness post procedure and chest x-ray shown complete resolution of the right upper lobe opacity (Figure 2D). Patient subsequently underwent fistuloplasty to his arterio-venous fistula and was complied with his dialysis regimen; the pleural effusion did not recur during follow up.
Discussion
Pleural effusion is a common complaint in haemodialysis patient. Commonest cause of pleural effusion in this group of patients remains fluid overload (1). Chest roentograph and clinical findings consistent with fluid overload are often capable of identify transudative pleural effusion confidently and thoracocentesis is usually not indicated. In the contrary, if there are atypical features, further workups are usually necessary (2). However, in a series of 52 haemodialysis patients with pleural effusion, transudative pleural effusion can present unilaterally in 33.3% (1). Our patient presented clinically with fluid overload however with an atypical chest roentograph demonstrating right upper lobe collapsed-consolidation. In view of previous history of non-specific pleuritis by medical thoracoscopy and a new collapsed-consolidation, an urgent flexible bronchoscopy was performed to rule out possibility of malignant disease as 12% of non-specific pleuritis may eventually established as malignant disease (3). Fortunately bronchoscopy revealed normal airway with negative microbiological study and subsequent CT thorax reported the presence of a hypodense pleural effusion which turn out to be transudative eventually.
Although transudative pleural effusion being the commonest causes of pleural effusion in haemodialysis patients, 26.9% of still require thoracocentesis (1). Repeated therapeutic thoracocentesis should be avoided when possible and underlying problem (i.e., poorly developed arterio-venous fistula in our case) leading to the pleural effusion should be solved promptly (2). Repeated thoracocentesis leads to pleural inflammation by inducing local release of pro-inflammatory cytokine (4). This resulted in fibrin formation and loculation of pleural fluid as in our case. The medical thoracoscope finding of an adherent right middle lobe to the chest wall likely divide the right pleural cavity into two, allowing pleural fluid to be collected at the right apical region as a locule in this case.
Loculated pleural effusion masquerading as mediastinal tumour had been reported but pleural effusion that conformed to the contour of a lung lobe is rare (5,6). This case highlights the atypical but unique presentation of a transudative pleural effusion and demonstrates the risk of repeated thoracocentesis complicating a simple clinical presentation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Bakirci T, Sasak G, Ozturk S, et al. Pleural effusion in long-term hemodialysis patients. Transplant Proc 2007;39:889-91. [Crossref] [PubMed]
- Hooper C, Lee YC, Maskell N, et al. Investigation of a unilateral pleural effusion in adults: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65 Suppl 2:ii4-17. [Crossref] [PubMed]
- Davies HE, Nicholso JE, Rahman NM, et al. Outcome of patients with nonspecific pleuritis/fibrosis on thoracoscopic pleural biopsies. Eur J Cardiothorac Surg 2010;38:472-7. [Crossref] [PubMed]
- Chung CL, Chen YC, Chang SC. Effect of repeated thoracenteses on fluid characteristics, cytokines, and fibrinolytic activity in malignant pleural effusion. Chest 2003;123:1188-95. [Crossref] [PubMed]
- Storey CF. Encapsulated pleural effusion simulating mediastinal tumour. Radiology 1952;58:408-14. [Crossref] [PubMed]
- Mohapatra PR, Garg K, Prashanth C, et al. Pleural effusion presenting as mediastinal widening. Lung India 2013;30:354-6. [Crossref] [PubMed]
Cite this article as: Kho SS, Tay PS, Lee J, Tie ST. Loculated transudative pleural effusion masquerading as right upper lobe consolidation in a haemodialysis patient. AME Case Rep 2017;1:4.